Oculopharyngeal muscular dystrophy
| Oculopharyngeal muscular dystrophy | |
|---|---|
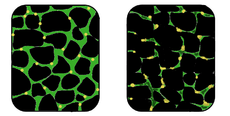 In affected muscle (right) the tissue becomes disorganized and the concentration of dystrophin (green) is greatly reduced, compared to normal muscle (left). | |
| Classification and external resources | |
| ICD-10 | G71.0 |
| ICD-9 | 359.1 |
| OMIM | 164300 |
| DiseasesDB | 29869 |
| MeSH | D039141 |
| GeneReviews | |
Oculopharyngeal muscular dystrophy (OPMD) can be autosomal dominant[1] neuromuscular disease or autosomal recessive which appears in early middle age (fifth decade).[2] The most common inheritance of OPMD is autosomal dominant, which means only one copy of the mutated gene needs to be present in each cell. Children of an affected parent have a 50% chance of inheriting the mutant gene. Generally, autosomal dominant inheritance have a strong family tie. Less commonly, OPMD can be inherited in an autosomal recessive pattern, which means that two copies of the mutated gene need to be present in each cell, both parents need to be carriers of the mutated gene, and usually show no signs or symptoms. The PABPN1 mutation contains a GCG trinucleotide repeat at the 5' end of the coding region, and expansion of this repeat from the normal 6 copies to 8-13 copies which then leads to autosomal dominant oculopharyngeal muscular dystrophy (OPMD) disease.[3]
Signs and symptoms
Progressive ptosis (drooping of eyelids) and weakness of the extraocular muscles is the initial clinical finding.. Dysphagia (difficulty swallowing) the swallowing difficulties begin with food but as the condition worsens liquids become difficult to swallow as well. Atrophy (weakness and wasting of the tongue). Problems taking in food can lead to malnutrition.
Proximal limb weakness develops later on in the disease, and usually occurs near the center of the body, particularly muscles in the upper legs and hips. This condition progresses slowly over time and individuals may need assistance of a cane or walker, but rarely will they need a wheelchair.[2][3]
Diagnosis
A muscle biopsy used to be the only method to diagnose the condition. Today a simple blood draw with genetic testing for GCG trinucleotide expansions in the PABPN1 gene is more common. A distinction between OPMD and myasthenia gravis or mitochondrial myopathy must be made. The absence of family history and the fluctuation of symptoms in myasthenia gravis usually distinguish the two conditions.[4]
Treatment
The condition does not generally reduce lifespan and there is no specific treatment, but there are many ways to help manage symptoms. A consistent diet planned with the help of a dietitian along with exercises taught by a speech therapist can assist with mild symptoms of dysphagia. Some surgeries are available that can reduce ptosis and dysphagia. . Cutting one of the throat muscles internally, an operation called cricopharyngeal myotomy, can be one way to ease symptoms in more severe cases. An individual can also have a balloon inflated to dilate the gullet. Physical therapy and specifically designed exercises may assist with proximal limb weakness, though there is still no current definitive data showing it will stop the progress of the disease. With all surgical procedures, they come with many risk factors and the choice for treatment depends upon the individual and their needs.[5][6]
Epidemiology
The disease is found across 5 continents and is frequently seen in French Canadians, with a prevalence 1:1000. It has also been seen in a population of Hispanic Americans in New Mexico. A 1997 study from Israel showed the second largest cluster of known individuals are of Bukhara Jews from Uzbekistan, with a calculated minimal prevalence of 1:600.[7]
References
- ↑ Davies Je, B. Z.; Berger, Z.; Rubinsztein, D. C. (February 2006). "Oculopharyngeal muscular dystrophy: Potential therapies for an aggregate-associated disorder". The International Journal of Biochemistry & Cell Biology 38 (9): 1457–1462. doi:10.1016/j.biocel.2006.01.016. PMID 16530457.
- ↑ 2.0 2.1 Brais B, Bouchard JP, Xie YG et al. (Feb 1998). "Short GCG expansions in the PABP2 gene cause oculopharyngeal muscular dystrophy". Nat. Genet. 18 (2): 164–7. doi:10.1038/ng0298-164. PMID 9462747.
- ↑ 3.0 3.1 http://www.ncbi.nlm.nih.gov/gene/8106 "PABPN1 poly(A) binding protein, nuclear 1 [ Homo sapiens (human) ]"]11 OCT 2014.
- ↑ GeneReviews/NCBI/NIH/UW entry on Oculopharyngeal Muscular Dystrophy
- ↑ Dr D.Hilton-Jones. "Types of muscle diseases", "Muscular Dystrophy Campaign," January, 2006
- ↑ Brais, B (January 2009). "Oculopharyngeal muscular dystrophy: a polyalanine myopathy.". Current neurology and neuroscience reports 9 (1): 76–82. doi:10.1007/s11910-009-0012-y. PMID 19080757.
- ↑ Blumen SC, Nisipeanu P, Sadeh M et al. (October 1997). "Epidemiology and inheritance of oculopharyngeal muscular dystrophy in Israel". Neuromuscul. Disord. 7 (Suppl 1): S38–40. doi:10.1016/s0960-8966(97)00080-1. PMID 9392014.
External links
- opmd at NIH/UW GeneTests
- Muscular Dystrophy Association's website in Greece
- Oculopharyngeal muscular dystrophy at NIH's Office of Rare Diseases
- GeneReviews Washington State University, funded by NIH
| ||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||