Osseointegration
Osseointegration derives from the Greek osteon, bone, and the Latin integrare, to make whole. The term refers to the direct structural and functional connection between living bone and the surface of a load-bearing artificial implant. Osseointegration has enhanced the science of medical bone and joint replacement techniques as well as dental implants and improving prosthetics for amputees.
Definition
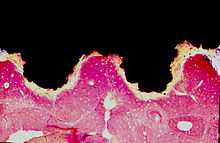
Osseointegration is also defined as: "the formation of a direct interface between an implant and bone, without intervening soft tissue".[1] Osseointegrated implant is a type of implant defined as "an endosteal implant containing pores into which osteoblasts and supporting connective tissue can migrate".[2] Applied to oral implantology, this thus refers to bone grown right up to the implant surface without interposed soft tissue layer. No scar tissue, cartilage or ligament fibers are present between the bone and implant surface. The direct contact of bone and implant surface can be verified microscopically.
Osseointegration may also be defined as :
- Osseous integration, the apparent direct attachment or connection of osseous tissue to an inert alloplastic material without intervening connective tissue.
- The process and resultant apparent direct connection of the endogenous material surface and the host bone tissues without intervening connective tissue.
- The interface between alloplastic material and bone.
History
Osseointegration was first observed—albeit not explicitly stated—by Bothe, Beaton, and Davenport in 1940.[3][4] Bothe et al. were the first researchers to implant titanium in an animal and remarked how it had the tendency to fuse with bone.[3][4] Bothe et al. reported that due to the elemental nature of the titanium, its strength, and its hardness, it had great potential to be used as future prosthesis material.[3][4] Osseointegration was later described by Gottlieb Leventhal in 1951.[3][5] Leventhal placed titanium screws in rat femurs and remarked how "At the end of 6 weeks, the screws were slightly tighter than when originally put in; at 12 weeks, the screws were more difficult to remove; and at the end of 16 weeks, the screws were so tight that in one specimen the femur was fractured when an attempt was made to remove the screw. Microscopic examinations of the bone structure revealed no reaction to the implants. The trabeculation appeared to be perfectly normal."[3][5] The reactions described by Leventhal and Bothe et al. would later be coined into the term "osseointegration" by Per-Ingvar Brånemark. In 1952, Per-Ingvar Brånemark of Sweden conducted an experiment where he utilized a titanium implant chamber to study blood flow in rabbit bone. At the conclusion of the experiment, when it became time to remove the titanium chambers from the bone, he discovered that the bone had integrated so completely with the implant that the chamber could not be removed. Brånemark called this "osseointegration," and, like Bothe et al. and Leventhal before him, saw the possibilities for human use.[3][4][5]
In dental medicine the implementation of osseointegration started in the mid-1960s as a result of Brånemark's work.[6][7][8][9] In 1965 Brånemark, who was at the time Professor of Anatomy at the University of Gothenburg, placed dental implants into the first human patient - Gösta Larsson. This patient had a cleft palate defect and required implants to support a palatal obturator. Gosta Larsson died in 2005, with the original implants still in place after 40 years of function.[10]
In the mid-1970s Brånemark entered into a commercial partnership with the Swedish defense company Bofors to manufacture dental implants and the instrumentation required for their placement. Eventually an offshoot of Bofors, Nobel Pharma, was created to concentrate on this product line. Nobel Pharma subsequently became Nobel Biocare.[10]
Brånemark spent almost 30 years fighting the scientific community for acceptance of osseointegration as a viable treatment. In Sweden he was often openly ridiculed at scientific conferences. His university stopped funding for his research, forcing him to open a private clinic to continue the treatment of patients. Eventually an emerging breed of young academics started to notice the work being performed in Sweden. Toronto's Professor Zarb, a Maltese dentist working in Canada, was instrumental in bringing the concept of osseointegration to the wider world. The 1983 Toronto Conference is generally considered to be the turning point, when finally the worldwide scientific community accepted Brånemark's work. Today osseointegration is a highly predictable and commonplace treatment modality.[10]
Mechanism of osseointegration
Osseointegration is a dynamic process in which characteristics of the implant (i.e. macrogeometry, surface properties, etc.) play a role in modulating molecular and cellular behavior. While osseointegration has been observed using different materials, it is most often used to describe the reaction of bone tissues to titanium, or titanium coated with calcium phosphate derivatives.[11] It was previously thought that titanium implants were retained in bone through the action of mechanical stabilization or interfacial bonding. Alternatively, calcium phosphate coated implants were thought to be stabilized via chemical bonding. It is now known that both calcium phosphate coated implants and titanium implants are stabilized chemically with bone, either through direct contact between calcium and titanium atoms, or by the bonding to a cement line-like layer at the implant/bone interface.[12][13] While there are some differences (e.g. like the lack of chondrogenic progenitors), osseointegration occurs through the same mechanisms as bone fracture healing.[14][15]
Technique
For osseointegrated dental implants, metallic, ceramic, and polymeric materials have been used,[2] in particular titanium.[16] To be termed osseointegration the connection between the bone and the implant need not be 100 percent, and the essence of osseointegration derives more from the stability of the fixation than the degree of contact in histologic terms. In short it represents a process whereby clinically asymptomatic rigid fixation of alloplastic materials is achieved, and maintained, in bone during functional loading.[17] Implant healing times and initial stability are a function of implant characteristics. For example, implants utilizing a screw-root form design achieve high initial mechanical stability through the action of their screws against the bone. Following placement of the implant, healing typically takes several weeks or months before the implant is fully integrated into the surrounding bone. First evidence of integration occurs after a few weeks, while more robust connection is progressively effected over the next months or years.[18] Implants that possess a screw-root form design result in bone resorption followed by interfacial bone remodeling and growth around the implant.[19]
Implants utilizing a plateau-root form design (or screw-root form implants with a wide enough gap between the pitch of the screws) undergo a different mode of peri-implant ossification. Unlike the aforementioned screw-root form implants, plateau-root form implants exhibit de novo bone formation on the implant surface.[20] The type of bone healing exhibited by plateau-root form implants is known as intramembranous-like healing.[19]
Though the osseointegrated interface becomes resistant to external shocks over time, it may be damaged by prolonged adverse stimuli and overload, which may result in implant failure.[21][22] In studies performed using "Mini dental implants," it was noted that the absence of micromotion at the bone-implant interface was necessary to enable proper osseointegration.[23] Further, it was noted that there is a critical threshold of micromotion above which a fibrous encapsulation process occurs, rather than osseointegration.[24]
Other complications may arise even in the absence of external impact. One issue is the growing of cement.[25] In normal cases, the absence of cementum on the implant surface prevents the attachment of collagen fibers. This is normally the case due to the absence of cementum progenitor cells in the area receiving the implant. However, when such cells are present, cement may form on or around the implant surface, and a functional collagen attachment may attach to it.[26]
Advances in materials engineering: metal foams
Since 2005, a number of orthopedic device manufacturers have introduced products that feature porous metal construction.[27][28][29] Clinical studies on mammals have shown that porous metals, such as titanium foam, may allow the formation of vascular systems within the porous area.[30] For orthopedic uses, metals such as tantalum or titanium are often used, as these metals exhibit high tensile strength and corrosion resistance with excellent biocompatibility.
The process of osseointegration in metal foams is similar to that in bone grafts. The porous bone-like properties of the metal foam contribute to extensive bone infiltration, allowing osteoblast activity to take place. In addition, the porous structure allows for soft tissue adherence and vascularization within the implant. These materials are currently deployed in hip replacement, knee replacement and dental implant surgeries.
Applications
- Dental implants are by far the main field of application
- Retention of a craniofacial prosthesis such as an artificial ear (ear prosthesis), maxillofacial reconstruction, eye (orbital prosthesis), or nose (nose prosthesis)
- Bone anchored limb prostheses[31]
- Bone anchored hearing conduction amplification (Bone anchored hearing aid)
- Eyeborg perceive color through sound waves
- Knee and joint replacement
See also
- Osseoincorporation
- Abutment (dentistry)
- Dental implant
- Periodontology
- Oral and maxillofacial surgery
- Oral Surgery
- Prosthesis
- Dentistry
- European Association for Osseointegration
- British Society of Oral Implantology
- The Osseointegration Group of Australia
Notes and references
- ↑ Miller, Benjamin F.; Keane, Claire B. (1992). Miller-Keane Encyclopedia & Dictionary of Medicine, Nursing, and Allied Health. Philadelphia: Saunders. ISBN 0-7216-3456-7.
- ↑ 2.0 2.1 Mosby's Medical, Nursing & Allied Health Dictionary. St. Louis: Mosby. 2002. p. 1240. ISBN 0-323-01430-5.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Rudy, Robert; Levi, Paul A; Bonacci, Fred J; Weisgold, Arnold S; Engler-Hamm, Daniel (2008). "Intraosseous anchorage of dental prostheses: an early 20th century contribution.". Compend Contin Educ Dent 29 (4): 220–229. PMID 18524206.
- ↑ 4.0 4.1 4.2 4.3 Bothe, RT; Beaton, KE; Davenport, HA (1940). "Reaction of bone to multiple metallic implants.". Surg Gynecol Obstet 71: 598–602.
- ↑ 5.0 5.1 5.2 Leventhal, Gottlieb (1951). "Titanium, a metal for surgery". J Bone Joint Surg Am 33–A (2): 473–474. PMID 14824196.
- ↑ Brånemark PI (September 1983). "Osseointegration and its experimental background". The Journal of Prosthetic Dentistry 50 (3): 399–410. doi:10.1016/S0022-3913(83)80101-2. PMID 6352924.
- ↑ Brånemark, Per-Ingvar; Zarb, George Albert; Albrektsson, Tomas (1985). Tissue-integrated prostheses: osseointegration in clinical dentistry. Chicago: Quintessence. ISBN 978-0-86715-129-9.
- ↑ Albrektsson, Tomas; Zarb, George A. (1989). The Branemark osseointegrated implant. Chicago: Quintessence Pub. Co. ISBN 978-0-86715-208-1.
- ↑ Beumer, John; Lewis, Steven (1989). The Branemark implant system: clinical and laboratory procedures. St. Louis: Ishiyaku EuroAmerica. ISBN 0-912791-62-4.
- ↑ 10.0 10.1 10.2 Close to the Edge - Brånemark and the Development of Osseointegration, edited by Elaine McClarence, Quintessence 2003.
- ↑ Albrektsson, T; Johansson, C (2001). "Osteoinduction, osteoconduction and osseointegration". Eur Spine J 10 (2): 596–510. doi:10.1007/s005860100282.
- ↑ Davies, J (2003). "Understanding peri-implant endosseous healing.". J Dent Ed 67 (8): 932–949.
- ↑ Thuvander, M; Andersson, M (2014). "Atomically resolved tissue integration.". Nano Lett 14 (8): 4220–4223. doi:10.1021/nl501564f. PMID 24989063.
- ↑ Colnot, C; Romero, DM; Huang, S; Rahman, J; Currey, JA; Nanci, A; Brunski, JB; Helms, JA (2007). "Molecular analysis of healing at a bone-implant interface.". J Dent Res 86 (9): 109–118. PMID 17720856.
- ↑ Albrektsson, T; Branemark, PI; Hansson, HA; Lindstrom, J (1981). "Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to- implant anchorage in man". Acta Orthop Scand. 52 (2): 155–170. doi:10.3109/17453678108991776. PMID 7246093.
- ↑ Natali, Arturo N., ed. (2003). Dental biomechanics. Washington, DC: Taylor & Francis. pp. 69–87. ISBN 978-0-415-30666-9.
- ↑ Zarb, George A.; Albrektsson, Tomas (1991). "Osseointegration: A requiem for the periodontal ligament?". International Journal of Periodontology and Restorative Dentistry (11): 88–91.
- ↑ Albrektsson, Tomas; Berglundh, Tord; Lindhe, Jan (2003). "Osseointegration: Historic Background and Current Concepts". In Lindhe, Jan; Karring, Thorkild; Lang, Niklaus P. Clinical Periodontology and Implant Dentistry. Oxford: Blackwell Munksgaard. p. 815. ISBN 1-4051-0236-5.
- ↑ 19.0 19.1 Coelho, P; Jimbo, R (2014). "Osseointegration of metallic devices: current trends based on implant hardware design.". Arch Biochem Biophys 561: 99–108. doi:10.1016/j.abb.2014.06.033. PMID 25010447.
- ↑ Berglundh, T; Abrahamsson, I; Lang, N; Lindhe, J (2003). "De novo alveolar bone formation adjacent to endosseous implants.". Clin. Oral Impl. Res. 14 (3): 251–262. doi:10.1034/j.1600-0501.2003.00972.x. PMID 12755774.
- ↑ Albrektsson, Tomas; Berglundh, Tord; Lindhe, Jan (2003). "Osseointegration: Historic Background and Current Concepts". In Lindhe, Jan; Karring, Thorkild; Lang, Niklaus P. Clinical Periodontology and Implant Dentistry. Oxford: Blackwell Munksgaard. p. 816. ISBN 1-4051-0236-5.
- ↑ Isidor F (June 1996). "Loss of osseointegration caused by occlusal load of oral implants. A clinical and radiographic study in monkeys". Clinical Oral Implants Research 7 (2): 143–52. doi:10.1034/j.1600-0501.1996.070208.x. PMID 9002833.
- ↑ Brunski JB (June 1999). "In vivo bone response to biomechanical loading at the bone/dental-implant interface". Advances in Dental Research 13: 99–119. doi:10.1177/08959374990130012301. PMID 11276755.
- ↑ Szmukler-Moncler S, Salama H, Reingewirtz Y, Dubruille JH (1998). "Timing of loading and effect of micromotion on bone-dental implant interface: review of experimental literature". Journal of Biomedical Materials Research 43 (2): 192–203. doi:10.1002/(SICI)1097-4636(199822)43:2<192::AID-JBM14>3.0.CO;2-K. PMID 9619438.
- ↑ Pauletto N, Lahiffe BJ, Walton JN (1999). "Complications associated with excess cement around crowns on osseointegrated implants: a clinical report". The International Journal of Oral & Maxillofacial Implants 14 (6): 865–8. PMID 10612925.
- ↑ Bernard, George W.; Carranza, Ferritin A.; Jovanovic, Sascha A. (1996). "Biologic Aspects of Dental Implants". In Carranza, Fermín A.; Newman, Michael G. Clinical Periodontology. pp. 685–9. ISBN 978-0-7216-6728-7.
- ↑ Biomet Orthopedics, Regenerex® Porous Titanium Construct, http://www.biomet.com/orthopedics/productDetail.cfm?category=2&product=231
- ↑ Zimmer Orthopedics, Trabeluar Metal Technology, http://www.zimmer.com/ctl?template=CP&op=global&action=1&id=33
- ↑ Zimmer Cancellous-Structured Titanium Porous Coating, http://www.zimmer.com/ctl?op=global&action=1&id=7876&template=MP
- ↑ Osseointegration with Titanium Foam in Rabbit Femur, YouTube: http://www.youtube.com/watch?v=hdscnna5r1Q
- ↑ Hagberg K, Brånemark R (2009). "One hundred patients treated with osseointegrated transfemoral amputation prostheses--rehabilitation perspective". Journal of Rehabilitation Research and Development 46 (3): 331–44. PMID 19675986.
23. Trabecular Metal Material: The Next Best Thing to BoneTM: http://www.trabecularmetal.zimmerdental.com/Implant/imp_home.aspx
Further reading
- Zarb GA, Schmitt A (July 1990). "The longitudinal clinical effectiveness of osseointegrated dental implants: the Toronto Study. Part II: The prosthetic results". The Journal of Prosthetic Dentistry 64 (1): 53–61. doi:10.1016/0022-3913(90)90153-4. PMID 2200880.
- Apse P, Zarb GA, Schmitt A, Lewis DW (1991). "The longitudinal effectiveness of osseointegrated dental implants. The Toronto Study: peri-implant mucosal response". The International Journal of Periodontics & Restorative Dentistry 11 (2): 94–111. PMID 1718917.
- Chaytor DV, Zarb GA, Schmitt A, Lewis DW (1991). "The longitudinal effectiveness of osseointegrated dental implants. The Toronto Study: bone level changes". The International Journal of Periodontics & Restorative Dentistry 11 (2): 112–25. PMID 1938184.
- Barber AJ, Butterworth CJ, Rogers SN (January 2010). "Systematic review of primary osseointegrated dental implants in head and neck oncology". The British Journal of Oral & Maxillofacial Surgery 49 (1): 29–36. doi:10.1016/j.bjoms.2009.12.007. PMID 20079957.
- Hultin M, Gustafsson A, Klinge B (February 2000). "Long-term evaluation of osseointegrated dental implants in the treatment of partly edentulous patients". Journal of Clinical Periodontology 27 (2): 128–33. doi:10.1034/j.1600-051x.2000.027002128.x. PMID 10703659.
- Olivé, Jordi; Aparicio, Carlos (1990). "The periotest implant as a measure of osseointegrated oral implant stability". The International Journal of Oral & Maxillofacial Implants 5 (4): 390–400.
- Holmgren EP, Seckinger RJ, Kilgren LM, Mante F (1998). "Evaluating parameters of osseointegrated dental implants using finite element analysis--a two-dimensional comparative study examining the effects of implant diameter, implant shape, and load direction". The Journal of Oral Implantology 24 (2): 80–8. doi:10.1563/1548-1336(1998)024<0080:EPOODI>2.3.CO;2. PMID 9835834.
External links
| ||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||