Melarsoprol
 | |
 | |
| Systematic (IUPAC) name | |
|---|---|
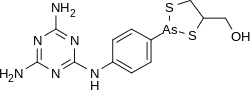
|
(2-(4-(4,6-diamino-1,3,5-triazin-2-ylamino)phenyl)- 1,3,2-dithiarsolan-4-yl)methanol | |
| Clinical data | |
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| |
| |
| IV | |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half-life | 35 hours |
| Excretion | Renal |
| Identifiers | |
|
494-79-1 | |
| P01CD01 QP51AD04 | |
| PubChem | CID 10311 |
| ChemSpider |
9889 |
| UNII |
ZF3786Q2E8 |
| KEGG |
D00832 |
| ChEMBL |
CHEMBL166 |
| Chemical data | |
| Formula | C12H15AsN6OS2 |
| 398.341 g/mol | |
|
SMILES
| |
| |
| | |
Melarsoprol (INN) is a prodrug used in the treatment of East African (rhodesiense) human African trypanosomiasis.[1] It is produced by Sanofi-Aventis and is on the World Health Organization's List of Essential Medicines.[2]
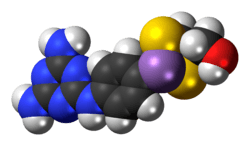
Freidheim demonstrated in 1949 the effects of melarsoprol against late-state trypanosomiasis. Melarsoprol is the dimercaptopropanol derivative of melarsen oxide (Mel Ox), whose structure is shown below:[3]
The main drug prescribed is Mel B, however, an alarming number of side effects occur from treatment. The active metabolite of Mel B is Mel Ox, which is taken up by the TbAT1 adenosine transporter in T. brucei brucei.[4] Due to side effects similar to arsenic poisoning, other pharmacological agents have become first-line treatments for stage one of the disease and for certain trypanosomes.
Treatment
All people with confirmed trypanosome-caused disease must be treated. Treatment differs based on whether disease levels are considered stage 1 or stage 2 and based on which specific trypanosome has infected a patient. Below are treatment options (all adapted from [5]).
Melasarprol is used in the treatment of the second stage of the disease, and is the only treatment available for late-stage T. b. rhodesiense treatment.[6]
Mechanism of action
Melarsoprol is a prodrug, which is metabolized to melarsen oxide (Mel Ox) as its active form. Mel Ox is an arsen-oxide which irreversibly binds to vicinal sulfhydryl groups causing the inactivation of enzymes. The inability to distinguish between host and parasites renders this drug highly toxic with many side effects.
Mel Ox reacts with trypanothione (a spermidine-glutathione adduct which replaces glutathione in trypanosomes). Binding to this adduct forms a melarsen oxide-trypanothione adduct (Mel T) which competitively inhibits trypanothione reductase, effectively killing the parasitic cell.[3]
Dosage
Two arsenic-containing stereoisomers exist in a 3:1 molar ratio. As melarsarprol is insoluble in water, dosage occurs via a 3.6% propylene glycol intravenous injection.[3]
Pharmacokinetics
The half-life of melarsoprol is less than 1 hour, but bioassays indicate a 35-hour half-life. This is indicative of pharmacologic agents with active metabolites. One such metabolite, Mel Ox, reaches maximum plasma levels about 15 minutes after melarsoprol injection. Clearance is at 21.5 ml/min/kg and Mel Ox half-life is 3.9 hours.[7]
Failure Rates & Resistance
Failure rates of 20-27% in certain African countries have been reported. These are linked to both drug resistance and other mechanisms which have not yet been elucidated. Resistance is likely due to transport problems associated with the P2 transporter, an adenine-adenosine transporter. Resistance can occur with point mutations within this transporter.[3]
Therapeutic uses
Due to high toxicity, melarsarprol is reserved only for the most dangerous of cases - stage 2 infection. Other agents with lower toxicity are used in stage 1.[1] The 2009 approval of nifurtimoxeflornithine combination therapy (NECT) for the treatment of T. b. gambiense served to limit merlarsoprol to the treatment of second-stage T. b. rhodesiense solely.[8]
Side effects
Being a toxic organic compound of arsenic, melarsoprol is a highly dangerous treatment which is only administered by injection under the supervision of a physician, as it can produce similar effects as arsenic poisoning. Among clinicians, it is colloquially referred to as "arsenic in antifreeze".[9] It is known to cause a range of side effects including convulsions, fever, loss of consciousness, rashes, bloody stools, nausea, and vomiting. It causes encephalopathy in 5–10% of cases, of which 40% die.[10]
References
- ↑ 1.0 1.1 Bisser S; N'Siesi FX; Lejon V et al. (2007). "Equivalence trial of melarsoprol and nifurtimox monotherapy and combination therapy for the treatment of second-stage Trypanosoma brucei rhodesiense sleeping sickness". J. Infect. Dis. 195 (3): 322–9. doi:10.1086/510534. PMID 17205469.
- ↑ "WHO Model List of Essential Medicines". World Health Organization. October 2013. Retrieved 22 April 2014.
- ↑ 3.0 3.1 3.2 3.3 Brunton L (2011). "Goodman & Gillman’s The Pharmacological Basis of Therapeutics". McGraw Hill Medical. pp. 1427–28.
- ↑ Schweingruber ME (2004). "The Melaminophenyl Arsenicals Melarsoprol and Melarsen Oxide Interfere with Thiamine Metabolism in the Fission Yeast Schizosaccharomyces pombe.". Antimicrobial Agents and Chemotherapy 48 (9): 3268–3271. doi:10.1128/AAC.
- ↑ CDC (2013). "Disease Control and Prevention: Parasites Africian Trypanosomiasis".
- ↑ World Health Organization (2013). "Human African Trypanosomiasis".
- ↑ Keiser J.; Ericsson O; Burri C (2000). "Investigations of the metabolites of the trypanocidal drug melarsoprol". Clinical Pharmacology 67: 478–88. doi:10.1067/mcp.2000.105990.
- ↑ Farrar J (2014). "Manson’s Tropical Diseases: Expert Consult-Online" 23. p. 616.
- ↑ Hollingham R (2005). "Curing diseases modern medicine has left behind". New Scientist 2005 (2482): 40–41.
- ↑ Balasegaram M; Harris S; Checchi F et al. (2006). "Melarsoprol versus eflornithine for treating late-stage Gambian trypanosomiasis in the Republic of the Congo". Bulletin of the WHO 84 (10): 783–91. doi:10.2471/blt.06.031955.
| ||||||||||||||||||||||||||||||||||||||||||||||||