Major depressive disorder
| Major depressive disorder | |
|---|---|
|
| |
| Classification and external resources | |
| ICD-10 | F32, F33 |
| ICD-9 | 296.2, 296.3 |
| OMIM | 608516 |
| DiseasesDB | 3589 |
| MedlinePlus | 003213 |
| eMedicine | med/532 |
| Patient UK | Major depressive disorder |
| MeSH | D003865 |
Major depressive disorder (MDD) (also known as clinical depression, major depression, unipolar depression, or unipolar disorder; or as recurrent depression in the case of repeated episodes) is a mental disorder characterized by a pervasive and persistent low mood that is accompanied by low self-esteem and by a loss of interest or pleasure in normally enjoyable activities. The term "depression" is used in a number of different ways. It is often used to mean this syndrome but may refer to other mood disorders or simply to a low mood. Major depressive disorder is a disabling condition that adversely affects a person's family, work or school life, sleeping and eating habits, and general health. In the United States, around 3.4% of people with major depression commit suicide, and up to 60% of people who commit suicide had depression or another mood disorder.[1]
The diagnosis of major depressive disorder is based on the patient's self-reported experiences, behavior reported by relatives or friends, and a mental status examination. There is no laboratory test for major depression, although physicians generally request tests for physical conditions that may cause similar symptoms. The most common time of onset is between the ages of 20 and 30 years, with a later peak between 30 and 40 years.[2]
Typically, people are treated with antidepressant medication and, in many cases, also receive counseling, particularly cognitive behavioral therapy (CBT).[3] Medication appears to be effective, but the effect may only be significant in the most severely depressed.[4][5] Hospitalization may be necessary in cases with associated self-neglect or a significant risk of harm to self or others. A minority are treated with electroconvulsive therapy (ECT). The course of the disorder varies widely, from one episode lasting weeks to a lifelong disorder with recurrent major depressive episodes. Depressed individuals have shorter life expectancies than those without depression, in part because of greater susceptibility to medical illnesses and suicide. It is unclear whether medications affect the risk of suicide. Current and former patients may be stigmatized.
The understanding of the nature and causes of depression has evolved over the centuries, though this understanding is incomplete and has left many aspects of depression as the subject of discussion and research. Proposed causes include psychological, psycho-social, hereditary, evolutionary and biological factors. Long-term substance abuse may cause or worsen depressive symptoms. Psychological treatments are based on theories of personality, interpersonal communication, and learning. Most biological theories focus on the monoamine chemicals serotonin, norepinephrine and dopamine, which are naturally present in the brain and assist communication between nerve cells. This cluster of symptoms (syndrome) was named, described and classified as one of the mood disorders in the 1980 edition of the American Psychiatric Association's diagnostic manual.
Symptoms and signs
Major depression significantly affects a person's family and personal relationships, work or school life, sleeping and eating habits, and general health.[6] Its impact on functioning and well-being has been compared to that of chronic medical conditions such as diabetes.[7]
A person having a major depressive episode usually exhibits a very low mood, which pervades all aspects of life, and an inability to experience pleasure in activities that were formerly enjoyed. Depressed people may be preoccupied with, or ruminate over, thoughts and feelings of worthlessness, inappropriate guilt or regret, helplessness, hopelessness, and self-hatred.[8] In severe cases, depressed people may have symptoms of psychosis. These symptoms include delusions or, less commonly, hallucinations, usually unpleasant.[9] Other symptoms of depression include poor concentration and memory (especially in those with melancholic or psychotic features),[10] withdrawal from social situations and activities, reduced sex drive, and thoughts of death or suicide. Insomnia is common among the depressed. In the typical pattern, a person wakes very early and cannot get back to sleep.[11] Hypersomnia, or oversleeping, can also happen.[11] Some antidepressants may also cause insomnia due to their stimulating effect.[12]
A depressed person may report multiple physical symptoms such as fatigue, headaches, or digestive problems; physical complaints are the most common presenting problem in developing countries, according to the World Health Organization's criteria for depression.[13] Appetite often decreases, with resulting weight loss, although increased appetite and weight gain occasionally occur.[8] Family and friends may notice that the person's behavior is either agitated or lethargic.[11] Older depressed people may have cognitive symptoms of recent onset, such as forgetfulness,[10] and a more noticeable slowing of movements.[14] Depression often coexists with physical disorders common among the elderly, such as stroke, other cardiovascular diseases, Parkinson's disease, and chronic obstructive pulmonary disease.[15]
Depressed children may often display an irritable mood rather than a depressed mood,[8] and show varying symptoms depending on age and situation.[16] Most lose interest in school and show a decline in academic performance. They may be described as clingy, demanding, dependent, or insecure.[11] Diagnosis may be delayed or missed when symptoms are interpreted as normal moodiness.[8] Depression may also coexist with attention-deficit hyperactivity disorder (ADHD), complicating the diagnosis and treatment of both.[17]
Comorbidity
Major depression frequently co-occurs with other psychiatric problems. The 1990–92 National Comorbidity Survey (US) reports that 51% of those with major depression also suffer from lifetime anxiety.[18] Anxiety symptoms can have a major impact on the course of a depressive illness, with delayed recovery, increased risk of relapse, greater disability and increased suicide attempts.[19] American neuroendocrinologist Robert Sapolsky similarly argues that the relationship between stress, anxiety, and depression could be measured and demonstrated biologically.[20] There are increased rates of alcohol and drug abuse and particularly dependence,[21] and around a third of individuals diagnosed with ADHD develop comorbid depression.[22] Post-traumatic stress disorder and depression often co-occur.[6]
Depression and pain often co-occur. One or more pain symptoms are present in 65% of depressed patients, and anywhere from 5 to 85% of patients with pain will be suffering from depression, depending on the setting; there is a lower prevalence in general practice, and higher in specialty clinics. The diagnosis of depression is often delayed or missed, and the outcome worsens. The outcome can also worsen if the depression is noticed but completely misunderstood.[23]
Depression is also associated with a 1.5- to 2-fold increased risk of cardiovascular disease, independent of other known risk factors, and is itself linked directly or indirectly to risk factors such as smoking and obesity. People with major depression are less likely to follow medical recommendations for treating and preventing cardiovascular disorders, which further increases their risk of medical complications.[24] In addition, cardiologists may not recognize underlying depression that complicates a cardiovascular problem under their care.[25]
Causes
The biopsychosocial model proposes that biological, psychological, and social factors all play a role in causing depression.[26] The diathesis–stress model specifies that depression results when a preexisting vulnerability, or diathesis, is activated by stressful life events. The preexisting vulnerability can be either genetic,[27][28] implying an interaction between nature and nurture, or schematic, resulting from views of the world learned in childhood.[29]
Depression may be directly caused by damage to the cerebellum as is seen in cerebellar cognitive affective syndrome.[30][31][32]
These interactive models have gained empirical support. For example, researchers in New Zealand took a prospective approach to studying depression, by documenting over time how depression emerged among an initially normal cohort of people. The researchers concluded that variation among the serotonin transporter (5-HTT) gene affects the chances that people who have dealt with very stressful life events will go on to experience depression. To be specific, depression may follow such events, but seems more likely to appear in people with one or two short alleles of the 5-HTT gene.[27] In addition, a Swedish study estimated the heritability of depression—the degree to which individual differences in occurrence are associated with genetic differences—to be around 40% for women and 30% for men,[33] and evolutionary psychologists have proposed that the genetic basis for depression lies deep in the history of naturally selected adaptations. A substance-induced mood disorder resembling major depression has been causally linked to long-term drug use or drug abuse, or to withdrawal from certain sedative and hypnotic drugs.[34][35]
Biological
Monoamine hypothesis

Most antidepressant medications increase the levels of one or more of the monoamines—the neurotransmitters serotonin, norepinephrine and dopamine—in the synaptic cleft between neurons in the brain. Some medications affect the monoamine receptors directly.
Serotonin is hypothesized to regulate other neurotransmitter systems; decreased serotonin activity may allow these systems to act in unusual and erratic ways.[36] According to this "permissive hypothesis", depression arises when low serotonin levels promote low levels of norepinephrine, another monoamine neurotransmitter.[37] Some antidepressants enhance the levels of norepinephrine directly, whereas others raise the levels of dopamine, a third monoamine neurotransmitter. These observations gave rise to the monoamine hypothesis of depression. In its contemporary formulation, the monoamine hypothesis postulates that a deficiency of certain neurotransmitters is responsible for the corresponding features of depression: "Norepinephrine may be related to alertness and energy as well as anxiety, attention, and interest in life; [lack of] serotonin to anxiety, obsessions, and compulsions; and dopamine to attention, motivation, pleasure, and reward, as well as interest in life."[38] The proponents of this theory recommend the choice of an antidepressant with mechanism of action that impacts the most prominent symptoms. Anxious and irritable patients should be treated with SSRIs or norepinephrine reuptake inhibitors, and those experiencing a loss of energy and enjoyment of life with norepinephrine- and dopamine-enhancing drugs.[38]
Besides the clinical observations that drugs that increase the amount of available monoamines are effective antidepressants, recent advances in psychiatric genetics indicate that phenotypic variation in central monoamine function may be marginally associated with vulnerability to depression. Despite these findings, the cause of depression is not simply monoamine deficiency.[39] In the past two decades, research has revealed multiple limitations of the monoamine hypothesis, and its explanatory inadequacy has been highlighted within the psychiatric community.[40] A counterargument is that the mood-enhancing effect of MAO inhibitors and SSRIs takes weeks of treatment to develop, even though the boost in available monoamines occurs within hours. Another counterargument is based on experiments with pharmacological agents that cause depletion of monoamines; while deliberate reduction in the concentration of centrally available monoamines may slightly lower the mood of unmedicated depressed patients, this reduction does not affect the mood of healthy people.[39] The monoamine hypothesis, already limited, has been further oversimplified when presented to the public as a mass marketing tool, usually phrased as a "chemical imbalance".[41]
In 2003 a gene-environment interaction (GxE) was hypothesized to explain why life stress is a predictor for depressive episodes in some individuals, but not in others, depending on an allelic variation of the serotonin-transporter-linked promoter region (5-HTTLPR);[27] a 2009 meta-analysis showed stressful life events were associated with depression, but found no evidence for an association with the 5-HTTLPR genotype.[42] Another 2009 meta-analysis agreed with the latter finding.[43] A 2010 review of studies in this area found a systematic relationship between the method used to assess environmental adversity and the results of the studies; this review also found that both 2009 meta-analyses were significantly biased toward negative studies, which used self-report measures of adversity.[44]
Other hypotheses
MRI scans of patients with depression have revealed a number of differences in brain structure compared to those who are not depressed. Recent meta-analyses of neuroimaging studies in major depression reported that, compared to controls, depressed patients had increased volume of the lateral ventricles and adrenal gland and smaller volumes of the basal ganglia, thalamus, hippocampus, and frontal lobe (including the orbitofrontal cortex and gyrus rectus).[45][46] Hyperintensities have been associated with patients with a late age of onset, and have led to the development of the theory of vascular depression.[47]
There may be a link between depression and neurogenesis of the hippocampus,[48] a center for both mood and memory. Loss of hippocampal neurons is found in some depressed individuals and correlates with impaired memory and dysthymic mood. Drugs may increase serotonin levels in the brain, stimulating neurogenesis and thus increasing the total mass of the hippocampus. This increase may help to restore mood and memory.[49][50] Similar relationships have been observed between depression and an area of the anterior cingulate cortex implicated in the modulation of emotional behavior.[51] One of the neurotrophins responsible for neurogenesis is brain-derived neurotrophic factor (BDNF). The level of BDNF in the blood plasma of depressed subjects is drastically reduced (more than threefold) as compared to the norm. Antidepressant treatment increases the blood level of BDNF. Although decreased plasma BDNF levels have been found in many other disorders, there is some evidence that BDNF is involved in the cause of depression and the mechanism of action of antidepressants.[52]
There is some evidence that major depression may be caused in part by an overactive hypothalamic-pituitary-adrenal axis (HPA axis) that results in an effect similar to the neuro-endocrine response to stress. Investigations reveal increased levels of the hormone cortisol and enlarged pituitary and adrenal glands, suggesting disturbances of the endocrine system may play a role in some psychiatric disorders, including major depression. Oversecretion of corticotropin-releasing hormone from the hypothalamus is thought to drive this, and is implicated in the cognitive and arousal symptoms.[53]
The hormone estrogen has been implicated in depressive disorders due to the increase in risk of depressive episodes after puberty, the antenatal period, and reduced rates after menopause.[54] On the converse, the premenstrual and postpartum periods of low estrogen levels are also associated with increased risk.[54] Sudden withdrawal of, fluctuations in or periods of sustained low levels of estrogen have been linked to significant mood lowering. Clinical recovery from depression postpartum, perimenopause, and postmenopause was shown to be effective after levels of estrogen were stabilized or restored.[55][56]
Other research has explored potential roles of molecules necessary for overall cellular functioning: cytokines. The symptoms of major depressive disorder are nearly identical to those of sickness behavior, the response of the body when the immune system is fighting an infection. This raises the possibility that depression can result from a maladaptive manifestation of sickness behavior as a result of abnormalities in circulating cytokines.[57] The involvement of pro-inflammatory cytokines in depression is strongly suggested by a meta-analysis of the clinical literature showing higher blood concentrations of IL-6 and TNF-α in depressed subjects compared to controls.[58] These immunological abnormalities may cause excessive prostaglandin E₂ production and likely excessive COX-2 expression. Abnormalities in how indoleamine 2,3-dioxygenase enzyme activates as well as the metabolism of tryptophan-kynurenine may lead to excessive metabolism of tryptophan-kynurenine and lead to increased production of the neurotoxin quinolinic acid, contributing to major depression. NMDA activation leading to excessive glutamatergic neurotransmission, may also contribute.[59]
Psychological
Various aspects of personality and its development appear to be integral to the occurrence and persistence of depression,[60] with negative emotionality as a common precursor.[61] Although depressive episodes are strongly correlated with adverse events, a person's characteristic style of coping may be correlated with his or her resilience.[62] In addition, low self-esteem and self-defeating or distorted thinking are related to depression. Depression is less likely to occur, as well as quicker to remit, among those who are religious.[63][64][65] It is not always clear which factors are causes and which are effects of depression; however, depressed persons that are able to reflect upon and challenge their thinking patterns often show improved mood and self-esteem.[66]
American psychiatrist Aaron T. Beck, following on from the earlier work of George Kelly and Albert Ellis, developed what is now known as a cognitive model of depression in the early 1960s. He proposed that three concepts underlie depression: a triad of negative thoughts composed of cognitive errors about oneself, one's world, and one's future; recurrent patterns of depressive thinking, or schemas; and distorted information processing.[67] From these principles, he developed the structured technique of cognitive behavioral therapy (CBT).[68] According to American psychologist Martin Seligman, depression in humans is similar to learned helplessness in laboratory animals, who remain in unpleasant situations when they are able to escape, but do not because they initially learned they had no control.[69]
Attachment theory, which was developed by English psychiatrist John Bowlby in the 1960s, predicts a relationship between depressive disorder in adulthood and the quality of the earlier bond between the infant and the adult caregiver. In particular, it is thought that "the experiences of early loss, separation and rejection by the parent or caregiver (conveying the message that the child is unlovable) may all lead to insecure internal working models ... Internal cognitive representations of the self as unlovable and of attachment figures as unloving [or] untrustworthy would be consistent with parts of Beck's cognitive triad".[70] While a wide variety of studies has upheld the basic tenets of attachment theory, research has been inconclusive as to whether self-reported early attachment and later depression are demonstrably related.[70]
Depressed individuals often blame themselves for negative events,[71] and, as shown in a 1993 study of hospitalized adolescents with self-reported depression, those who blame themselves for negative occurrences may not take credit for positive outcomes.[72] This tendency is characteristic of a depressive attributional, or pessimistic explanatory style.[71] According to Albert Bandura, a Canadian social psychologist associated with social cognitive theory, depressed individuals have negative beliefs about themselves, based on experiences of failure, observing the failure of social models, a lack of social persuasion that they can succeed, and their own somatic and emotional states including tension and stress. These influences may result in a negative self-concept and a lack of self-efficacy; that is, they do not believe they can influence events or achieve personal goals.[73][74]
An examination of depression in women indicates that vulnerability factors—such as early maternal loss, lack of a confiding relationship, responsibility for the care of several young children at home, and unemployment—can interact with life stressors to increase the risk of depression.[75] For older adults, the factors are often health problems, changes in relationships with a spouse or adult children due to the transition to a care-giving or care-needing role, the death of a significant other, or a change in the availability or quality of social relationships with older friends because of their own health-related life changes.[76]
The understanding of depression has also received contributions from the psychoanalytic and humanistic branches of psychology. From the classical psychoanalytic perspective of Austrian psychiatrist Sigmund Freud, depression, or melancholia, may be related to interpersonal loss[77][78] and early life experiences.[79] Existential therapists have connected depression to the lack of both meaning in the present[80] and a vision of the future.[81][82]
Social
Poverty and social isolation are associated with increased risk of mental health problems in general.[60] Child abuse (physical, emotional, sexual, or neglect) is also associated with increased risk of developing depressive disorders later in life.[83] Such a link has good face validity given that it is during the years of development that a child is learning how to become a social being. Abuse of the child by the caregiver is bound to distort the developing personality and create a much greater risk for depression and many other debilitating mental and emotional states. Disturbances in family functioning, such as parental (particularly maternal) depression, severe marital conflict or divorce, death of a parent, or other disturbances in parenting are additional risk factors.[60] In adulthood, stressful life events are strongly associated with the onset of major depressive episodes.[84] In this context, life events connected to social rejection appear to be particularly related to depression.[85][86] Evidence that a first episode of depression is more likely to be immediately preceded by stressful life events than are recurrent ones is consistent with the hypothesis that people may become increasingly sensitized to life stress over successive recurrences of depression.[87][88]
The relationship between stressful life events and social support has been a matter of some debate; the lack of social support may increase the likelihood that life stress will lead to depression, or the absence of social support may constitute a form of strain that leads to depression directly.[89] There is evidence that neighborhood social disorder, for example, due to crime or illicit drugs, is a risk factor, and that a high neighborhood socioeconomic status, with better amenities, is a protective factor.[90] Adverse conditions at work, particularly demanding jobs with little scope for decision-making, are associated with depression, although diversity and confounding factors make it difficult to confirm that the relationship is causal.[91]
Depression can be caused by prejudice. This can occur when people hold negative self-stereotypes about themselves. This "deprejudice" can be related to a group membership (e.g., Me-Gay-Bad) or not (Me-Bad). If someone has prejudicial beliefs about a stigmatized group and then becomes a member of that group, they may internalize their prejudice and develop depression. For example, a boy growing up in the United States may learn the negative stereotype that gay men are immoral. When he grows up and realizes he is gay, he may direct this prejudice inward on himself and become depressed. People may also show prejudice internalization through self-stereotyping because of negative childhood experiences such as verbal and physical abuse.[92]
Evolutionary
From the standpoint of evolutionary theory, major depression is hypothesized, in some instances, to increase an individual's reproductive fitness. Evolutionary approaches to depression and evolutionary psychology posit specific mechanisms by which depression may have been genetically incorporated into the human gene pool, accounting for the high heritability and prevalence of depression by proposing that certain components of depression are adaptations,[93] such as the behaviors relating to attachment and social rank.[94] Current behaviors can be explained as adaptations to regulate relationships or resources, although the result may be maladaptive in modern environments.[95]
From another viewpoint, a counseling therapist may see depression not as a biochemical illness or disorder but as "a species-wide evolved suite of emotional programs that are mostly activated by a perception, almost always over-negative, of a major decline in personal usefulness, that can sometimes be linked to guilt, shame or perceived rejection".[96] This suite may have manifested in aging hunters in humans' foraging past, who were marginalized by their declining skills, and may continue to appear in alienated members of today's society. The feelings of uselessness generated by such marginalization could in theory prompt support from friends and kin. In addition, in a manner analogous to that in which physical pain has evolved to hinder actions that may cause further injury, "psychic misery" may have evolved to prevent hasty and maladaptive reactions to distressing situations.[97]
Drug and alcohol use
Very high levels of substance abuse occur in the psychiatric population, especially alcohol, sedatives and cannabis. Depression and other mental health problems can have a substance induced cause; making a differential or dual diagnosis regarding whether mental ill-health is substance related or not or co-occurring is an important part of a psychiatric evaluation.[98] According to the DSM-IV, a diagnosis of mood disorder cannot be made if the cause is believed to be due to "the direct physiological effects of a substance"; when a syndrome resembling major depression is believed to be caused immediately by substance abuse or by an adverse drug reaction, it is referred to as, "substance-induced mood disturbance". Alcoholism or excessive alcohol consumption significantly increases the risk of developing major depression.[99][100] Like alcohol, the benzodiazepines are central nervous system depressants; this class of medication is commonly used to treat insomnia, anxiety, and muscular spasms. Similar to alcohol, benzodiazepines increase the risk of developing major depression. This increased risk of depression may be due in part to the adverse or toxic effects of sedative-hypnotic drugs including alcohol on neurochemistry,[100] such as decreased levels of serotonin and norepinephrine,[35] or activation of immune mediated inflammatory pathways in the brain.[101] Chronic use of benzodiazepines also can cause or worsen depression,[102] or depression may be part of a protracted withdrawal syndrome.[103][104] About a quarter of people recovering from alcoholism experience anxiety and depression, which can persist for up to 2 years.[105] Methamphetamine abuse is also commonly associated with depression.[106]
Diagnosis
Clinical assessment
A diagnostic assessment may be conducted by a suitably trained general practitioner, or by a psychiatrist or psychologist,[6] who records the person's current circumstances, biographical history, current symptoms, and family history. The broad clinical aim is to formulate the relevant biological, psychological, and social factors that may be impacting on the individual's mood. The assessor may also discuss the person's current ways of regulating mood (healthy or otherwise) such as alcohol and drug use. The assessment also includes a mental state examination, which is an assessment of the person's current mood and thought content, in particular the presence of themes of hopelessness or pessimism, self-harm or suicide, and an absence of positive thoughts or plans.[6] Specialist mental health services are rare in rural areas, and thus diagnosis and management is left largely to primary-care clinicians.[107] This issue is even more marked in developing countries.[108] The mental health examination may include the use of a rating scale such as the Hamilton Rating Scale for Depression[109] or the Beck Depression Inventory.[110] The score on a rating scale alone is insufficient to diagnose depression to the satisfaction of the DSM or ICD, but it provides an indication of the severity of symptoms for a time period, so a person who scores above a given cut-off point can be more thoroughly evaluated for a depressive disorder diagnosis.[111] Several rating scales are used for this purpose.[111] Screening programs have been advocated to improve detection of depression, but there is evidence that they do not improve detection rates, treatment, or outcome.[112]
Primary-care physicians and other non-psychiatrist physicians have difficulty diagnosing depression, in part because they are trained to recognize and treat physical symptoms, and depression can cause myriad physical (psychosomatic) symptoms. Non-psychiatrists miss two-thirds of cases and unnecessarily treat other patients.[113][114]
Before diagnosing a major depressive disorder, in general a doctor performs a medical examination and selected investigations to rule out other causes of symptoms. These include blood tests measuring TSH and thyroxine to exclude hypothyroidism; basic electrolytes and serum calcium to rule out a metabolic disturbance; and a full blood count including ESR to rule out a systemic infection or chronic disease.[114] Adverse affective reactions to medications or alcohol misuse are often ruled out, as well. Testosterone levels may be evaluated to diagnose hypogonadism, a cause of depression in men.[115]
Subjective cognitive complaints appear in older depressed people, but they can also be indicative of the onset of a dementing disorder, such as Alzheimer's disease.[116][117] Cognitive testing and brain imaging can help distinguish depression from dementia.[118] A CT scan can exclude brain pathology in those with psychotic, rapid-onset or otherwise unusual symptoms.[119] In general, investigations are not repeated for a subsequent episode unless there is a medical indication.
No biological tests confirm major depression.[120] Biomarkers of depression have been sought to provide an objective method of diagnosis. There are several potential biomarkers, including Brain-Derived Neurotrophic Factor and various functional MRI techniques. One study developed a decision tree model of interpreting a series of fMRI scans taken during various activities. In their subjects, the authors of that study were able to achieve a sensitivity of 80% and a specificity of 87%, corresponding to a negative predictive value of 98% and a positive predictive value of 32% (positive and negative likelihood ratios were 6.15, 0.23, respectively). However, much more research is needed before these tests could be used clinically.[121]
DSM-IV-TR and ICD-10 criteria
The most widely used criteria for diagnosing depressive conditions are found in the American Psychiatric Association's revised fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR), and the World Health Organization's International Statistical Classification of Diseases and Related Health Problems (ICD-10), which uses the name depressive episode for a single episode and recurrent depressive disorder for repeated episodes.[122] The latter system is typically used in European countries, while the former is used in the US and many other non-European nations,[123] and the authors of both have worked towards conforming one with the other.[124]
Both DSM-IV-TR and ICD-10 mark out typical (main) depressive symptoms.[125] ICD-10 defines three typical depressive symptoms (depressed mood, anhedonia, and reduced energy), two of which should be present to determine depressive disorder diagnosis.[126][127] According to DSM-IV-TR, there are two main depressive symptoms—depressed mood and anhedonia. At least one of these must be present to make a diagnosis of major depressive episode.[128]
Major depressive disorder is classified as a mood disorder in DSM-IV-TR.[129] The diagnosis hinges on the presence of single or recurrent major depressive episodes.[8] Further qualifiers are used to classify both the episode itself and the course of the disorder. The category Depressive Disorder Not Otherwise Specified is diagnosed if the depressive episode's manifestation does not meet the criteria for a major depressive episode. The ICD-10 system does not use the term major depressive disorder but lists very similar criteria for the diagnosis of a depressive episode (mild, moderate or severe); the term recurrent may be added if there have been multiple episodes without mania.[122]
Major depressive episode
A major depressive episode is characterized by the presence of a severely depressed mood that persists for at least two weeks.[8] Episodes may be isolated or recurrent and are categorized as mild (few symptoms in excess of minimum criteria), moderate, or severe (marked impact on social or occupational functioning). An episode with psychotic features—commonly referred to as psychotic depression—is automatically rated as severe. If the patient has had an episode of mania or markedly elevated mood, a diagnosis of bipolar disorder is made instead.[130] Depression without mania is sometimes referred to as unipolar because the mood remains at one emotional state or "pole".[131]
DSM-IV-TR excludes cases where the symptoms are a result of bereavement, although it is possible for normal bereavement to evolve into a depressive episode if the mood persists and the characteristic features of a major depressive episode develop.[132] The criteria have been criticized because they do not take into account any other aspects of the personal and social context in which depression can occur.[133] In addition, some studies have found little empirical support for the DSM-IV cut-off criteria, indicating they are a diagnostic convention imposed on a continuum of depressive symptoms of varying severity and duration:[134] Excluded are a range of related diagnoses, including dysthymia, which involves a chronic but milder mood disturbance;[135] recurrent brief depression, consisting of briefer depressive episodes;[136][137] minor depressive disorder, whereby only some symptoms of major depression are present;[138] and adjustment disorder with depressed mood, which denotes low mood resulting from a psychological response to an identifiable event or stressor.[139]
Subtypes
The DSM-IV-TR recognizes five further subtypes of MDD, called specifiers, in addition to noting the length, severity and presence of psychotic features:
- Melancholic depression is characterized by a loss of pleasure in most or all activities, a failure of reactivity to pleasurable stimuli, a quality of depressed mood more pronounced than that of grief or loss, a worsening of symptoms in the morning hours, early-morning waking, psychomotor retardation, excessive weight loss (not to be confused with anorexia nervosa), or excessive guilt.[140]
- Atypical depression is characterized by mood reactivity (paradoxical anhedonia) and positivity, significant weight gain or increased appetite (comfort eating), excessive sleep or sleepiness (hypersomnia), a sensation of heaviness in limbs known as leaden paralysis, and significant social impairment as a consequence of hypersensitivity to perceived interpersonal rejection.[141]
- Catatonic depression is a rare and severe form of major depression involving disturbances of motor behavior and other symptoms. Here, the person is mute and almost stuporous, and either remains immobile or exhibits purposeless or even bizarre movements. Catatonic symptoms also occur in schizophrenia or in manic episodes, or may be caused by neuroleptic malignant syndrome.[142]
- Postpartum depression, or mental and behavioral disorders associated with the puerperium, not elsewhere classified,[122] refers to the intense, sustained and sometimes disabling depression experienced by women after giving birth. Postpartum depression has an incidence rate of 10–15% among new mothers. The DSM-IV mandates that, in order to qualify as postpartum depression, onset occur within one month of delivery. It has been said that postpartum depression can last as long as three months.[143]
- Seasonal affective disorder (SAD) is a form of depression in which depressive episodes come on in the autumn or winter, and resolve in spring. The diagnosis is made if at least two episodes have occurred in colder months with none at other times, over a two-year period or longer.[144]
Differential diagnoses
To confer major depressive disorder as the most likely diagnosis, other potential diagnoses must be considered, including dysthymia, adjustment disorder with depressed mood, or bipolar disorder. Dysthymia is a chronic, milder mood disturbance in which a person reports a low mood almost daily over a span of at least two years. The symptoms are not as severe as those for major depression, although people with dysthymia are vulnerable to secondary episodes of major depression (sometimes referred to as double depression).[135] Adjustment disorder with depressed mood is a mood disturbance appearing as a psychological response to an identifiable event or stressor, in which the resulting emotional or behavioral symptoms are significant but do not meet the criteria for a major depressive episode.[139] Bipolar disorder, also known as manic–depressive disorder, is a condition in which depressive phases alternate with periods of mania or hypomania. Although depression is currently categorized as a separate disorder, there is ongoing debate because individuals diagnosed with major depression often experience some hypomanic symptoms, indicating a mood disorder continuum.[145]
Other disorders need to be ruled out before diagnosing major depressive disorder. They include depressions due to physical illness, medications, and substance abuse. Depression due to physical illness is diagnosed as a mood disorder due to a general medical condition. This condition is determined based on history, laboratory findings, or physical examination. When the depression is caused by a substance abused including a drug of abuse, a medication, or exposure to a toxin, it is then diagnosed as a substance-induced mood disorder.[146]
Prevention
Behavioral interventions, such as interpersonal therapy and cognitive-behavioral therapy, are effective at preventing new onset depression.[147][148][149] Because such interventions appear to be most effective when delivered to individuals or small groups, it has been suggested that they may be able to reach their large target audience most efficiently through the Internet.[150]
However, an earlier meta-analysis found preventive programs with a competence-enhancing component to be superior to behavior-oriented programs overall, and found behavioral programs to be particularly unhelpful for older people, for whom social support programs were uniquely beneficial. In addition, the programs that best prevented depression comprised more than eight sessions, each lasting between 60 and 90 minutes, were provided by a combination of lay and professional workers, had a high-quality research design, reported attrition rates, and had a well-defined intervention.[151]
The Netherlands mental health care system provides preventive interventions, such as the "Coping with Depression" course (CWD) for people with sub-threshold depression. The course is claimed to be the most successful of psychoeducational interventions for the treatment and prevention of depression (both for its adaptability to various populations and its results), with a risk reduction of 38% in major depression and an efficacy as a treatment comparing favorably to other psychotherapies.[147][152] Preventative efforts may result in decreases in rates of the condition of between 22 and 38%.[149]
Management
The three most common treatments for depression are psychotherapy, medication, and electroconvulsive therapy. Psychotherapy is the treatment of choice (over medication) for people under 18. The UK National Institute for Health and Care Excellence (NICE) 2004 guidelines indicate that antidepressants should not be used for the initial treatment of mild depression, because the risk-benefit ratio is poor. The guidelines recommend that antidepressants treatment in combination with psychosocial interventions should be considered for:
- People with a past history of moderate or severe depression
- Those with mild depression that has been present for a long period
- As a second line treatment for mild depression that persists after other interventions
- As a first line treatment for moderate or severe depression.
The guidelines further note that antidepressant treatment should be continued for at least six months to reduce the risk of relapse, and that SSRIs are better tolerated than tricyclic antidepressants.[153]
American Psychiatric Association treatment guidelines recommend that initial treatment should be individually tailored based on factors including severity of symptoms, co-existing disorders, prior treatment experience, and patient preference. Options may include pharmacotherapy, psychotherapy, electroconvulsive therapy (ECT), transcranial magnetic stimulation (TMS) or light therapy. Antidepressant medication is recommended as an initial treatment choice in people with mild, moderate, or severe major depression, and should be given to all patients with severe depression unless ECT is planned.[154]
Treatment options are much more limited in developing countries, where access to mental health staff, medication, and psychotherapy is often difficult. Development of mental health services is minimal in many countries; depression is viewed as a phenomenon of the developed world despite evidence to the contrary, and not as an inherently life-threatening condition.[155] A 2014 Cochrane review found insufficient evidence to determine the effectiveness of psychological versus medical therapy in children.[156]
Psychotherapy
Psychotherapy can be delivered, to individuals, groups, or families by mental health professionals, including psychotherapists, psychiatrists, psychologists, clinical social workers, counselors, and suitably trained psychiatric nurses. With more complex and chronic forms of depression, a combination of medication and psychotherapy may be used.[157][158] A 2012 review found psychotherapy to be better than no treatment but not other treatments.[159]
Cognitive behavioral therapy (CBT) currently has the most research evidence for the treatment of depression in children and adolescents, and CBT and interpersonal psychotherapy (IPT) are preferred therapies for adolescent depression.[160] In people under 18, according to the National Institute for Health and Clinical Excellence, medication should be offered only in conjunction with a psychological therapy, such as CBT, interpersonal therapy, or family therapy.[161]
Psychotherapy has been shown to be effective in older people.[162][163] Successful psychotherapy appears to reduce the recurrence of depression even after it has been terminated or replaced by occasional booster sessions.
The most-studied form of psychotherapy for depression is CBT, which teaches clients to challenge self-defeating, but enduring ways of thinking (cognitions) and change counter-productive behaviors. Research beginning in the mid-1990s suggested that CBT could perform as well or as better than antidepressants in patients with moderate to severe depression.[164][165] CBT may be effective in depressed adolescents,[166] although its effects on severe episodes are not definitively known.[167] Several variables predict success for cognitive behavioral therapy in adolescents: higher levels of rational thoughts, less hopelessness, fewer negative thoughts, and fewer cognitive distortions.[168] CBT is particularly beneficial in preventing relapse.[169][170] Several variants of cognitive behavior therapy have been used in those with depression, the most notable being rational emotive behavior therapy,[171] and mindfulness-based cognitive therapy.[172] Mindfulness based stress reduction programs may reduce depression symptoms.[173][174] Mindfulness programs also appear to be a promising intervention in youth.[175]
Psychoanalysis is a school of thought, founded by Sigmund Freud, which emphasizes the resolution of unconscious mental conflicts.[176] Psychoanalytic techniques are used by some practitioners to treat clients presenting with major depression.[177] A more widely practiced, eclectic technique, called psychodynamic psychotherapy, is loosely based on psychoanalysis and has an additional social and interpersonal focus.[178] In a meta-analysis of three controlled trials of Short Psychodynamic Supportive Psychotherapy, this modification was found to be as effective as medication for mild to moderate depression.[179]
Logotherapy, a form of existential psychotherapy developed by Austrian psychiatrist Viktor Frankl, addresses the filling of an "existential vacuum" associated with feelings of futility and meaninglessness. It is posited that this type of psychotherapy may be useful for depression in older adolescents.[180]
Antidepressants

Conflicting results have arisen from studies look at the effectiveness of antidepressants in people with acute mild to moderate depression. Stronger evidence supports the usefulness of antidepressants in the treatment of depression that is chronic (dysthymia) or severe.
While small benefits were found researchers Irving Kirsch and Thomas Moore state they may be due to issues with the trials rather than a true effect of the medication.[182] In a later publication, Kirsch concluded that the overall effect of new-generation antidepressant medication is below recommended criteria for clinical significance.[5] Similar results were obtained in a meta analysis by Fornier.[4]
A review commissioned by the National Institute for Health and Care Excellence concluded that there is strong evidence that SSRIs have greater efficacy than placebo on achieving a 50% reduction in depression scores in moderate and severe major depression, and that there is some evidence for a similar effect in mild depression.[183] Similarly, a Cochrane systematic review of clinical trials of the generic antidepressant amitriptyline concluded that there is strong evidence that its efficacy is superior to placebo.[184]
In 2014 the U.S. FDA published a systematic review of all antidepressant maintenance trials submitted to the agency between 1985 and 2012. The authors concluded that maintenance treatment reduced the risk of relapse by 52% compared to placebo, and that this effect was primarily due to recurrent depression in the placebo group rather than a drug withdrawal effect.[4]
To find the most effective antidepressant medication with minimal side-effects, the dosages can be adjusted, and if necessary, combinations of different classes of antidepressants can be tried. Response rates to the first antidepressant administered range from 50–75%, and it can take at least six to eight weeks from the start of medication to remission.[185] Antidepressant medication treatment is usually continued for 16 to 20 weeks after remission, to minimize the chance of recurrence,[185] and even up to one year of continuation is recommended.[186] People with chronic depression may need to take medication indefinitely to avoid relapse.[6]
Selective serotonin reuptake inhibitors (SSRIs) are the primary medications prescribed, owing to their relatively mild side-effects, and because they are less toxic in overdose than other antidepressants.[187] Patients who do not respond to one SSRI can be switched to another antidepressant, and this results in improvement in almost 50% of cases.[188] Another option is to switch to the atypical antidepressant bupropion.[189] Venlafaxine, an antidepressant with a different mechanism of action, may be modestly more effective than SSRIs.[190] However, venlafaxine is not recommended in the UK as a first-line treatment because of evidence suggesting its risks may outweigh benefits,[191] and it is specifically discouraged in children and adolescents.[192][193]
For adolescent depression, fluoxetine is recommended[192] Antidepressants appear to have only slight benefit in children.[194] There is also insufficient evidence to determine effectiveness in those with depression complicated by dementia.[195] Any antidepressant can cause low serum sodium levels (also called hyponatremia);[196] nevertheless, it has been reported more often with SSRIs.[187] It is not uncommon for SSRIs to cause or worsen insomnia; the sedating antidepressant mirtazapine can be used in such cases.[197][198]
Irreversible monoamine oxidase inhibitors, an older class of antidepressants, have been plagued by potentially life-threatening dietary and drug interactions. They are still used only rarely, although newer and better-tolerated agents of this class have been developed.[199] The safety profile is different with reversible monoamine oxidase inhibitors such as moclobemide where the risk of serious dietary interactions is negligible and dietary restrictions are less strict.[200]
For children, adolescents, and probably young adults between 18 and 24 years old, there is a higher risk of both suicidal ideations and suicidal behavior in those treated with SSRIs.[201][202] For adults, it is unclear whether SSRIs affect the risk of suicidality.[202] One review found no connection;[203] another an increased risk;[204] and a third no risk in those 25–65 years old and a decrease risk in those more than 65.[205] A black box warning was introduced in the United States in 2007 on SSRI and other antidepressant medications due to increased risk of suicide in patients younger than 24 years old.[206] Similar precautionary notice revisions were implemented by the Japanese Ministry of Health.[207]
Other medications
There is some evidence that fish oil supplements containing high levels of eicosapentaenoic acid (EPA) to docosahexaenoic acid (DHA) may be effective in major depression,[208] but other meta-analysis of the research conclude that positive effects may be due to publication bias.[209] There is some preliminary evidence that COX-2 inhibitors have a beneficial effect on major depression.[59] Lithium appears effective at lowering the risk of suicide in those with bipolar disorder and unipolar depression to nearly the same levels as the general population.[210] There is a narrow range of effective and safe dosages of lithium thus close monitoring may be needed.[211] Low-dose thyroid hormone may be added to existing antidepressants to treat persistent depression symptoms in people who have tried multiple courses of medication.[212]
Electroconvulsive therapy
Electroconvulsive therapy (ECT) is a standard psychiatric treatment in which seizures are electrically induced in patients to provide relief from psychiatric illnesses.[213]:1880 ECT is used with informed consent[214] as a last line of intervention for major depressive disorder.[215]
A round of ECT is effective for about 50% of people with treatment-resistant major depressive disorder, whether it is unipolar or bipolar.[216] Followup treatment is still poorly studied, but about half of people who respond, relapse with twelve months.[217]
Aside from effects in the brain, the general physical risks of ECT are similar to those of brief general anesthesia.[218]:259 Immediately following treatment, the most common adverse effects are confusion and memory loss.[215][219] ECT is considered one of the least harmful treatment options available for severely depressed pregnant women.[220]
A usual course of ECT involves multiple administrations, typically given two or three times per week until the patient is no longer suffering symptoms ECT is administered under anesthetic with a muscle relaxant.[221] Electroconvulsive therapy can differ in its application in three ways: electrode placement, frequency of treatments, and the electrical waveform of the stimulus. These three forms of application have significant differences in both adverse side effects and symptom remission. After treatment, drug therapy is usually continued, and some patients receive maintenance ECT.[215]
ECT appears to work in the short term via an anticonvulsant effect mostly in the frontal lobes, and longer term via neurotrophic effects primarily in the medial temporal lobe.[222]
Other
Bright light therapy reduces depression symptom severity, with benefit was found for both seasonal affective disorder and for nonseasonal depression, and an effect similar to those for conventional antidepressants. For non-seasonal depression, adding light therapy to the standard antidepressant treatment was not effective.[223] For non-seasonal depression where light was used mostly in combination with antidepressants or wake therapy a moderate effect was found, with response better than control treatment in high-quality studies, in studies that applied morning light treatment, and with people who respond to total or partial sleep deprivation.[224] Both analyses noted poor quality, short duration, and small size of most of the reviewed studies.
There is a small amount of evidence that skipping a night's sleep may help.[225] Physical exercise is recommended for management of mild depression,[226] and has a moderate effect on symptoms.[227] It is equivalent to the use of medications or psychological therapies in most people.[227] In the older people it does appear to decrease depression.[228] In unblinded, non-randomized observational studies Smoking cessation has benefits in depression as large as or larger than those of medications.[229] Cognitive behavioral therapy and occupational programs (including modification of work activities and assistance) have been shown to be effective in reducing sick days taken by workers with depression.[230]
Prognosis
Major depressive episodes often resolve over time whether or not they are treated. Outpatients on a waiting list show a 10–15% reduction in symptoms within a few months, with approximately 20% no longer meeting the full criteria for a depressive disorder.[231] The median duration of an episode has been estimated to be 23 weeks, with the highest rate of recovery in the first three months.[232]
Studies have shown that 80% of those suffering from their first major depressive episode will suffer from at least 1 more during their life,[233] with a lifetime average of 4 episodes.[234] Other general population studies indicate that around half those who have an episode recover (whether treated or not) and remain well, while the other half will have at least one more, and around 15% of those experience chronic recurrence.[235] Studies recruiting from selective inpatient sources suggest lower recovery and higher chronicity, while studies of mostly outpatients show that nearly all recover, with a median episode duration of 11 months. Around 90% of those with severe or psychotic depression, most of whom also meet criteria for other mental disorders, experience recurrence.[236][237]
Recurrence is more likely if symptoms have not fully resolved with treatment. Current guidelines recommend continuing antidepressants for four to six months after remission to prevent relapse. Evidence from many randomized controlled trials indicates continuing antidepressant medications after recovery can reduce the chance of relapse by 70% (41% on placebo vs. 18% on antidepressant). The preventive effect probably lasts for at least the first 36 months of use.[238]
Those people experiencing repeated episodes of depression require ongoing treatment in order to prevent more severe, long-term depression. In some cases, people must take medications for long periods of time or for the rest of their lives.[239]
Cases when outcome is poor are associated with inappropriate treatment, severe initial symptoms that may include psychosis, early age of onset, more previous episodes, incomplete recovery after 1 year, pre-existing severe mental or medical disorder, and family dysfunction as well.[240]
Depressed individuals have a shorter life expectancy than those without depression, in part because depressed patients are at risk of dying by suicide.[241] However, they also have a higher rate of dying from other causes,[242] being more susceptible to medical conditions such as heart disease.[243] Up to 60% of people who commit suicide have a mood disorder such as major depression, and the risk is especially high if a person has a marked sense of hopelessness or has both depression and borderline personality disorder.[1] The lifetime risk of suicide associated with a diagnosis of major depression in the US is estimated at 3.4%, which averages two highly disparate figures of almost 7% for men and 1% for women[244] (although suicide attempts are more frequent in women).[245] The estimate is substantially lower than a previously accepted figure of 15%, which had been derived from older studies of hospitalized patients.[246]
Depression is often associated with unemployment and poverty.[247] Major depression is currently the leading cause of disease burden in North America and other high-income countries, and the fourth-leading cause worldwide. In the year 2030, it is predicted to be the second-leading cause of disease burden worldwide after HIV, according to the World Health Organization.[248] Delay or failure in seeking treatment after relapse, and the failure of health professionals to provide treatment, are two barriers to reducing disability.[249]
Epidemiology
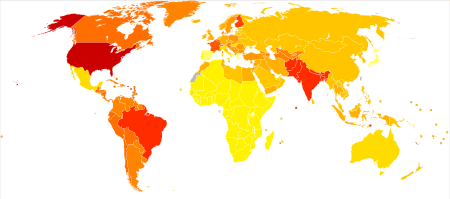
no data
<700
700–775
775–850
850–925
925–1000
1000–1075
|
1075–1150
1150–1225
1225–1300
1300–1375
1375–1450
>1450
|
Depression is a major cause of morbidity worldwide.[251] It is believed to currently affect approximately 298 million people as of 2010 (4.3% of the global population).[252] Lifetime prevalence varies widely, from 3% in Japan to 17% in the US.[253] In most countries the number of people who have depression during their lives falls within an 8–12% range.[253] In North America, the probability of having a major depressive episode within a year-long period is 3–5% for males and 8–10% for females.[254][255] Population studies have consistently shown major depression to be about twice as common in women as in men, although it is unclear why this is so, and whether factors unaccounted for are contributing to this.[256] The relative increase in occurrence is related to pubertal development rather than chronological age, reaches adult ratios between the ages of 15 and 18, and appears associated with psychosocial more than hormonal factors.[256]
People are most likely to suffer their first depressive episode between the ages of 30 and 40, and there is a second, smaller peak of incidence between ages 50 and 60.[257] The risk of major depression is increased with neurological conditions such as stroke, Parkinson's disease, or multiple sclerosis, and during the first year after childbirth.[258] It is also more common after cardiovascular illnesses, and is related more to a poor outcome than to a better one.[243][259] Studies conflict on the prevalence of depression in the elderly, but most data suggest there is a reduction in this age group.[260] Depressive disorders are more common to observe in urban than in rural population and the prevalence is in groups with stronger socioeconomic factors i.e. homelessness.[261]
History

The Ancient Greek physician Hippocrates described a syndrome of melancholia as a distinct disease with particular mental and physical symptoms; he characterized all "fears and despondencies, if they last a long time" as being symptomatic of the ailment.[262] It was a similar but far broader concept than today's depression; prominence was given to a clustering of the symptoms of sadness, dejection, and despondency, and often fear, anger, delusions and obsessions were included.[79]
The term depression itself was derived from the Latin verb deprimere, "to press down".[263] From the 14th century, "to depress" meant to subjugate or to bring down in spirits. It was used in 1665 in English author Richard Baker's Chronicle to refer to someone having "a great depression of spirit", and by English author Samuel Johnson in a similar sense in 1753.[264] The term also came into use in physiology and economics. An early usage referring to a psychiatric symptom was by French psychiatrist Louis Delasiauve in 1856, and by the 1860s it was appearing in medical dictionaries to refer to a physiological and metaphorical lowering of emotional function.[265] Since Aristotle, melancholia had been associated with men of learning and intellectual brilliance, a hazard of contemplation and creativity. The newer concept abandoned these associations and through the 19th century, became more associated with women.[79]
Although melancholia remained the dominant diagnostic term, depression gained increasing currency in medical treatises and was a synonym by the end of the century; German psychiatrist Emil Kraepelin may have been the first to use it as the overarching term, referring to different kinds of melancholia as depressive states.[266]
Sigmund Freud likened the state of melancholia to mourning in his 1917 paper Mourning and Melancholia. He theorized that objective loss, such as the loss of a valued relationship through death or a romantic break-up, results in subjective loss as well; the depressed individual has identified with the object of affection through an unconscious, narcissistic process called the libidinal cathexis of the ego. Such loss results in severe melancholic symptoms more profound than mourning; not only is the outside world viewed negatively but the ego itself is compromised.[77] The patient's decline of self-perception is revealed in his belief of his own blame, inferiority, and unworthiness.[78] He also emphasized early life experiences as a predisposing factor.[79] Adolf Meyer put forward a mixed social and biological framework emphasizing reactions in the context of an individual's life, and argued that the term depression should be used instead of melancholia.[267] The first version of the DSM (DSM-I, 1952) contained depressive reaction and the DSM-II (1968) depressive neurosis, defined as an excessive reaction to internal conflict or an identifiable event, and also included a depressive type of manic-depressive psychosis within Major affective disorders.[268]
In the mid-20th century, researchers theorized that depression was caused by a chemical imbalance in neurotransmitters in the brain, a theory based on observations made in the 1950s of the effects of reserpine and isoniazid in altering monoamine neurotransmitter levels and affecting depressive symptoms.[269]
The term "unipolar" (along with the related term "bipolar") was coined by the neurologist and psychiatrist Karl Kleist, and subsequently used by his disciples Edda Neele and Karl Leonhard.[270]
The term Major depressive disorder was introduced by a group of US clinicians in the mid-1970s as part of proposals for diagnostic criteria based on patterns of symptoms (called the "Research Diagnostic Criteria", building on earlier Feighner Criteria),[271] and was incorporated into the DSM-III in 1980.[272] To maintain consistency the ICD-10 used the same criteria, with only minor alterations, but using the DSM diagnostic threshold to mark a mild depressive episode, adding higher threshold categories for moderate and severe episodes.[125][272] The ancient idea of melancholia still survives in the notion of a melancholic subtype.
The new definitions of depression were widely accepted, albeit with some conflicting findings and views. There have been some continued empirically based arguments for a return to the diagnosis of melancholia.[273][274] There has been some criticism of the expansion of coverage of the diagnosis, related to the development and promotion of antidepressants and the biological model since the late 1950s.[275]
Society and culture

People's conceptualizations of depression vary widely, both within and among cultures. "Because of the lack of scientific certainty," one commentator has observed, "the debate over depression turns on questions of language. What we call it—'disease,' 'disorder,' 'state of mind'—affects how we view, diagnose, and treat it."[277] There are cultural differences in the extent to which serious depression is considered an illness requiring personal professional treatment, or is an indicator of something else, such as the need to address social or moral problems, the result of biological imbalances, or a reflection of individual differences in the understanding of distress that may reinforce feelings of powerlessness, and emotional struggle.[278][279]
The diagnosis is less common in some countries, such as China. It has been argued that the Chinese traditionally deny or somatize emotional depression (although since the early 1980s, the Chinese denial of depression may have modified drastically).[280] Alternatively, it may be that Western cultures reframe and elevate some expressions of human distress to disorder status. Australian professor Gordon Parker and others have argued that the Western concept of depression "medicalizes" sadness or misery.[281][282] Similarly, Hungarian-American psychiatrist Thomas Szasz and others argue that depression is a metaphorical illness that is inappropriately regarded as an actual disease.[283] There has also been concern that the DSM, as well as the field of descriptive psychiatry that employs it, tends to reify abstract phenomena such as depression, which may in fact be social constructs.[284] American archetypal psychologist James Hillman writes that depression can be healthy for the soul, insofar as "it brings refuge, limitation, focus, gravity, weight, and humble powerlessness."[285] Hillman argues that therapeutic attempts to eliminate depression echo the Christian theme of resurrection, but have the unfortunate effect of demonizing a soulful state of being.
Historical figures were often reluctant to discuss or seek treatment for depression due to social stigma about the condition, or due to ignorance of diagnosis or treatments. Nevertheless, analysis or interpretation of letters, journals, artwork, writings, or statements of family and friends of some historical personalities has led to the presumption that they may have had some form of depression. People who may have had depression include English author Mary Shelley,[286] American-British writer Henry James,[287] and American president Abraham Lincoln.[288] Some well-known contemporary people with possible depression include Canadian songwriter Leonard Cohen[289] and American playwright and novelist Tennessee Williams.[290] Some pioneering psychologists, such as Americans William James[291][292] and John B. Watson,[293] dealt with their own depression.
There has been a continuing discussion of whether neurological disorders and mood disorders may be linked to creativity, a discussion that goes back to Aristotelian times.[294][295] British literature gives many examples of reflections on depression.[296] English philosopher John Stuart Mill experienced a several-months-long period of what he called "a dull state of nerves", when one is "unsusceptible to enjoyment or pleasurable excitement; one of those moods when what is pleasure at other times, becomes insipid or indifferent". He quoted English poet Samuel Taylor Coleridge's "Dejection" as a perfect description of his case: "A grief without a pang, void, dark and drear, / A drowsy, stifled, unimpassioned grief, / Which finds no natural outlet or relief / In word, or sigh, or tear."[297][298] English writer Samuel Johnson used the term "the black dog" in the 1780s to describe his own depression,[299] and it was subsequently popularized by depression sufferer former British Prime Minister Sir Winston Churchill.[299]
Social stigma of major depression is widespread, and contact with mental health services reduces this only slightly. Public opinions on treatment differ markedly to those of health professionals; alternative treatments are held to be more helpful than pharmacological ones, which are viewed poorly.[300] In the UK, the Royal College of Psychiatrists and the Royal College of General Practitioners conducted a joint Five-year Defeat Depression campaign to educate and reduce stigma from 1992 to 1996;[301] a MORI study conducted afterwards showed a small positive change in public attitudes to depression and treatment.[302]
Other animals
References
- ↑ 1.0 1.1 Barlow 2005, pp. 248–49
- ↑ "Major Depressive Disorder". American Medical Network, Inc. Retrieved 15 January 2011.
- ↑ Driessen, Ellen; Hollon, Steven D. (2010). "Cognitive Behavioral Therapy for Mood Disorders: Efficacy, Moderators and Mediators". Psychiatric Clinics of North America 33 (3): 537–55.
- ↑ 4.0 4.1 4.2 Fournier JC, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD, Shelton RC, Fawcett J (January 2010). "Antidepressant drug effects and depression severity: a patient-level meta-analysis". JAMA 303 (1): 47–53. doi:10.1001/jama.2009.1943. PMC 3712503. PMID 20051569.
- ↑ 5.0 5.1 Kirsch I, Deacon BJ, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT (February 2008). "Initial severity and antidepressant benefits: a meta-analysis of data submitted to the Food and Drug Administration". PLoS Med. 5 (2): e45. doi:10.1371/journal.pmed.0050045. PMC 2253608. PMID 18303940.
- ↑ 6.0 6.1 6.2 6.3 6.4 Depression (PDF). National Institute of Mental Health (NIMH). Retrieved 7 September 2008.
- ↑ Hays RD, Wells KB, Sherbourne CD, Rogers W, Spritzer K (1995). "Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses". Archives of General Psychiatry 52 (1): 11–19. doi:10.1001/archpsyc.1995.03950130011002. PMID 7811158.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 American Psychiatric Association 2000a, p. 349
- ↑ American Psychiatric Association 2000a, p. 412
- ↑ 10.0 10.1 Delgado PL and Schillerstrom J (2009). "Cognitive Difficulties Associated With Depression: What Are the Implications for Treatment?". Psychiatric Times 26 (3).
- ↑ 11.0 11.1 11.2 11.3 American Psychiatric Association 2000a, p. 350
- ↑ "Insomnia: Assessment and Management in Primary Care". American Family Physician 59 (11): 3029–38. 1999. Retrieved 12 November 2014.
- ↑ Patel V, Abas M, Broadhead J (2001). "Depression in developing countries: Lessons from Zimbabwe". BMJ 322 (7284): 482–84. doi:10.1136/bmj.322.7284.482.
- ↑ Faculty of Psychiatry of Old Age, NSW Branch, RANZCP; Kitching D Raphael B (2001). Consensus Guidelines for Assessment and Management of Depression in the Elderly (PDF). North Sydney, New South Wales: NSW Health Department. p. 2. ISBN 0-7347-3341-0.
- ↑ Yohannes AM and Baldwin RC (2008). "Medical Comorbidities in Late-Life Depression". Psychiatric Times 25 (14).
- ↑ American Psychiatric Association 2000a, p. 354
- ↑ Brunsvold GL, Oepen G (2008). "Comorbid Depression in ADHD: Children and Adolescents". Psychiatric Times 25 (10).
- ↑ Kessler RC, Nelson CB, McGonagle KA, Liu J, Swartz M, Blazer DG (1996). "Comorbidity of DSM-III-R major depressive disorder in the general population: results from the US National Comorbidity Survey". British Journal of Psychiatry 168 (suppl 30): 17–30. PMID 8864145.
- ↑ Hirschfeld RM (2001). "The Comorbidity of Major Depression and Anxiety Disorders: Recognition and Management in Primary Care". Primary Care Companion to the Journal of Clinical Psychiatry 3 (6): 244–254. PMC 181193. PMID 15014592.
- ↑ Sapolsky Robert M (2004). Why zebras don't get ulcers. Henry Holt and Company, LLC. pp. 291–98. ISBN 0-8050-7369-8.
- ↑ Grant BF (1995). "Comorbidity between DSM-IV drug use disorders and major depression: Results of a national survey of adults". Journal of Substance Abuse 7 (4): 481–87. doi:10.1016/0899-3289(95)90017-9. PMID 8838629.
- ↑ Hallowell EM, Ratey JJ (2005). Delivered from distraction: Getting the most out of life with Attention Deficit Disorder. New York: Ballantine Books. pp. 253–55. ISBN 0-345-44231-8.
- ↑ Bair MJ, Robinson RL, Katon W, Kroenke K (2003). "Depression and Pain Comorbidity: A Literature Review". Archives of Internal Medicine 163 (20): 2433–45. doi:10.1001/archinte.163.20.2433. PMID 14609780.
- ↑ Swardfager W, Herrmann N, Marzolini S, Saleem M, Farber SB, Kiss A, Oh PI, Lanctôt KL (2011). "Major depressive disorder predicts completion, adherence, and outcomes in cardiac rehabilitation: a prospective cohort study of 195 patients with coronary artery disease.". Journal of Clinical Psychiatry 72 (9): 1181–8. doi:10.4088/jcp.09m05810blu. PMID 21208573.
- ↑ Schulman J and Shapiro BA (2008). "Depression and Cardiovascular Disease: What Is the Correlation?". Psychiatric Times 25 (9).
- ↑ Department of Health and Human Services (1999). "The fundamentals of mental health and mental illness" (PDF). Mental Health: A Report of the Surgeon General. Retrieved 11 November 2008.
- ↑ 27.0 27.1 27.2 Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R (July 2003). "Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene". Science 301 (5631): 386–89. Bibcode:2003Sci...301..386C. doi:10.1126/science.1083968. PMID 12869766.
- ↑ Haeffel GJ, Getchell M, Koposov RA, Yrigollen CM, Deyoung CG, Klinteberg BA, Oreland L, Ruchkin VV, Grigorenko EL (2008). "Association between polymorphisms in the dopamine transporter gene and depression: evidence for a gene-environment interaction in a sample of juvenile detainees" (PDF). Psychol Sci 19 (1): 62–9. doi:10.1111/j.1467-9280.2008.02047.x. PMID 18181793.
- ↑ Slavich GM (2004). "Deconstructing depression: A diathesis-stress perspective (Opinion)". APS Observer. Retrieved 11 November 2008.
- ↑ Schmahmann JD (2004). "Disorders of the cerebellum: ataxia, dysmetria of thought, and the cerebellar cognitive affective syndrome". J Neuropsychiatry Clin Neurosci 16 (3): 367–78. doi:10.1176/appi.neuropsych.16.3.367. PMID 15377747.
- ↑ Konarski JZ, McIntyre RS, Grupp LA, Kennedy SH (May 2005). "Is the cerebellum relevant in the circuitry of neuropsychiatric disorders?". J Psychiatry Neurosci 30 (3): 178–86. PMID 15944742.
- ↑ Schmahmann JD, Weilburg JB, Sherman JC (2007). "The neuropsychiatry of the cerebellum – insights from the clinic". Cerebellum 6 (3): 254–67. doi:10.1080/14734220701490995. PMID 17786822.
- ↑ Kendler KS, Gatz M, Gardner CO, Pedersen NL (2006). "A Swedish national twin study of lifetime major depression". American Journal of Psychiatry 163 (1): 109–14. doi:10.1176/appi.ajp.163.1.109. PMID 16390897.
- ↑ Schuckit MA, Tipp JE, Bergman M, Reich W, Hesselbrock VM, Smith TL (1997). "Comparison of induced and independent major depressive disorders in 2,945 alcoholics". Am J Psychiatry 154 (7): 948–57. doi:10.1176/ajp.154.7.948. PMID 9210745.
- ↑ 35.0 35.1 Professor Heather Ashton (2002). "Benzodiazepines: How They Work and How to Withdraw".
- ↑ Barlow 2005, p. 226
- ↑ Shah N, Eisner T, Farrell M, Raeder C (July–August 1999). "An overview of SSRIs for the treatment of depression" (PDF). Journal of the Pharmacy Society of Wisconsin. Retrieved 10 November 2008.
- ↑ 38.0 38.1 Nutt DJ (2008). "Relationship of neurotransmitters to the symptoms of major depressive disorder". Journal of Clinical Psychiatry. 69 Suppl E1: 4–7. PMID 18494537.
- ↑ 39.0 39.1 Krishnan V, Nestler EJ (October 2008). "The molecular neurobiology of depression". Nature 455 (7215): 894–902. Bibcode:2008Natur.455..894K. doi:10.1038/nature07455. PMC 2721780. PMID 18923511.
- ↑ Hirschfeld RM (2000). "History and evolution of the monoamine hypothesis of depression". Journal of Clinical Psychiatry. 61 Suppl 6: 4–6. PMID 10775017.
- ↑ Lacasse JR, Leo J (2005). "Serotonin and depression: A disconnect between the advertisements and the scientific literature". PLoS Med 2 (12): e392. doi:10.1371/journal.pmed.0020392. PMC 1277931. PMID 16268734. Retrieved 30 October 2008. Lay summary – Medscape (8 November 2005).
- ↑ Risch N, Herrell R, Lehner T, Liang KY, Eaves L, Hoh J, Griem A, Kovacs M, Ott J, Merikangas KR (June 2009). "Interaction between the serotonin transporter gene (5-HTTLPR), stressful life events, and risk of depression: a meta-analysis". JAMA 301 (23): 2462–71. doi:10.1001/jama.2009.878. PMC 2938776. PMID 19531786.
- ↑ Munafò MR, Durrant C, Lewis G, Flint J (February 2009). "Gene X environment interactions at the serotonin transporter locus". Biol. Psychiatry 65 (3): 211–9. doi:10.1016/j.biopsych.2008.06.009. PMID 18691701.
- ↑ Uher R, McGuffin P (January 2010). "The moderation by the serotonin transporter gene of environmental adversity in the etiology of depression: 2009 update". Mol. Psychiatry 15 (1): 18–22. doi:10.1038/mp.2009.123. PMID 20029411.
- ↑ Kempton MJ, Salvador Z, Munafò MR, Geddes JR, Simmons A, Frangou S, Williams SC (2011). "Structural Neuroimaging Studies in Major Depressive Disorder: Meta-analysis and Comparison With Bipolar Disorder". Arch Gen Psychiatry 68 (7): 675–90. doi:10.1001/archgenpsychiatry.2011.60. PMID 21727252. see also MRI database at www.depressiondatabase.org
- ↑ Arnone D, McIntosh AM, Ebmeier KP, Munafò MR, Anderson IM (July 2011). "Magnetic resonance imaging studies in unipolar depression: Systematic review and meta-regression analyses". Eur Neuropsychopharmacol 22 (1): 1–16. doi:10.1016/j.euroneuro.2011.05.003. PMID 21723712.
- ↑ Herrmann LL, Le Masurier M, Ebmeier KP (2008). "White matter hyperintensities in late life depression: a systematic review". Journal of Neurology, Neurosurgery, and Psychiatry 79 (6): 619–24. doi:10.1136/jnnp.2007.124651. PMID 17717021.
- ↑ Mayberg H (6 July 2007). "Brain pathway may underlie depression". Scientific American 17 (4): 26–31. Retrieved 13 September 2008.
- ↑ Sheline YI, Gado MH, Kraemer HC (2003). "Untreated depression and hippocampal volume loss". American Journal of Psychiatry 160 (8): 1516–18. doi:10.1176/appi.ajp.160.8.1516. PMID 12900317.
- ↑ Duman RS, Heninger GR, Nestler EJ (1997). "A molecular and cellular theory of depression". Archives of General Psychiatry 54 (7): 597–606. doi:10.1001/archpsyc.1997.01830190015002. PMID 9236543.
- ↑ Drevets WC, Savitz J, Trimble M (2008). "The subgenual anterior cingulate cortex in mood disorders". CNS Spectrums 13 (8): 663–81. PMC 2729429. PMID 18704022.
- ↑ Sen S, Duman R, Sanacora G (2008). "Serum brain-derived neurotrophic factor, depression, and antidepressant medications: Meta-analyses and implications". Biological Psychiatry 64 (6): 527–32. doi:10.1016/j.biopsych.2008.05.005. PMC 2597158. PMID 18571629.
- ↑ Monteleone P (2001). "Endocrine disturbances and psychiatric disorders". Current Opinion in Psychiatry (Lippincott Williams & Wilkins, Inc.) 14 (6): 605–10. doi:10.1097/00001504-200111000-00020. ISSN 0951-7367.
- ↑ 54.0 54.1 Cutter WJ, Norbury R, Murphy DG (2003). "Oestrogen, brain function, and neuropsychiatric disorders". Journal of Neurology, Neurosurgery and Psychiatry 74 (7): 837–40. doi:10.1136/jnnp.74.7.837. PMC 1738534. PMID 12810759.
- ↑ Douma SL, Husband C, O'Donnell ME, Barwin BN, Woodend AK (2005). "Estrogen-related Mood Disorders Reproductive Life Cycle Factors". Advances in Nursing Science 28 (4): 364–375. doi:10.1097/00012272-200510000-00008. PMID 16292022.
- ↑ Lasiuk GC, Hegadoren KM (2007). "The Effects of Estradiol on Central Serotonergic Systems and Its Relationship to Mood in Women". Biological Research for Nursing (2007), 9 (2): 147–160. doi:10.1177/1099800407305600. PMID 17909167.
- ↑ Dantzer R, O'Connor JC, Freund GG, Johnson RW, Kelley KW (2008). "From inflammation to sickness and depression: when the immune system subjugates the brain". Nature Reviews Neuroscience 9 (1): 46–56. doi:10.1038/nrn2297. PMC 2919277. PMID 18073775.
- ↑ Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, Lanctôt KL (2010). "A meta-analysis of cytokines in major depression". Biological Psychiatry 67 (5): 446–457. doi:10.1016/j.biopsych.2009.09.033. PMID 20015486.
- ↑ 59.0 59.1 Müller N, Myint AM, Schwarz MJ (February 2011). "Inflammatory biomarkers and depression". Neurotox Res 19 (2): 308–18. doi:10.1007/s12640-010-9210-2. PMID 20658274.
- ↑ 60.0 60.1 60.2 Raphael B (2000). "Unmet Need for Prevention". In Andrews G, Henderson S (eds). Unmet Need in Psychiatry:Problems, Resources, Responses. Cambridge University Press. pp. 138–39. ISBN 0-521-66229-X.
- ↑ Morris BH, Bylsma LM, Rottenberg J (September 2009). "Does emotion predict the course of major depressive disorder? A review of prospective studies". Br J Clin Psychol 48 (Pt 3): 255–73. doi:10.1348/014466508X396549. PMID 19187578.
- ↑ Sadock 2002, p. 541
- ↑ McCullough ME, Larson DB (1 June 1999). "Religion and depression: a review of the literature". Twin Research (Australian Academic Press) 2 (2): 126–136. doi:10.1375/136905299320565997. PMID 10480747.
- ↑ Dein, S (2006). "Religion, spirituality and depression: implications for research and treatment" (PDF). Primary Care and Community Psychiatry 11 (2): 67–72. doi:10.1185/135525706X121110. Retrieved 21 November 2008. Archived 21 October 2006 at the Wayback Machine
- ↑ Moreira-Almeida A, Neto FL, Koenig HG (September 2006). "Religiousness and mental health: a review". Rev. Bras. Psiquiatr. 28 (3): 242–50. doi:10.1590/S1516-44462006005000006. PMID 16924349.
- ↑ Warman DM, Beck AT (2003). "About treatment and supports: Cognitive behavioral therapy". National Alliance on Mental Illness (NAMI) website. Retrieved 17 October 2008.
- ↑ Beck 1987, pp. 10–15
- ↑ Beck 1987, p. 3
- ↑ Seligman, M (1975). "Depression". Helplessness: On depression, development and death. San Francisco, CA, USA: WH Freeman. pp. 75–106. ISBN 0-7167-0751-9.
- ↑ 70.0 70.1 Ma, K (2006). "Attachment theory in adult psychiatry. Part 1: Conceptualisations, measurement and clinical research findings". Advances in Psychiatric Treatment 12 (6): 440–449. doi:10.1192/apt.12.6.440. Retrieved 21 April 2010.
- ↑ 71.0 71.1 Barlow 2005, pp. 230–32
- ↑ Pinto A, Francis G (1993). "Cognitive correlates of depressive symptoms in hospitalized adolescents". Adolescence 28 (111): 661–72. PMID 8237551.
- ↑ Kanfer R, Zeiss AM (1983). "Depression, Interpersonal Standard Setting". Journal of Abnormal Psychology 92 (3): 319–29. doi:10.1037/0021-843X.92.3.319. PMID 6619407.
- ↑ Bandura A (1998). "Self-Efficacy". In Friedman H. Encyclopedia of mental health. San Diego: Academic Press. ISBN 0-12-226676-5. Retrieved 17 August 2008.
- ↑ Brown GW, Harris TO (2001) [1978]. Social Origins of Depression: A Study of Psychiatric Disorder in Women. Routledge. ISBN 0-415-20268-X.
- ↑ Hinrichsen GA, Emery EE (2006). "Interpersonal factors and late-life depression". Clinical Psychology: Science and Practice 12 (3): 264–75. doi:10.1093/clipsy/bpi027. (subscription required (help)).
- ↑ 77.0 77.1 Carhart-Harris RL, Mayberg HS, Malizia AL, Nutt D (2008). "Mourning and melancholia revisited: Correspondences between principles of Freudian metapsychology and empirical findings in neuropsychiatry". Annals of General Psychiatry 7: 9. doi:10.1186/1744-859X-7-9. PMC 2515304. PMID 18652673.
- ↑ 78.0 78.1 Freud, S (1984). "Mourning and Melancholia". In Richards A. 11.On Metapsychology: The Theory of Psycholoanalysis. Aylesbury, Bucks: Pelican. pp. 245–69. ISBN 0-14-021740-1.
- ↑ 79.0 79.1 79.2 79.3 Radden, J (2003). "Is this dame melancholy? Equating today's depression and past melancholia". Philosophy, Psychiatry, & Psychology 10 (1): 37–52. doi:10.1353/ppp.2003.0081.
- ↑ Frankl VE (2000). Man's search for ultimate meaning. New York, NY, USA: Basic Books. pp. 139–40. ISBN 0-7382-0354-8.
- ↑ Geppert C.M.A. (2006). "Damage control". Psychiatric Times. Retrieved 12 November 2014.
- ↑ May 1994, p. 133
- ↑ Heim C, Newport DJ, Mletzko T, Miller AH, Nemeroff CB (2008). "The link between childhood trauma and depression: insights from HPA axis studies in humans". Psychoneuroendocrinology 33 (6): 693–710. doi:10.1016/j.psyneuen.2008.03.008. PMID 18602762.
- ↑ Kessler RC (1997). "The effects of stressful life events on depression". Annual revue of Psychology 48: 191–214. doi:10.1146/annurev.psych.48.1.191. PMID 9046559.
- ↑ Kendler KS, Hettema JM, Butera F, Gardner CO, Prescott CA (2003). "Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety". Archives of General Psychiatry 60 (8): 789–796. doi:10.1001/archpsyc.60.8.789. PMID 12912762.
- ↑ Slavich GM, Thornton T, Torres LD, Monroe SM, Gotlib IH (2009). "Targeted rejection predicts hastened onset of major depression". Journal of Social and Clinical Psychology 28: 223–243. doi:10.1521/jscp.2009.28.2.223. PMC 2847269. PMID 20357895.
- ↑ Monroe SM, Slavich GM, Torres LD, Gotlib IH (2007). "Major life events and major chronic difficulties are differentially associated with history of major depressive episodes". Journal of Abnormal Psychology 116 (1): 116–124. doi:10.1037/0021-843X.116.1.116. PMID 17324022.
- ↑ Sadock 2002, p. 540
- ↑ Vilhjalmsson R (1993). "Life stress, social support and clinical depression: A reanalysis of the literature". Social Science & Medicine 37 (3): 331–42. doi:10.1016/0277-9536(93)90264-5. PMID 8356482.
- ↑ Kim D (2008). "Blues from the neighborhood? Neighborhood characteristics and depression". Epidemiologic reviews 30: 101–17. doi:10.1093/epirev/mxn009. PMID 18753674.
- ↑ Bonde JP (2008). "Psychosocial factors at work and risk of depression: A systematic review of the epidemiological evidence". Journal of Occupational and Environmental Medicine 65 (7): 438–45. doi:10.1136/oem.2007.038430. PMID 18417557.
- ↑ Cox WTL, Abramson LY, Devine PG, Hollon SD (2012). "Stereotypes, Prejudice, and Depression: The Integrated Perspective". Perspectives on Psychological Science 7 (5): 427–449. doi:10.1177/1745691612455204.
- ↑ Panksepp J, Moskal JR, Panksepp JB, Kroes RA (2002). "Comparative approaches in evolutionary psychology: Molecular neuroscience meets the mind" (PDF). Neuroendocrinology Letters 23 (Supplement 4): 105–15. PMID 12496741.
- ↑ Sloman L, Gilbert P, Hasey G (2003). "Evolved mechanisms in depression: The role and interaction of attachment and social rank in depression". Journal of Affective Disorders 74 (2): 107–21. doi:10.1016/S0165-0327(02)00116-7. PMID 12706512.
- ↑ Tooby, J, Cosmides, L (2005). Conceptual foundations of evolutionary psychology. In D. M. Buss (Ed.), The Handbook of Evolutionary Psychology (PDF). Hoboken, NJ: Wiley & Sons. pp. 5–67.
- ↑ Carey TJ (2005). "Evolution, depression and counselling". Counselling Psychology Quarterly 18 (3): 215–22. doi:10.1080/09515070500304508.
- ↑ Mashman, RC (1997). "An evolutionary view of psychic misery". Journal of Social Behaviour & Personality 12: 979–99. ISSN 0886-1641.
- ↑ Cottencin O (December 2009). "[Severe depression and addictions]". Encephale (in French). 35 Suppl 7: S264–8. doi:10.1016/S0013-7006(09)73483-9. PMID 20141784.
- ↑ Falk DE, Yi HY, Hilton ME (2008). "Age of onset and temporal sequencing of lifetime DSM-IV alcohol use disorders relative to comorbid mood and anxiety disorders". Drug Alcohol Depend 94 (1–3): 234–45. doi:10.1016/j.drugalcdep.2007.11.022. PMC 2386955. PMID 18215474.
- ↑ 100.0 100.1 Boden JM, Fergusson DM (May 2011). "Alcohol and depression". Addiction 106 (5): 906–14. doi:10.1111/j.1360-0443.2010.03351.x. PMID 21382111.
- ↑ Kelley KW, Dantzer R (June 2011). "Alcoholism and inflammation: neuroimmunology of behavioral and mood disorders". Brain Behav. Immun. 25 Suppl 1: S13–20. doi:10.1016/j.bbi.2010.12.013. PMID 21193024.
- ↑ Semple, David; Roger Smyth; Jonathan Burns; Rajan Darjee; Andrew McIntosh (2007) [2005]. "13". Oxford Handbook of Psychiatry. United Kingdom: Oxford University Press. p. 540. ISBN 0-19-852783-7.
- ↑ Collier, Judith; Longmore, Murray (2003). "4". In Scally, Peter. Oxford Handbook of Clinical Specialties (6 ed.). Oxford University Press. p. 366. ISBN 978-0-19-852518-9.
- ↑ Janicak, Philip G.; Marder, Stephen R.; Pavuluri, Mani N. (2011). Principles and practice of psychopharmacotherap. Philadelphia: Wolters Kluwer Health/Lippincott Williams Wilkins. pp. 507–508. ISBN 978-1-60547-565-3.
- ↑ Johnson, Bankole A. (2011). Addiction medicine : science and practic. New York: Springer. pp. 301–303. ISBN 978-1-4419-0337-2.
- ↑ Marshall BD, Werb D (June 2010). "Health outcomes associated with methamphetamine use among young people: a systematic review". Addiction 105 (6): 991–1002. doi:10.1111/j.1360-0443.2010.02932.x. PMID 20659059.
- ↑ Kaufmann IM (1 September 1993). "Rural psychiatric services. A collaborative model". Canadian Family Physician 39: 1957–61. PMC 2379905. PMID 8219844.
- ↑ "Call for action over Third World depression". BBC News (Health). British Broadcasting Corporation (BBC). 1 November 1999. Retrieved 11 October 2008.
- ↑ Zimmerman M, Chelminski I, Posternak M (September 2004). "A Review of Studies of the Hamilton Depression Rating Scale in Healthy Controls: Implications for the Definition of Remission in Treatment Studies Of Depression". J Nerv Ment Dis 192 (9): 595–601. doi:10.1097/01.nmd.0000138226.22761.39. PMID 15348975.
- ↑ McPherson A, Martin CR (February 2010). "A Narrative Review of the Beck Depression Inventory (BDI) and Implications for its Use in an Alcohol-Dependent Population". J Psychiatr Ment Health Nurs 17 (1): 19–30. doi:10.1111/j.1365-2850.2009.01469.x. PMID 20100303.
- ↑ 111.0 111.1 Sharp LK, Lipsky MS (2002). "Screening for depression across the lifespan: a review of measures for use in primary care settings". American Family Physician 66 (6): 1001–8. PMID 12358212.
- ↑ Gilbody S, House AO, Sheldon TA (2005). "Screening and case finding instruments for depression". Cochrane Database of Systematic Reviews (4): CD002792. doi:10.1002/14651858.CD002792.pub2. PMID 16235301.
- ↑ Cepoiu M, McCusker J, Cole MG, Sewitch M, Belzile E, Ciampi A (2008). "Recognition of depression by non-psychiatric physicians—a systematic literature review and meta-analysis". J Gen Intern Med 23 (1): 25–36. doi:10.1007/s11606-007-0428-5. PMC 2173927. PMID 17968628.
- ↑ 114.0 114.1 Dale J, Sorour E, Milner G (2008). "Do psychiatrists perform appropriate physical investigations for their patients? A review of current practices in a general psychiatric inpatient and outpatient setting". Journal of Mental Health 17 (3): 293–98. doi:10.1080/09638230701498325.
- ↑ Orengo CA, Fullerton G, Tan R (2004). "Male depression: A review of gender concerns and testosterone therapy". Geriatrics 59 (10): 24–30. PMID 15508552.
- ↑ Reid LM, Maclullich AM (2006). "Subjective memory complaints and cognitive impairment in older people". Dementia and geriatric cognitive disorders 22 (5–6): 471–85. doi:10.1159/000096295. PMID 17047326.
- ↑ Katz IR (1998). "Diagnosis and treatment of depression in patients with Alzheimer's disease and other dementias". The Journal of clinical psychiatry. 59 Suppl 9: 38–44. PMID 9720486.
- ↑ Wright SL, Persad C (2007). "Distinguishing between depression and dementia in older persons: Neuropsychological and neuropathological correlates". Journal of geriatric psychiatry and neurology 20 (4): 189–98. doi:10.1177/0891988707308801. PMID 18004006.
- ↑ Sadock 2002, p. 108
- ↑ Sadock 2002, p. 260
- ↑ Hahn T, Marquand AF, Ehlis AC, Dresler T, Kittel-Schneider S, Jarczok TA, Lesch KP, Jakob PM, Mourao-Miranda J, Brammer MJ, Fallgatter AJ (December 2010). "Integrating Neurobiological Markers of Depression". Arch. Gen. Psychiatry 68 (4): 361–368. doi:10.1001/archgenpsychiatry.2010.178. PMID 21135315. Retrieved 1 April 2011.
- ↑ 122.0 122.1 122.2 "Mental and behavioural disorders: Mood [affective] disorders". World Health Organization. 2010. Retrieved 8 November 2008.
- ↑ Sadock 2002, p. 288
- ↑ American Psychiatric Association 2000a, p. xxix
- ↑ 125.0 125.1 Gruenberg, A.M., Goldstein, R.D., Pincus, H.A. (2005). "Classification of Depression: Research and Diagnostic Criteria: DSM-IV and ICD-10" (PDF). Biology of Depression: From Novel Insights to Therapeutic Strategies (eds J. Licinio and M.-L. Wong). Wiley-VCH Verlag GmbH. doi:10.1002/9783527619672.ch1. Retrieved 30 October 2008.
- ↑ "The ICD-10 Classification of Mental and Behavioural Disorders: Clinical descriptions and diagnostic guidelines" (PDF). World Health Organization. 2010. Retrieved 12 November 2014.
- ↑ The ICD-10 classification of mental and behavioral disorders. Clinical description and diagnostic guideline. Geneva: World Health Organization, 1992
- ↑ American Psychiatric Association 2000a
- ↑ American Psychiatric Association 2000a, p. 345
- ↑ American Psychiatric Association 2000a, p. 372
- ↑ Parker 1996, p. 173
- ↑ American Psychiatric Association 2000a, p. 352
- ↑ Wakefield JC, Schmitz MF, First MB, Horwitz AV (2007). "Extending the bereavement exclusion for major depression to other losses: Evidence from the National Comorbidity Survey". Archives of General Psychiatry 64 (4): 433–40. doi:10.1001/archpsyc.64.4.433. PMID 17404120. Lay summary – The Washington Post (3 April 2007).
- ↑ Kendler KS, Gardner CO (1 February 1998). "Boundaries of major depression: An evaluation of DSM-IV criteria". American Journal of Psychiatry 155 (2): 172–77. PMID 9464194.
- ↑ 135.0 135.1 Sadock 2002, p. 552
- ↑ American Psychiatric Association 2000a, p. 778
- ↑ Carta MG, Altamura AC, Hardoy MC, Pinna F, Medda S, Dell'Osso L, Carpiniello B, Angst J (2003). "Is recurrent brief depression an expression of mood spectrum disorders in young people?". European Archives of Psychiatry and Clinical Neuroscience 253 (3): 149–53. doi:10.1007/s00406-003-0418-5. PMID 12904979.
- ↑ Rapaport MH, Judd LL, Schettler PJ, Yonkers KA, Thase ME, Kupfer DJ, Frank E, Plewes JM, Tollefson GD, Rush AJ (2002). "A descriptive analysis of minor depression". American Journal of Psychiatry 159 (4): 637–43. doi:10.1176/appi.ajp.159.4.637. PMID 11925303.
- ↑ 139.0 139.1 American Psychiatric Association 2000a, p. 355
- ↑ American Psychiatric Association 2000a, pp. 419–20
- ↑ American Psychiatric Association 2000a, pp. 421–22
- ↑ American Psychiatric Association 2000a, pp. 417–18
- ↑ Nonacs, Ruta M (4 December 2007). "Postpartum depression". eMedicine. Retrieved 30 October 2008.
- ↑ American Psychiatric Association 2000a, p. 425
- ↑ Akiskal HS, Benazzi F (2006). "The DSM-IV and ICD-10 categories of recurrent [major] depressive and bipolar II disorders: Evidence that they lie on a dimensional spectrum". Journal of Affective Disorders 92 (1): 45–54. doi:10.1016/j.jad.2005.12.035. PMID 16488021.
- ↑ "Major Depressive Episode". psychnet-uk.com. Retrieved 16 July 2010.
- ↑ 147.0 147.1 Muñoz RF, Beardslee WR, Leykin Y (May–June 2012). "Major depression can be prevented". The American Psychologist 67 (4): 285–95. doi:10.1037/a0027666. PMID 22583342.
- ↑ Cuijpers, P (20 September 2012). Prevention and early treatment of mental ill-health (PDF). PSYCHOLOGY FOR HEALTH: Contributions to Policy Making, Brussels.
- ↑ 149.0 149.1 Cuijpers P, van Straten A, Smit F, Mihalopoulos C, Beekman A (2008). "Preventing the onset of depressive disorders: a meta-analytic review of psychological interventions". Am J Psychiatry 165 (10): 1272–80. doi:10.1176/appi.ajp.2008.07091422. PMID 18765483.
- ↑ Griffiths, K.M.; Farrer, L.; Christensen, H. (2010). "The efficacy of internet interventions for depression and anxiety disorders: a review of randomised controlled trials" (PDF). Medical Journal of Australia 192 (11): 4–11. Retrieved 12 November 2014.
- ↑ Jané-Llopis E; Hosman C; Jenkins R; Anderson P. (2003). "Predictors of efficacy in depression prevention programmes" (PDF). British Journal of Psychiatry. Retrieved 2 April 2009.
- ↑ Cuijpers P, Muñoz RF, Clarke GN, Lewinsohn PM (2009). "Psychoeducational treatment and prevention of depression: the "Coping with Depression" course thirty years later". Clinical Psychology Review 29 (5): 449–458. doi:10.1016/j.cpr.2009.04.005. PMID 19450912.
- ↑ "Depression". National Institute for Health and Care Excellence. December 2004. Archived from the original on 15 November 2008. Retrieved 20 March 2013.
- ↑ "PsychiatryOnline | APA Practice Guidelines | Practice Guideline for the Treatment of Patients With Major Depressive Disorder, Third Edition".
- ↑ Patel V, Araya R, Bolton P (2004). "Editorial: Treating depression in the developing world". Tropical Medicine & International Health 9 (5): 539–41. doi:10.1111/j.1365-3156.2004.01243.x. PMID 15117296. (subscription required (help)).
- ↑ Cox GR, Callahan P, Churchill R, Hunot V, Merry SN, Parker AG, Hetrick SE (30 November 2014). "Psychological therapies versus antidepressant medication, alone and in combination for depression in children and adolescents.". The Cochrane database of systematic reviews 11: CD008324. doi:10.1002/14651858.CD008324.pub3. PMID 25433518.
- ↑ Thase ME (1999). "When are psychotherapy and pharmacotherapy combinations the treatment of choice for major depressive disorder?". Psychiatric Quarterly 70 (4): 333–46. doi:10.1023/A:1022042316895. PMID 10587988.
- ↑ Cordes, J. (2013). "Depression". Encyclopedia of Sciences and Religions. p. 610. doi:10.1007/978-1-4020-8265-8_301. ISBN 978-1-4020-8264-1.
- ↑ Khan A, Faucett J, Lichtenberg P, Kirsch I, Brown WA (30 July 2012). "A Systematic Review of Comparative Efficacy of Treatments and Controls for Depression". PLOS ONE 7 (7): e41778. doi:10.1371/journal.pone.0041778. PMC 3408478. PMID 22860015.
- ↑ Childhood Depression. abct.org. Last updated: 30 July 2010
- ↑ NICE (2005). NICE guidelines: Depression in children and adolescents. London: NICE. p. 5. ISBN 1-84629-074-0. Retrieved 16 August 2008.
- ↑ Wilson KC, Mottram PG, Vassilas CA (2008). "Psychotherapeutic treatments for older depressed people". Cochrane Database of Systematic Reviews 23 (1): CD004853. doi:10.1002/14651858.CD004853.pub2. PMID 18254062.
- ↑ Cuijpers P, van Straten A, Smit F (2006). "Psychological treatment of late-life depression: a meta-analysis of randomized controlled trials". International Journal of Geriatric Psychiatry 21 (12): 1139–49. doi:10.1002/gps.1620. PMID 16955421.
- ↑ Dobson KS (1989). "A meta-analysis of the efficacy of cognitive therapy for depression". J Consult Clin Psychol 57 (3): 414–9. doi:10.1037/0022-006X.57.3.414. PMID 2738214.
- ↑ Roth, Anthony; Fonagy, Peter (2005) [1996]. What Works for Whom? Second Edition: A Critical Review of Psychotherapy Research. Guilford Press. p. 78. ISBN 1-59385-272-X.
- ↑ Weersing VR, Walker PN (2008). "Review: Cognitive behavioural therapy for adolescents with depression". Evidence-Based Mental Health 11 (3): 76. doi:10.1136/ebmh.11.3.76. PMID 18669678. Retrieved 27 November 2008.
- ↑ Harrington R, Whittaker J, Shoebridge P, Campbell F (1998). "Systematic review of efficacy of cognitive behaviour therapies in childhood and adolescent depressive disorder". BMJ 325 (7358): 229–30. doi:10.1136/bmj.325.7358.229. PMC 28555. PMID 9596592.
- ↑ Becker SJ (2008). "Cognitive-Behavioral Therapy for Adolescent Depression: Processes of Cognitive Change". Psychiatric Times 25 (14).
- ↑ Almeida AM, Lotufo Neto F (2003). "Cognitive-behavioral therapy in prevention of depression relapses and recurrences: a review". Revista brasileira de psiquiatria (Sao Paulo, Brazil : 1999) 25 (4): 239–44. PMID 15328551.
- ↑ Paykel ES (2007). "Cognitive therapy in relapse prevention in depression". The international journal of neuropsychopharmacology / official scientific journal of the Collegium Internationale Neuropsychopharmacologicum (CINP) 10 (1): 131–6. doi:10.1017/S1461145706006912. PMID 16787553.
- ↑ Beck 1987, p. 10
- ↑ Coelho HF, Canter PH, Ernst E (2007). "Mindfulness-based cognitive therapy: Evaluating current evidence and informing future research". Journal of Consulting and Clinical Psychology 75 (6): 1000–05. doi:10.1037/0022-006X.75.6.1000. PMID 18085916.
- ↑ Khoury B, Lecomte T, Fortin G, Masse M, Therien P, Bouchard V, Chapleau MA, Paquin K, Hofmann SG (August 2013). "Mindfulness-based therapy: a comprehensive meta-analysis". Clin Psychol Rev. 33 (6): 763–71. doi:10.1016/j.cpr.2013.05.005. PMID 23796855.
- ↑ Jain FA, Walsh RN, Eisendrath SJ et al. (2014). "Critical Analysis of the Efficacy of Meditation Therapies for Acute and Subacute Phase Treatment of Depressive Disorders: A systematic Review". Psychosomatics 56: 297–302. doi:10.1016/j.psym.2014.10.007.
- ↑ Simkin DR, Black NB (July 2014). "Meditation and mindfulness in clinical practice.". Child and adolescent psychiatric clinics of North America 23 (3): 487–534. doi:10.1016/j.chc.2014.03.002. PMID 24975623.
- ↑ Dworetzky J (1997). Psychology. Pacific Grove, CA, USA: Brooks/Cole Pub. Co. p. 602. ISBN 0-314-20412-1.
- ↑ Doidge N, Simon B, Lancee WJ, First M, Brunshaw J, Brauer L, Grant DC, Stevens A, Oldham JM, Mosher P (2002). "Psychoanalytic patients in the US, Canada, and Australia: II. A DSM-III-R validation study". Journal of the American Psychoanalytic Association 50 (2): 615–27. doi:10.1177/00030651020500021101. PMID 12206545.
- ↑ Barlow 2005, p. 20
- ↑ de Maat S, Dekker J, Schoevers R, van Aalst G, Gijsbers-van Wijk C, Hendriksen M, Kool S, Peen J, Van R, de Jonghe F (2007). "Short Psychodynamic Supportive Psychotherapy, antidepressants, and their combination in the treatment of major depression: A mega-analysis based on three Randomized Clinical Trials". Depression and Anxiety 25 (7): 565–74. doi:10.1002/da.20305. PMID 17557313.
- ↑ Blair RG (2004). "Helping older adolescents search for meaning in depression". Journal of Mental Health Counseling. Retrieved 6 November 2008.
- ↑ The sertraline prescriptions were calculated as a total of prescriptions for Zoloft and generic Sertraline using data from the charts for generic and brand name drugs, see: Verispan (18 February 2008). "Top 200 Generic Drugs by Units in 2007" (PDF). Drug Topics. Retrieved 30 March 2008. and Verispan (18 February 2008). "Top 200 Brand Drugs by Units in 2007" (PDF). Drug Topics. Retrieved 30 March 2008.
- ↑ Kirsch I, Moore TJ, Scoboria A, Nicholls SS (2002). "The emperor's new drugs: An analysis of antidepressant medication data submitted to the U.S. Food and Drug Administration". Prevention & Treatment 5. doi:10.1037/1522-3736.5.1.523a.
- ↑ "The treatment and management of depression in adults" (PDF). NICE. October 2009. Retrieved 12 November 2014.
- ↑ Leucht C, Huhn M, Leucht S (2012). Leucht, C, ed. "Amitriptyline versus placebo for major depressive disorder". Cochrane Database of Systematic Reviews 12: CD009138. doi:10.1002/14651858.CD009138.pub2. PMID 23235671.
- ↑ 185.0 185.1 Karasu TB, Gelenberg A, Merriam A, Wang P (April 2000). "Practice Guideline for the Treatment of Patients With Major Depressive Disorder (Second Edition)". Am J Psychiatry 157 (4 Suppl): 1–45. PMID 10767867.; Third edition doi:10.1176/appi.books.9780890423363.48690
- ↑ Thase ME (2006). "Preventing relapse and recurrence of depression: a brief review of therapeutic options". CNS spectrums 11 (12 Suppl 15): 12–21. PMID 17146414.
- ↑ 187.0 187.1 Royal Pharmaceutical Society of Great Britain 2008, p. 204
- ↑ Whooley MA, Simon GE (2000). "Managing Depression in Medical Outpatients". New England Journal of Medicine 343 (26): 1942–50. doi:10.1056/NEJM200012283432607. PMID 11136266. Retrieved 11 November 2008.
- ↑ Zisook S, Rush AJ, Haight BR, Clines DC, Rockett CB (2006). "Use of bupropion in combination with serotonin reuptake inhibitors". Biological Psychiatry 59 (3): 203–10. doi:10.1016/j.biopsych.2005.06.027. PMID 16165100.
- ↑ Papakostas GI, Thase ME, Fava M, Nelson JC, Shelton RC (2007). "Are antidepressant drugs that combine serotonergic and noradrenergic mechanisms of action more effective than the selective serotonin reuptake inhibitors in treating major depressive disorder? A meta-analysis of studies of newer agents". Biological Psychiatry 62 (11): 1217–27. doi:10.1016/j.biopsych.2007.03.027. PMID 17588546.
- ↑ Gordon Duff (31 May 2006). "Updated prescribing advice for venlafaxine (Efexor/Efexor XL)". Medicines and Healthcare products Regulatory Agency (MHRA).
- ↑ 192.0 192.1 "Depression in children and young people: Identification and management in primary, community and secondary care" (PDF). NHS National Institute for Health and Clinical Excellence. 2005. Retrieved 12 November 2014.
- ↑ Mayers AG, Baldwin DS (2005). "Antidepressants and their effect on sleep". Human Psychopharmacology 20 (8): 533–59. doi:10.1002/hup.726. PMID 16229049.
- ↑ Tsapakis EM, Soldani F, Tondo L, Baldessarini RJ (2008). "Efficacy of antidepressants in juvenile depression: meta-analysis". Br J Psychiatry 193 (1): 10–7. doi:10.1192/bjp.bp.106.031088. PMID 18700212.
- ↑ Nelson JC, Devanand DP (April 2011). "A systematic review and meta-analysis of placebo-controlled antidepressant studies in people with depression and dementia". Journal of the American Geriatrics Society 59 (4): 577–85. doi:10.1111/j.1532-5415.2011.03355.x. PMID 21453380.
- ↑ Palmer BF, Gates JR, Lader M (2003). "Causes and Management of Hyponatremia". Annals of Pharmacotherapy 37 (11): 1694–702. doi:10.1345/aph.1D105. PMID 14565794.
- ↑ Guaiana G, Barbui C, Hotopf M (2007). "Amitriptyline for depression". Cochrane Database of Systematic Reviews 18 (3): 11–7. doi:10.1002/14651858.CD004186.pub2. PMID 17636748.
- ↑ Anderson IM (2000). "Selective serotonin reuptake inhibitors versus tricyclic antidepressants: A meta-analysis of efficacy and tolerability". Journal of Affective Disorders 58 (1): 19–36. doi:10.1016/S0165-0327(99)00092-0. PMID 10760555.
- ↑ Krishnan KR (2007). "Revisiting monoamine oxidase inhibitors". Journal of Clinical Psychiatry. 68 Suppl 8: 35–41. PMID 17640156.
- ↑ Bonnet U (2003). "Moclobemide: therapeutic use and clinical studies". CNS Drug Rev 9 (1): 97–140. doi:10.1111/j.1527-3458.2003.tb00245.x. PMID 12595913.
- ↑ Hammad TA (16 August 2004). "Review and evaluation of clinical data. Relationship between psychiatric drugs and pediatric suicidality" (PDF). FDA. pp. 42; 115. Retrieved 29 May 2008.
- ↑ 202.0 202.1 Hetrick S, Merry S, McKenzie J, Sindahl P, Proctor M (2007). "Selective serotonin reuptake inhibitors (SSRIs) for depressive disorders in children and adolescents". Cochrane Database of Systematic Reviews (3): CD004851. doi:10.1002/14651858.CD004851.pub2. PMID 17636776.
- ↑ Gunnell D, Saperia J, Ashby D (2005). "Selective serotonin reuptake inhibitors (SSRIs) and suicide in adults: meta-analysis of drug company data from placebo controlled, randomised controlled trials submitted to the MHRA's safety review". BMJ 330 (7488): 385. doi:10.1136/bmj.330.7488.385. PMC 549105. PMID 15718537.
- ↑ Fergusson D, Doucette S, Glass KC, Shapiro S, Healy D, Hebert P, Hutton B (2005). "Association between suicide attempts and selective serotonin reuptake inhibitors: systematic review of randomised controlled trials". BMJ 330 (7488): 396. doi:10.1136/bmj.330.7488.396. PMC 549110. PMID 15718539.
- ↑ Stone M, Laughren T, Jones ML, Levenson M, Holland PC, Hughes A, Hammad TA, Temple R, Rochester G (11 August 2009). "Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration". BMJ (Clinical research ed.) 339: b2880. doi:10.1136/bmj.b2880. PMC 2725270. PMID 19671933.
- ↑ "FDA Proposes New Warnings About Suicidal Thinking, Behavior in Young Adults Who Take Antidepressant Medications". FDA. 2 May 2007. Retrieved 29 May 2008.
- ↑ Medics and Foods Department. Pharmaceuticals and Medical Devices Safety Information (PDF) (Report). 261 (in Japanese). Ministry of Health, Labour and Welfare (Japan).
- ↑ Sublette ME, Ellis SP, Geant AL, Mann JJ (September 2011). "Meta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression". J Clin Psychiatry 72 (12): 1577–84. doi:10.4088/JCP.10m06634. PMC 3534764. PMID 21939614.
- ↑ Bloch MH, Hannestad J (September 2011). "Omega-3 fatty acids for the treatment of depression: systematic review and meta-analysis". Mol Psychiatry 17 (12): 1272–82. doi:10.1038/mp.2011.100. PMC 3625950. PMID 21931319.
- ↑ Cipriani A, Hawton K, Stockton S, Geddes JR (27 June 2013). "Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis". BMJ 346 (jun27 4): f3646–f3646. doi:10.1136/bmj.f3646. PMID 23814104.
- ↑ Nolen-Hoeksema, Susan. (2014) "Treatment of Mood Disorders". In (6th ed.) Abnormal Psychology p. 196. New York: McGraw-Hill. ISBN 9780078035388.
- ↑ Gelenberg, Alan J.; Freeman, Marlene P.; Markowitz, John C. "Practice Guideline for the Treatment of Patients with Major Depressive Disorder. 3rd edition." (PDF). American Psychiatric Association (APA). Retrieved 3 November 2014.
- ↑ Rudorfer, MV, Henry, ME, Sackeim, HA (2003). "Electroconvulsive therapy". In A Tasman, J Kay, JA Lieberman (eds) Psychiatry, Second Edition. Chichester: John Wiley & Sons Ltd, 1865–1901.
- ↑ Beloucif S. Informed consent for special procedures: electroconvulsive therapy and psychosurgery. Curr Opin Anaesthesiol. 2013 doi:10.1097/ACO.0b013e32835e7380 PMID 23385317
- ↑ 215.0 215.1 215.2 FDA. FDA Executive Summary. Prepared for the 27–28 January 2011 meeting of the Neurological Devices Panel Meeting to Discuss the Classification of Electroconvulsive Therapy Devices (ECT). Quote, p38: "Three major practice guidelines have been published on ECT. These guidelines include: APA Task Force on ECT (2001); Third report of the Royal College of Psychiatrists’ Special Committee on ECT (2004); National Institute for Health and Clinical Excellence (NICE 2003; NICE 2009). There is significant agreement between the three sets of recommendations."
- ↑ Dierckx B, Heijnen WT, van den Broek WW, Birkenhäger TK; Heijnen, WT; Van Den Broek, WW; Birkenhäger, TK (2012). "Efficacy of electroconvulsive therapy in bipolar versus unipolar major depression: A meta-analysis". Bipolar Disorders 12 (2): 146–150. doi:10.1111/j.1399-5618.2012.00997.x. PMID 22420590.
- ↑ Jelovac A et al. (Nov 2013). "Relapse following successful electroconvulsive therapy for major depression: a meta-analysis". Neuropsychopharmacology 38 (12): 2467–74. doi:10.1038/npp.2013.149. PMID 23774532.
- ↑ Surgeon General (1999). Mental Health: A Report of the Surgeon General, chapter 4.
- ↑ American Psychiatric Association; Committee on Electroconvulsive Therapy; Richard D. Weiner (chairperson) et al. (2001). The practice of electroconvulsive therapy: recommendations for treatment, training, and privileging (2nd ed.). Washington, DC: American Psychiatric Publishing. ISBN 978-0-89042-206-9.
- ↑ Pompili M et al. (Dec 2014). "Electroconvulsive treatment during pregnancy: a systematic review". Expert Rev Neurother 14 (12): 1377–90. doi:10.1586/14737175.2014.972373. PMID 25346216.
- ↑ http://psychcentral.com/lib/5-outdated-beliefs-about-ect/00011255
- ↑ Abbott CC, et al A review of longitudinal electroconvulsive therapy: neuroimaging investigations. J Geriatr Psychiatry Neurol. 2014 Mar;27(1):33–46. Review. doi:10.1177/0891988713516542 PMID 24381234
- ↑ Golden RN, Gaynes BN, Ekstrom RD, Hamer RM, Jacobsen FM, Suppes T, Wisner KL, Nemeroff CB (April 2005). "The efficacy of light therapy in the treatment of mood disorders: a review and meta-analysis of the evidence". American Journal of Psychiatry 162 (4): 656–62. doi:10.1176/appi.ajp.162.4.656. PMID 15800134.
- ↑ Tuunainen A, Kripke DF, Endo T (2004). Tuunainen, Arja, ed. "Light therapy for non-seasonal depression". Cochrane Database Syst Rev (2): CD004050. doi:10.1002/14651858.CD004050.pub2. PMID 15106233.
- ↑ Giedke H, Schwärzler F (2002). "Therapeutic use of sleep deprivation in depression". Sleep Medicine Reviews 6 (5): 361–77. doi:10.1053/smrv.2002.0235. PMID 12531127.
- ↑ "Management of depression in primary and secondary care" (PDF). National Clinical Practice Guideline Number 23. National Institute for Health and Clinical Excellence. 2007. Retrieved 4 November 2008.
- ↑ 227.0 227.1 Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR, McMurdo M, Mead GE (12 September 2013). Mead, Gillian E, ed. "Exercise for depression". Cochrane Database of Systematic Reviews 9: CD004366. doi:10.1002/14651858.CD004366.pub6. PMID 24026850.
- ↑ Bridle C, Spanjers K, Patel S, Atherton NM, Lamb SE (September 2012). "Effect of exercise on depression severity in older people: systematic review and meta-analysis of randomised controlled trials". Br J Psychiatry 201 (3): 180–5. doi:10.1192/bjp.bp.111.095174. PMID 22945926.
- ↑ Taylor G, McNeill A, Girling A, Farley A, Lindson-Hawley N, Aveyard P (13 February 2014). "Change in mental health after smoking cessation: systematic review and meta-analysis". BMJ 348 (feb13 1): g1151–g1151. doi:10.1136/bmj.g1151. PMC 3923980. PMID 24524926.
- ↑ Nieuwenhuijsen K, Faber B, Verbeek JH, Neumeyer-Gromen A, Hees HL, Verhoeven AC et al. (2014). "Interventions to improve return to work in depressed people". The Cochrane Database of Systematic Reviews 12: CD006237. doi:10.1002/14651858.CD006237.pub3. PMID 25470301.
- ↑ Posternak MA, Miller I (2001). "Untreated short-term course of major depression: A meta-analysis of outcomes from studies using wait-list control groups". Journal of Affective Disorders 66 (2–3): 139–46. doi:10.1016/S0165-0327(00)00304-9. PMID 11578666.
- ↑ Posternak MA, Solomon DA, Leon AC, Mueller TI, Shea MT, Endicott J, Keller MB (2006). "The naturalistic course of unipolar major depression in the absence of somatic therapy". Journal of Nervous and Mental Disease 194 (5): 324–29. doi:10.1097/01.nmd.0000217820.33841.53. PMID 16699380.
- ↑ Fava GA, Park SK, Sonino N (2006). "Treatment of recurrent depression.". Expert Review of Neurotherapeutics 6 (11): 1735–1740. doi:10.1586/14737175.6.11.1735. PMID 17144786.
- ↑ Limosin F, Mekaoui L, Hautecouverture S (2007). "Stratégies thérapeutiques prophylactiques dans la dépression unipolaire [Prophylactic treatment for recurrent major depression]". La Presse Médicale 36 (11-C2): 1627–1633. doi:10.1016/j.lpm.2007.03.032. PMID 17555914.
- ↑ Eaton WW, Shao H, Nestadt G, Lee HB, Lee BH, Bienvenu OJ, Zandi P (2008). "Population-based study of first onset and chronicity in major depressive disorder". Archives of General Psychiatry 65 (5): 513–20. doi:10.1001/archpsyc.65.5.513. PMC 2761826. PMID 18458203.
- ↑ Holma KM, Holma IA, Melartin TK, Rytsälä HJ, Isometsä ET (2008). "Long-term outcome of major depressive disorder in psychiatric patients is variable". Journal of Clinical Psychiatry 69 (2): 196–205. doi:10.4088/JCP.v69n0205. PMID 18251627.
- ↑ Kanai T, Takeuchi H, Furukawa TA, Yoshimura R, Imaizumi T, Kitamura T, Takahashi K (2003). "Time to recurrence after recovery from major depressive episodes and its predictors". Psychological Medicine 33 (5): 839–45. doi:10.1017/S0033291703007827. PMID 12877398.
- ↑ Geddes JR, Carney SM, Davies C, Furukawa TA, Kupfer DJ, Frank E, Goodwin GM (2003). "Relapse prevention with antidepressant drug treatment in depressive disorders: A systematic review". Lancet 361 (9358): 653–61. doi:10.1016/S0140-6736(03)12599-8. PMID 12606176.
- ↑ "Major Depression". MedlinePlus. 10 March 2014. Retrieved 16 July 2010.
- ↑ "Depression, Major: Prognosis". MDGuidlines. Guardian Life Insurance Company of America. Retrieved 16 July 2010.
- ↑ Cassano P, Fava M (2002). "Depression and public health: an overview". J Psychosom Res 53 (4): 849–57. doi:10.1016/S0022-3999(02)00304-5. PMID 12377293.
- ↑ Rush AJ (2007). "The varied clinical presentations of major depressive disorder". The Journal of clinical psychiatry 68 (Supplement 8): 4–10. PMID 17640152.
- ↑ 243.0 243.1 Alboni P, Favaron E, Paparella N, Sciammarella M, Pedaci M (2008). "Is there an association between depression and cardiovascular mortality or sudden death?". Journal of cardiovascular medicine (Hagerstown, Md.) 9 (4): 356–62. doi:10.2459/JCM.0b013e3282785240. PMID 18334889.
- ↑ Blair-West GW, Mellsop GW (2001). "Major depression: Does a gender-based down-rating of suicide risk challenge its diagnostic validity?". Australian and New Zealand Journal of Psychiatry 35 (3): 322–28. doi:10.1046/j.1440-1614.2001.00895.x. PMID 11437805.
- ↑ Oquendo MA, Bongiovi-Garcia ME, Galfalvy H, Goldberg PH, Grunebaum MF, Burke AK, Mann JJ (2007). "Sex differences in clinical predictors of suicidal acts after major depression: a prospective study". The American Journal of Psychiatry 164 (1): 134–41. doi:10.1176/ajp.2007.164.1.134. PMID 17202555.
- ↑ Bostwick JM, Pankratz VS (2000). "Affective disorders and suicide risk: A reexamination". American Journal of Psychiatry 157 (12): 1925–32. doi:10.1176/appi.ajp.157.12.1925. PMID 11097952.
- ↑ Weich S, Lewis G (1998). ( "Poverty, unemployment, and common mental disorders: Population based cohort study". BMJ 317 (7151): 115–19. doi:10.1136/bmj.317.7151.115. PMC 28602. PMID 9657786. Retrieved 16 September 2008.
- ↑ Mathers CD, Loncar D (2006). "Projections of global mortality and burden of disease from 2002 to 2030". PLoS Med. 3 (11): e442. doi:10.1371/journal.pmed.0030442. PMC 1664601. PMID 17132052.
- ↑ Andrews G (2008). "In Review: Reducing the Burden of Depression". Canadian Journal of Psychiatry 53 (7): 420–27. PMID 18674396.
- ↑ "WHO Disease and injury country estimates". World Health Organization. 2009. Retrieved 11 November 2009.
- ↑ "The world health report 2001 – Mental Health: New Understanding, New Hope". WHO website. World Health Organization. 2001. Retrieved 19 October 2008.
- ↑ Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M et al. (December 2012). "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet 380 (9859): 2163–96. doi:10.1016/S0140-6736(12)61729-2. PMID 23245607.
- ↑ 253.0 253.1 Andrade L, Caraveo-Anduaga JJ, Berglund P, Bijl RV, De Graaf R, Vollebergh W, Dragomirecka E, Kohn R, Keller M, Kessler RC, Kawakami N, Kiliç C, Offord D, Ustun TB, Wittchen HU (2003). "The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys". Int J Methods Psychiatr Res 12 (1): 3–21. doi:10.1002/mpr.138. PMID 12830306.
- ↑ Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE (2005). "Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication". Archives of General Psychiatry 62 (6): 593–602. doi:10.1001/archpsyc.62.6.593. PMID 15939837.
- ↑ Murphy JM, Laird NM, Monson RR, Sobol AM, Leighton AH (2000). "A 40-year perspective on the prevalence of depression: The Stirling County Study". Archives of General Psychiatry 57 (3): 209–15. doi:10.1001/archpsyc.57.3.209. PMID 10711905.
- ↑ 256.0 256.1 Kuehner C (2003). "Gender differences in unipolar depression: An update of epidemiological findings and possible explanations". Acta Psychiatrica Scandinavica 108 (3): 163–74. doi:10.1034/j.1600-0447.2003.00204.x. PMID 12890270.
- ↑ Eaton WW, Anthony JC, Gallo J, Cai G, Tien A, Romanoski A, Lyketsos C, Chen LS (1997). "Natural history of diagnostic interview schedule/DSM-IV major depression. The Baltimore Epidemiologic Catchment Area follow-up". Archives of General Psychiatry 54 (11): 993–99. doi:10.1001/archpsyc.1997.01830230023003. PMID 9366655.
- ↑ Rickards H (2005). "Depression in neurological disorders: Parkinson's disease, multiple sclerosis, and stroke". Journal of Neurology Neurosurgery and Psychiatry 76: i48–i52. doi:10.1136/jnnp.2004.060426. PMC 1765679. PMID 15718222.
- ↑ Strik JJ, Honig A, Maes M (2001). "Depression and myocardial infarction: relationship between heart and mind". Progress in neuro-psychopharmacology & biological psychiatry 25 (4): 879–92. doi:10.1016/S0278-5846(01)00150-6. PMID 11383983.
- ↑ Jorm AF (2000). "Does old age reduce the risk of anxiety and depression? A review of epidemiological studies across the adult life span". Psychological Medicine 30 (1): 11–22. doi:10.1017/S0033291799001452. PMID 10722172.
- ↑ Gelder, M., Mayou, R. and Geddes, J. 2005. Psychiatry. 3rd ed. New York: Oxford. pp105.
- ↑ Hippocrates, Aphorisms, Section 6.23
- ↑ depress. (n.d.). Online Etymology Dictionary. Retrieved 30 June 2008, from Dictionary.com
- ↑ Wolpert, L (1999). "Malignant Sadness: The Anatomy of Depression". The New York Times. Retrieved 30 October 2008.
- ↑ Berrios GE (1988). "Melancholia and depression during the 19th century: A conceptual history". British Journal of Psychiatry 153: 298–304. doi:10.1192/bjp.153.3.298. PMID 3074848.
- ↑ Davison, K (2006). "Historical aspects of mood disorders". Psychiatry 5 (4): 115–18. doi:10.1383/psyt.2006.5.4.115.
- ↑ Lewis, AJ (1934). "Melancholia: A historical review". Journal of Mental Science 80: 1–42. doi:10.1192/bjp.80.328.1.
- ↑ American Psychiatric Association (1968). "Schizophrenia". Diagnostic and statistical manual of mental disorders: DSM-II (PDF). Washington, DC: American Psychiatric Publishing, Inc. pp. 36–37, 40. Retrieved 3 August 2008.
- ↑ Schildkraut JJ (1965). "The catecholamine hypothesis of affective disorders: A review of supporting evidence". American Journal of Psychiatry 122 (5): 509–22. doi:10.1176/ajp.122.5.509. PMID 5319766.
- ↑ Angst J. Terminology, history and definition of bipolar spectrum. In: Maj M, Akiskal HS, López-Ibor JJ, Sartorius N (eds.), Bipolar disorders. Chichester: Wiley & Sons, LTD; 2002. pp. 53–55.
- ↑ Spitzer RL, Endicott J, Robins E (1975). "The development of diagnostic criteria in psychiatry" (PDF). Retrieved 8 November 2008.
- ↑ 272.0 272.1 Philipp M, Maier W, Delmo CD (1991). "The concept of major depression. I. Descriptive comparison of six competing operational definitions including ICD-10 and DSM-III-R". European Archives of Psychiatry and Clinical Neuroscience 240 (4–5): 258–65. doi:10.1007/BF02189537. PMID 1829000.
- ↑ Bolwig, Tom G.; Shorter, Edward (2007). "Melancholia: Beyond DSM, beyond neurotransmitters. Proceedings of a conference, May 2006, Copenhagen, Denmark". Acta Psychiatrica Scandinavica Suppl 115 (433): 4–183. doi:10.1111/j.1600-0447.2007.00956.x. PMID 17280564.
- ↑ Fink M, Bolwig TG, Parker G, Shorter E (2007). "Melancholia: Restoration in psychiatric classification recommended". Acta Psychiatrica Scandinavica 115 (2): 89–92. doi:10.1111/j.1600-0447.2006.00943.x. PMID 17244171.
- ↑ Healy, David (1999). The Antidepressant Era. Cambridge, MA: Harvard University Press. p. 42. ISBN 0-674-03958-0.
- ↑ Wolf, Joshua "Lincoln's Great Depression", The Atlantic, October 2005, Retrieved 10 October 2009
- ↑ Maloney F (3 November 2005). "The Depression Wars: Would Honest Abe Have Written the Gettysburg Address on Prozac?". Slate magazine. Washington Post. Retrieved 3 October 2008.
- ↑ Karasz A (2005). "Cultural differences in conceptual models of depression". Social Science in Medicine 60 (7): 1625–35. doi:10.1016/j.socscimed.2004.08.011. PMID 15652693.
- ↑ Tilbury, F (2004). "There are orphans in Africa still looking for my hands': African women refugees and the sources of emotional distress". Health Sociology Review 13 (1): 54–64. doi:10.5555/hesr.2004.13.1.54. Retrieved 3 October 2008.
- ↑ Parker G, Gladstone G, Chee KT (2001). "Depression in the planet's largest ethnic group: The Chinese". American Journal of Psychiatry 158 (6): 857–64. doi:10.1176/appi.ajp.158.6.857. PMID 11384889.
- ↑ Parker G (2007). "Is depression overdiagnosed? Yes". BMJ 335 (7615): 328. doi:10.1136/bmj.39268.475799.AD. PMC 1949440. PMID 17703040.
- ↑ Pilgrim D, Bentall R (1999). "The medicalisation of misery: A critical realist analysis of the concept of depression". Journal of Mental Health 8 (3): 261–74. doi:10.1080/09638239917580.
- ↑ Steibel W (Producer) (1998). "Is depression a disease?". Debatesdebates. Retrieved 16 November 2008.
- ↑ Blazer DG (2005). The age of melancholy: "Major depression" and its social origins. New York, NY, USA: Routledge. ISBN 978-0-415-95188-3.
- ↑ Hillman J (T Moore, Ed.) (1989). A blue fire: Selected writings by James Hillman. New York, NY, USA: Harper & Row. pp. 152–53. ISBN 0-06-016132-9.
- ↑ Seymour, Miranda (2002). Mary Shelley. Grove Press. pp. 560–61. ISBN 0-8021-3948-5.
- ↑ "Biography of Henry James". pbs.org. Retrieved 19 August 2008.
- ↑ Burlingame, Michael (1997). The Inner World of Abraham Lincoln. Urbana: University of Illinois Press. pp. xvii, 92–113. ISBN 0-252-06667-7.
- ↑ Pita E (26 September 2001). "An Intimate Conversation with...Leonard Cohen". Retrieved 3 October 2008.
- ↑ Jeste ND, Palmer BW, Jeste DV (2004). "Tennessee Williams". American Journal of Geriatric Psychiatry 12 (4): 370–75. doi:10.1097/00019442-200407000-00004. PMID 15249274.
- ↑ James H (Ed.) (1920). Letters of William James (Vols. 1 and 2). Montana USA: Kessinger Publishing Co. pp. 147–48. ISBN 978-0-7661-7566-2.
- ↑ Hergenhahn 2005, p. 311
- ↑ Cohen D (1979). J. B. Watson: The Founder of Behaviourism. London, UK: Routledge & Kegan Paul. p. 7. ISBN 0-7100-0054-5.
- ↑ Andreasen NC (2008). "The relationship between creativity and mood disorders". Dialogues in clinical neuroscience 10 (2): 251–5. PMC 3181877. PMID 18689294.
- ↑ Simonton, DK (2005). "Are genius and madness related? Contemporary answers to an ancient question". Psychiatric Times 22 (7).
- ↑ Heffernan CF (1996). The melancholy muse: Chaucer, Shakespeare and early medicine. Pittsburgh, PA, USA: Duquesne University Press. ISBN 0-8207-0262-5.
- ↑ Mill JS (2003). "A crisis in my mental history: One stage onward". Autobiography (TXT). Project Gutenberg EBook. pp. 1826–32. ISBN 1-4212-4200-1. Retrieved 9 August 2008.
- ↑ Sterba R (1947). "The 'Mental Crisis' of John Stuart Mill". Psychoanalytic Quarterly 16 (2): 271–72. Retrieved 5 November 2008.
- ↑ 299.0 299.1 "Churchill’s Black Dog?: The History of the ‘Black Dog’ as a Metaphor for Depression" (PDF). Black Dog Institute website. Black Dog Institute. 2005. Retrieved 18 August 2008.
- ↑ Jorm AF, Angermeyer M, Katschnig H (2000). "Public knowledge of and attitudes to mental disorders: a limiting factor in the optimal use of treatment services". In Andrews G, Henderson S (eds). Unmet Need in Psychiatry:Problems, Resources, Responses. Cambridge University Press. p. 409. ISBN 0-521-66229-X.
- ↑ Paykel ES, Tylee A, Wright A, Priest RG, Rix S, Hart D (1997). "The Defeat Depression Campaign: psychiatry in the public arena". American Journal of Psychiatry 154 (6 Suppl): 59–65. PMID 9167546.
- ↑ Paykel ES, Hart D, Priest RG (1998). "Changes in public attitudes to depression during the Defeat Depression Campaign". British Journal of Psychiatry 173 (6): 519–22. doi:10.1192/bjp.173.6.519. PMID 9926082.
Cited works
- American Psychiatric Association (2000a). Diagnostic and statistical manual of mental disorders, Fourth Edition, Text Revision: DSM-IV-TR. Washington, DC: American Psychiatric Publishing, Inc. ISBN 0-89042-025-4.
- Barlow DH; Durand VM (2005). Abnormal psychology: An integrative approach (5th ed.). Belmont, CA, USA: Thomson Wadsworth. ISBN 0-534-63356-0.
- Beck AT, Rush J, Shaw BF, Emery G (1987) [1979]. Cognitive Therapy of depression. New York, NY, USA: Guilford Press. ISBN 0-89862-919-5.
- Hergenhahn BR (2005). An Introduction to the History of Psychology (5th ed.). Belmont, CA, USA: Thomson Wadsworth. ISBN 0-534-55401-6.
- May R (1994). The discovery of being: Writings in existential psychology. New York, NY, USA: W. W. Norton & Company. ISBN 0-393-31240-2.
- Hadzi-Pavlovic, Dusan; Parker, Gordon (1996). Melancholia: a disorder of movement and mood: a phenomenological and neurobiological review. Cambridge, UK: Cambridge University Press. ISBN 0-521-47275-X.
- Royal Pharmaceutical Society of Great Britain (2008). British National Formulary (BNF 56). UK: BMJ Group and RPS Publishing. ISBN 978-0-85369-778-7.
- Sadock, Virginia A.; Sadock, Benjamin J.; Kaplan, Harold I. (2003). Kaplan & Sadock's synopsis of psychiatry: behavioral sciences/clinical psychiatry. Philadelphia: Lippincott Williams & Wilkins. ISBN 0-7817-3183-6.
External links
- Depression at DMOZ
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||