List of benzodiazepines
| Benzodiazepines |
|---|
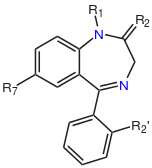 The core structure of benzodiazepines. "R" labels denote common locations of side chains, which give different benzodiazepines their unique properties. |
The below tables contain a sample list of benzodiazepines and benzodiazepine analogs that are commonly prescribed, with their basic pharmacological characteristics such as half-life and equivalent doses to other benzodiazepines also listed, along with their trade names and primary uses. The elimination half-life is how long it takes for half of the drug to be eliminated by the body. "Time to peak" refers to when maximum levels of the drug in the blood occur after a given dose. Benzodiazepines generally share the same pharmacological properties, such as anxiolytic, sedative, hypnotic, skeletal muscle relaxant, amnesic and anticonvulsant (hypertension in combination with other anti hypertension medications). Variation in potency of certain effects may exist among individual benzodiazepines. Some benzodiazepines produce active metabolites. Active metabolites are produced when a person's body metabolizes the drug into compounds that share a similar pharmacological profile to the parent compound and thus are relevant when calculating how long the pharmacological effects of a drug will last. Long-acting benzodiazepines with long-acting active metabolites such as diazepam and chlordiazepoxide are often prescribed for benzodiazepine or alcohol withdrawal or for anxiety if constant dose levels are required throughout the day. Shorter-acting benzodiazepines are often preferred for insomnia due to their lesser hangover effect.[1][2][3][4][5]
It is important to note that the elimination half-life of diazepam and chlordiazepoxide as well as other long half-life benzodiazepines is twice as long in the elderly compared to younger individuals. Individuals with an impaired liver also metabolise benzodiazepines more slowly. Many doctors make the mistake of not adjusting benzodiazepine dosage according to age in elderly patients. Thus the approximate equivalent doses below may need to be adjusted accordingly in individuals on short acting benzodiazepines who metabolise long-acting benzodiazepines more slowly and vice versa. The changes are most notable with long acting benzodiazepines as these are prone to significant accumulation in such individuals. For example the equivalent dose of diazepam in an elderly individual on lorazepam may be up to half of what would be expected in a younger individual.[6][7] Equivalencies between individual benzodiazepines can differ by 400 fold on a mg per mg basis; awareness of this fact is necessary for the safe and effective use of benzodiazepines.[8]
Dose equivalency table
Data in the table below is taken from the Ashton "Benzodiazepine Equivalency Table".[9] The equivalences should be considered rough guidelines, as individual patient responses may vary widely.
| Drug Name | Common Brand Names* | Time to Peak (Onset of action in hours) | Elimination Half-Life (h)† [active metabolite] | Therapeutic use | Approximate Equivalent Dose‡ |
|---|---|---|---|---|---|
| Alprazolam | Helex, Xanax, Xanor, Onax, Alprox, Restyl, Tafil | 1-2 | 9–20 hours | anxiolytic | 0.5 mg |
| Bentazepam | Thiadipona | 1-3 | 2-4 hours | anxiolytic | 25 mg |
| Bretazenil[10] | N/A | ? | 2.5 hours | anxiolytic, anticonvulsant | 0.5 mg |
| Bromazepam | Lectopam, Lexaurin, Lexotanil, Lexotan, Bromam | 1-3 | 10–20 hours | anxiolytic | 5–6 mg |
| Brotizolam | Lendormin, Dormex, Sintonal, Noctilan | 0.5-2 | 4–5 hours | hypnotic | 0.25 mg |
| Camazepam | Albego, Limpidon, Paxor | 0.5-2 | 6-29 hours | anxiolytic | 10 mg |
| Chlordiazepoxide | Librium, Risolid, Elenium | 1.5-4 | 5–30 hours [36–200 hours] | anxiolytic | 25 mg |
| Cinolazepam | Gerodorm | 0.5-2 | 9 hours | sedative | 40 mg |
| Clonazepam | Rivatril, Rivotril, Klonopin, Iktorivil, Paxam | 1-4 | 18–50 hours | anxiolytic, anticonvulsant | 0.5 mg |
| Clorazepate | Tranxene, Tranxilium | Variable | 36–100 hours | anxiolytic, anticonvulsant | 15 mg |
| Clotiazepam | Veratran, Clozan, Rize | 1-3 | 6–18 hours | anxiolytic | 5–10 mg |
| Cloxazolam | Sepazon, Olcadil | 2-5 (?) | 18–50 hours | anxiolytic, anticonvulsant | 1 mg |
| Delorazepam | Dadumir | 1-2 | 60–140 hours | anxiolytic | 1 mg |
| Deschloroetizolam | Thialprazolam | 1-2 | 10–40 hours | anxiolytic | about 2 mg |
| Diazepam | Antenex, Apaurin, Apzepam, Apozepam, Hexalid, Pax, Stesolid, Stedon, Valium, Vival, Valaxona | 1-1.5 | 20–100 hours [36–200] | anxiolytic, anticonvulsant, muscle relaxant | 10 mg |
| Diclazepam[11] | N/A | 1.5-4 (4-6) | 42–220 hours [10–200 (metabolites)] | anxiolytic, anticonvulsant, hypnotic muscle relaxant, sedative, skeletal muscle relaxant | 1-1.5 mg |
| Estazolam | ProSom | 1-5 | 10–24 hours | hypnotic | 2 mg |
| Ethyl carfluzepate | N/A | 1-5 | 11–24 hours | hypnotic | 2 mg |
| Etizolam | Etilaam, Etizest, Pasaden, Depas | 1-2 | 6 hours | anxiolytic, hypnotic | 1 mg |
| Ethyl loflazepate | Victan, Meilax, Ronlax | 1.5 | 50–100 hours | anxiolytic | 2 mg |
| Flubromazepam[12] | N/A | 1.5-4 (4-8) | 100–220 hours | anxiolytic, anticonvulsant, hypnotic muscle relaxant, sedative | 4-6 mg |
| Flunitrazepam | Rohypnol, Hipnosedon, Vulbegal, Fluscand, Flunipam, Ronal, Rohydorm, | 0.5-3 | 18–26 hours [36–200 hours] | hypnotic | 1 mg |
| Flurazepam | Dalmadorm, Dalmane | 1-1.5 | 40–250 hours | hypnotic | 15–30 mg |
| Flutoprazepam | Restas | 0.5-9 | 60–90 hours | hypnotic, anticonvulsant | 2–3 mg |
| Halazepam | Paxipam | 1-3 | 30–100 hours | anxiolytic | 20–40 mg |
| Ketazolam | Anxon | 2.5-3 | 30–100 hours [36–200] | anxiolytic | 15–30 mg |
| Loprazolam | Dormonoct | 0.5-4 | 6–12 hours | hypnotic | 2 mg |
| Lorazepam | Ativan, Lorenin, Lorsilan, Temesta, Tavor, Lorabenz | 2-4 | 10–20 hours | anxiolytic, anticonvulsant | 1 mg |
| Lormetazepam | Loramet, Noctamid, Pronoctan | 0.5-2 | 10–12 hours | hypnotic | 1.5 mg |
| Medazepam | Nobrium, Ansilan, Mezapam, Rudotel, Raporan | ? | 36–200 hours | anxiolytic | 10 mg |
| Midazolam | Dormicum, Versed, Hypnovel, Dormonid | 0.5-1 | 3 hours (1.8–6 hours) | hypnotic, anticonvulsant | 7.5 mg |
| Nimetazepam | Erimin | 0.5-3 | 14–30 hours | hypnotic | 5 mg |
| Nitrazepam | Mogadon, Alodorm, Pacisyn, Dumolid, Nitrazadon | 0.5-7 | 15–38 hours | hypnotic, anticonvulsant | 10 mg |
| Nordazepam | Madar, Stilny | ? | 50–120 hours | anxiolytic | 10 mg |
| Oxazepam | Seresta, Serax, Serenid, Serepax, Sobril, Oxabenz, Oxapax, Opamox | 3-4 | 4–15 hours | anxiolytic | 20 mg |
| Phenazepam | Phenazepam | 1.5-4 | 60 hours | anxiolytic, anticonvulsant | 1 mg |
| Pinazepam | Domar | ? | 40–100 hours | anxiolytic | 20 mg |
| Prazepam | Lysanxia, Centrax | 2-6 | 36–200 hours | anxiolytic | 20 mg |
| Premazepam | N/A | 2-6 | 10–13 hours | anxiolytic | 15 mg |
| Pyrazolam | Pyrazolam, Bromazolam | 1-1.5 | 16-18[13] hours | anxiolytic | 1 mg |
| Quazepam | Doral | 1-5 | 39–120 hours | hypnotic | 20 mg |
| Temazepam | Restoril, Normison, Euhypnos, Temaze, Tenox | 0.5-3 | 8–22 hours | hypnotic | 20 mg |
| Tetrazepam | Myolastan | 1-3 | 3–26 hours | Skeletal muscle relaxant | 100 mg |
| Triazolam | Halcion, Rilamir | 0.5-2 | 2 hours | hypnotic | 0.25 mg (0.5 mg with oral bioavailability) |
Atypical benzodiazepine receptor ligands
| Drug Name | Common Brand Names* | Elimination Half-Life (h)† [active metabolite] | Primary Effects | Approximate Equivalent Dose‡ |
| Clobazam | Frisium, Urbanol | 8–60 hours | anxiolytic, anticonvulsant | 20 mg |
| DMCM | ? | ? | anxiogenic, convulsant | Non-applicable |
| Flumazenil** | Anexate, Lanexat, Mazicon, Romazicon | 1 hour | antidote | Typical dose 0.2 - 0.6 mgð |
| Eszopiclone§ | Lunesta | 6 hours | hypnotic | 3 mg |
| Zaleplon§ | Sonata, Starnoc | 1 hours | hypnotic | 20 mg |
| Zolpidem§ | Ambien, Nytamel, Sanval, Stilnoct, Stilnox, Sublinox (Canada), Xolnox, Zoldem, Zolnod | 2.6 hours | hypnotic | 20 mg |
| Zopiclone§ | Imovane, Rhovane, Ximovan; Zileze; Zimoclone; Zimovane; Zopitan; Zorclone, | 4–6 hours | hypnotic | 15 mg |
* Not all trade names are listed. Click on drug name to see a more comprehensive list.
‡ Equivalent doses are based on clinical experience but may vary between individuals.[9]
** Flumazenil is an imidazobenzodiazepine derivative,[14] and in layman's terms, it is a benzodiazepine overdose antidote that is given intravenously in Intensive Care Units (ICUs) to reverse the effects of benzodiazepine overdoses, as well for overdoses of the non-benzodiazepine "Z-drugs" such as Ambien and Lunesta.[15] Flumazenil is contraindicated for benzodiazepine-tolerant patients in overdose cases.[16] In such cases, the benefits are far outweighed by the risks, which include potential and severe seizures.[17][14] The method by which Flumazenil acts to prevent non-benzodiazepine tolerant overdose from causing potential harm is via preventing the benzodiazepines and Z-drugs from binding to the GABAA receptors via competitive inhibition which the Flumazenil creates. Clinical observation notating the patient's oxygen levels, respiratory, heart and blood pressure rates are used, as they are much safer than the potential seizure effects from Flumazenil. Supportive care to mediate any problems resulting from abnormal rates of the pulmonary, respiratory, and cardiovascular systems is typically the only treatment that is required in benzodiazepine-only overdoses.[18] In most cases, activated charcoal/carbon is often used to prevent benzodiazepines from being absorbed by the gastrointestinal tract, and the use of stomach-pumping/gastric lavage is no longer commonly used nor suggested by some toxicologists.[19] Even in cases where other central nervous system (CSN) depressants (such as in combined benzodiazepine and tricyclic antidepressant/TCA overdoses) are detected and/or suspected, endotrachial intubation for the airway path and supportive oxygen are typically implemented and are much safer than Flumazenil.[18]
Controversy
The Ashton Manual claims the potency of both alprazolam and clonazepam to be 0.5 mg equivalent to 10 mg of diazepam, whereas most sources give an 1 mg equivalent to 10 mg of diazepam.[20]
Another chart with different ratios can be seen in the pdf document released by the Australian Department of Health. It notes that 10 mg of diazepam is equivalent to 1 mg of alprazolam and 0.5 - 1 mg of clonazepam.[21]
The UK's House of Commons began APPGITA/The All Party Parliamentary Group on Involuntary Tranquilliser Addiction. Since 2002, APPGITA has tried to politically mandate prescribing guidelines for benzodiazepines.[22] APPGITA has attempted to get a two to four week limit mandate for prescribing benzodiazepines to replace the two to four week benzodiazepine prescribing guidelines, which are merely recommended.[23][24]
See also
References
- ↑ Golombok S, Lader M (August 1984). "The psychopharmacological effects of premazepam, diazepam and placebo in healthy human subjects". Br J Clin Pharmacol 18 (2): 127–33. doi:10.1111/j.1365-2125.1984.tb02444.x. PMC 1463527. PMID 6148956.
- ↑ de Visser SJ, van der Post JP, de Waal PP, Cornet F, Cohen AF, van Gerven JM (January 2003). "Biomarkers for the effects of benzodiazepines in healthy volunteers" (PDF). Br J Clin Pharmacol 55 (1): 39–50. doi:10.1046/j.1365-2125.2002.t01-10-01714.x. PMC 1884188. PMID 12534639.
- ↑ "Benzodiazepine Names". non-benzodiazepines.org.uk. Retrieved 2009-04-05.
- ↑ C. Heather Ashton (March 2007). "Benzodiazepine Equivalence Table". benzo.org.uk. Retrieved 2009-04-05.
- ↑ Bob, Dr (July 1995). "Benzodiazepine Equivalence Charts". dr-bob.org. Retrieved 2009-04-05.
- ↑ Salzman, Carl (15 May 2004). Clinical geriatric psychopharmacology (4th ed.). USA: Lippincott Williams & Wilkins. pp. 450–453. ISBN 978-0-7817-4380-8.
- ↑ Delcò F, Tchambaz L, Schlienger R, Drewe J, Krähenbühl S (2005). "Dose adjustment in patients with liver disease". Drug Saf 28 (6): 529–45. doi:10.2165/00002018-200528060-00005. PMID 15924505.
- ↑ Riss, J.; Cloyd, J.; Gates, J.; Collins, S. (Aug 2008). "Benzodiazepines in epilepsy: pharmacology and pharmacokinetics.". Acta Neurol Scand 118 (2): 69–86. doi:10.1111/j.1600-0404.2008.01004.x. PMID 18384456.
- ↑ 9.0 9.1 Ashton, Dr. Heather (April 2007). "Benzodiazepine Equivalency Table". Retrieved 22 March 2015.
- ↑ van Steveninck AL et al. (1996). "Pharmacokinetic and pharmacodynamic interactions of bretazenil and diazepam with alcohol.". British Journal of Clinical Pharmacology 41 (6): 565–573. doi:10.1046/j.1365-2125.1996.38514.x. PMC 2042631. PMID 8799523.
- ↑ Moosmann, Bisel P, Auwärter V. (2014). "Characterization of the designer benzodiazepine diclazepam and preliminary data on its metabolism and pharmacokinetics.". The National Center for Biotechnology 1 (7-8): 1. doi:10.1002/dta.1628. PMID 24604775.
- ↑ J Mass Spectrom (2013). "Detection and identification of the designer benzodiazepine flubromazepam and preliminary data on its metabolism and pharmacokinetics.". The National Center for Biotechnology 1 (11): 1150–9. doi:10.1002/jms.3279. PMID 24259203.
- ↑
- ↑ 14.0 14.1 http://www.gene.com/download/pdf/romazicon_prescribing.pdf
- ↑ "Flumazenil Injection, Solution [App Pharmaceuticals, Llc]". Dailymed.nlm.nih.gov. Retrieved 2014-08-15.
- ↑ "DailyMed". Dailymed.nlm.nih.gov. Retrieved 2014-08-15.
- ↑ Gary R. Fleisher; Stephen Ludwig; Benjamin K. Silverman (2002). Synopsis of pediatric emergency medicine. Lippincott Williams & Wilkins. pp 409. ISBN 978-0-7817-3274-1. Retrieved 3/22/2013.
- ↑ 18.0 18.1 http://www.inchem.org/documents/pims/pharm/pim181.htm#DivisionTitle:8.1.1.1 Toxicological analyses. Retrieved 3/21/2013.)
- ↑ Vale JA, Kulig K; American Academy of Clinical Toxicology; European Association of Poisons Centres and Clinical Toxicologists. (2004). "Position paper: gastric lavage". J Toxicol Clin Toxicol 42 (7): 933–943. doi:10.1081/CLT-200045006. PMID 15641639
- ↑ http://www.csam-asam.org/sites/default/files/pdf/misc/TIP_45.pdf, Page 76. US Department of Health and Human Services, 2006. Retrieved 21 March 2015
- ↑ http://www.health.qld.gov.au/atod/documents/24904.pdf, Table 11, Section 5.8, Australian Department of Health.
- ↑ "Early Day Motion, Launched 18 November 2002". Appgita. 18 November 2002. Retrieved 15 August 2014.
- ↑ "November | 2002". Appgita. Retrieved 15 August 2014.
- ↑ "APPG for Involuntary Tranquilliser Addiction". benzo.org.uk. Retrieved 21 March 2015.
Further reading
- Gitlow, Stuart (1 October 2006). Substance Use Disorders: A Practical Guide (2nd ed.). USA: Lippincott Williams and Wilkins. p. 110. ISBN 978-0-7817-6998-3.
- Galanter, Marc; Kleber, Herbert D. (1 July 2008). The American Psychiatric Publishing Textbook of Substance Abuse Treatment (4th ed.). United States of America: American Psychiatric Publishing Inc. p. 216. ISBN 978-1-58562-276-4.