Mitral valve
| Mitral valve | |
|---|---|
.svg.png)
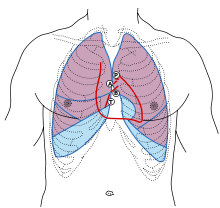
 Anterior (frontal) view of the opened heart. White arrows indicate normal blood flow. (Mitral valve labeled at center right.) | |
 Base of ventricles exposed by removal of the atria. (Bicuspid (mitral) valve visible at bottom left.) | |
| Details | |
| Latin |
Valva atrioventricularis sinistra, valva mitralis |
| Identifiers | |
| Gray's | p.534 |
| MeSH | A07.541.510.507 |
| Dorlands /Elsevier | 12843904 |
| TA | A12.1.04.003 |
| FMA | 7235 |
| Anatomical terminology | |
The mitral valve (also known as the bicuspid valve or left atrioventricular valve) is a dual-flap (bi- from the Latin, meaning double, and mitral- from the Latin, meaning shaped like a mitre) valve in the heart that lies between the left atrium (LA) and the left ventricle (LV). The mitral valve (not to be confused with the congenital bicuspid aortic valve) and the tricuspid valve are known collectively as the atrioventricular valves because they lie between the atria and the ventricles of the heart and control the flow of blood.
During diastole, a normally-functioning mitral valve opens as a result of increased pressure from the left atrium as it fills with blood (preloading). As atrial pressure increases above that of the left ventricle, the mitral valve opens. Opening facilitates the passive flow of blood into the left ventricle. Diastole ends with atrial contraction, which ejects the final 20% of blood that is transferred from the left atrium to the left ventricle. This amount of blood is known as end-diastolic volume (EDV), and the mitral valve closes at the end of atrial contraction to prevent a reversal of blood flow.
Structure

The mitral valve is typically 4–6 cm² in area. It has two cusps, or leaflets, (the anteromedial leaflet and the posterolateral leaflet) that guard the opening. The opening is surrounded by a fibrous ring known as the mitral valve annulus. (The orientation of the two leaflets resemble a bishop's mitre, whence the valve receives its name.[1]) The anterior cusp protects approximately two-thirds of the valve (imagine a crescent moon within the circle, where the crescent represents the posterior cusp). Note that although the anterior leaflet takes up a larger part of the ring and rises higher, the posterior leaflet has a larger surface area. These valve leaflets are prevented from prolapsing into the left atrium by the action of tendons attached to the posterior surface of the valve, chordae tendineae.
The inelastic chordae tendineae are attached at one end to the papillary muscles and the other to the valve cusps. Papillary muscles are fingerlike projections from the wall of the left ventricle. Chordae tendineae from each muscle are attached to both leaflets of the mitral valve. Thus, when the left ventricle contracts, the intraventricular pressure forces the valve to close, while the tendons keep the leaflets coapting together and prevent the valve from opening in the wrong direction (thus preventing blood to flow back to the left atrium). Each chord has a different thickness. The thinnest ones are attached to the free leaflet margin, whereas thickest ones (strut chords) are attached quite away from the free margin. This disposition has important effects on systolic stress distribution physiology [2]
Function
During left ventricular diastole, after the pressure drops in the left ventricle due to relaxation of the ventricular myocardium, the mitral valve opens, and blood travels from the left atrium to the left ventricle. About 70 to 80% of the blood that travels across the mitral valve occurs during the early filling phase of the left ventricle. This early filling phase is due to active relaxation of the ventricular myocardium, causing a pressure gradient that allows a rapid flow of blood from the left atrium, across the mitral valve. This early filling across the mitral valve is seen on doppler echocardiography of the mitral valve as the E wave.
After the E wave, there is a period of slow filling of the ventricle.
Left atrial contraction (left atrial systole) (during left ventricular diastole) causes added blood to flow across the mitral valve immediately before left ventricular systole. This late flow across the open mitral valve is seen on doppler echocardiography of the mitral valve as the A wave. The late filling of the LV contributes about 20% to the volume in the left ventricle prior to ventricular systole, and is known as the atrial kick.
The mitral annulus changes in shape and size during the cardiac cycle. It is smaller at the end of atrial systole due to the contraction of the left atrium around it, like a sphincter. This reduction in annulus size at the end of atrial systole may be important for the proper coapting of the leaflets of the mitral valve when the left ventricle contracts and pumps blood.[3] Leaking valves can be corrected by mitral valve annuloplasty, a common surgical procedure that aims at restoring proper leaflet coaptation.
Clinical significance
The closing of the mitral valve and the tricuspid valve constitutes the first heart sound (S1). It is not the valve closure itself which produces the sound but the sudden cessation of blood flow, when the mitral and tricuspid valves close.
There are some valvular heart diseases that affect the mitral valve. Mitral stenosis is a narrowing of the valve. This can be heard as an opening snap in a heart sound which is not normally present.
Classic mitral valve prolapse is caused by an excess of connective tissue that thickens the spongiosa layer of the cusp and separates collagen bundles in the fibrosa. This weakens the cusps and adjacent tissue, resulting in an increased cuspal area and lengthening of the chordae tendineae. Elongation of the chordae tendineae often causes rupture, commonly to the chordae attached to the posterior cusp. Advanced lesions—also commonly involving the posterior leaflet—lead to leaflet folding, inversion, and displacement toward the left atrium.[4]
A valve prolapse can result in mitral insufficiency which is a regurgitation or backflow of blood due to the incomplete closure of the valve. Surgery can be performed to replace or repair a damaged valve. A less invasive method is that of mitral valvuloplasty which uses a balloon catheter to open up a stenotic valve.
Additional images
-

Section of the heart showing the ventricular septum. (Bicuspid valve visible at center.)
-

Apical view of valves
-

Cross-sectional view of mitral valve between left atrium (upper chamber) and left ventricle (lower chamber), which shows parts of walls of left atrium and left ventricle that are next to the mitral valve.
-

Mitral valve
-

Mitral valve
See also
- Infective endocarditis
- The mitral valve is the most common site of native-valve endocarditis.
- Infective endocarditis
References
- ↑ mitral valve, Stedman's Online Medical Dictionary at Lippincott Williams and Wilkins
- ↑ Nazari S, Carli F, Salvi S et al. (Apr 2000). "Patterns of systolic stress distribution on mitral valve anterior leaflet chordal apparatus. A structural mechanical theoretical analysis". J Cardiovasc Surg (Torino) 41 (2): 193–202. PMID 10901521.
- ↑ Pai RG, Varadarajan P, Tanimoto M (2003). "Effect of atrial fibrillation on the dynamics of mitral annular area". The Journal of Heart Valve Disease 12 (1): 31–7. PMID 12578332. Retrieved 2010-03-04.
- ↑ Playford, David; Weyman, Arthur (2001). "Mitral valve prolapse: time for a fresh look". Reviews in Cardiovascular Medicine 2 (2): 73–81. PMID 12439384.
External links
- Anatomy figure: 20:07-03 at Human Anatomy Online, SUNY Downstate Medical Center — "Valves of the heart"
- Mitral Valve Repair at The Mount Sinai Hospital — "Mitral Valve Function"
- Surgical Anatomy of the Mitral Valve at echoincontext.com
- Mitral Valve Repair at Englewood Hospital and Medical Center — Mitral valve repair
- Mitral Valve Surgery reference site
- Cardiac Valve Animations - Perioperative Interactive Education Group — Cardiac valve animations
- Mitral Valve Patient Learning Center
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||