Kikuchi disease
| Kikuchi-Fujimoto disease | |
|---|---|
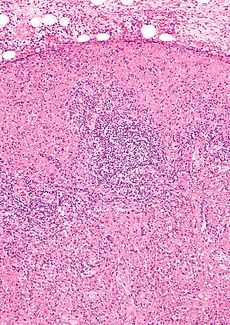 Micrograph of a lymph node with Kikuchi disease showing the characteristic features (abundant histiocytes, necrosis without neutrophils). H&E stain. | |
| Classification and external resources | |
| eMedicine | med/3663 |
| MeSH | D020042 |
Kikuchi-Fujimoto disease (KFD) was described in 1972 in Japan. It is also known as Kikuchi disease, histiocytic necrotizing lymphadenitis, Kikuchi necrotizing lymphadenitis, phagocytic necrotizing lymphadenitis, subacute necrotizing lymphadenitis, and necrotizing lymphadenitis.[1][2][3][4]
It was first described in Japan by Dr Masahiro Kikuchi in 1972[5] and independently by Y. Fujimoto.
Epidemiology
Kikuchi-Fujimoto disease (KFD) is a rare, self-limiting disorder that typically affects the cervical lymph nodes. Recognition of this condition is crucial, especially because it can easily be mistaken for tuberculosis, lymphoma, or even adenocarcinoma. Awareness of this disorder will help prevent misdiagnosis and inappropriate treatment.[1]
Kikuchi's disease is a very rare disease and mainly seen in Japan. Isolated cases are reported in America, Europe and Asia. It is mainly a disease of young adults (mean age, 20–30 years), with a slight bias towards females. The cause of this disease is not known although infectious and autoimmune etiologies have been proposed. Course of the disease is generally benign and self-limiting. Lymphadenopathy most often resolves over several weeks to six months. Recurrence rate is about 3%. Mortality is extremely rare and usually due to hepatic, respiratory, or cardiac failure.
Pathophysiology
Some studies have suggested a genetic predisposition to the proposed autoimmune response. Several infectious candidates have been associated with Kikuchi's disease.[6]
There are many postulates about the etiology of KFD. A microbial/viral or autoimmune cause has been suggested. Mycobacterium szulgai, Yersinia and Toxoplasma have been implicated. More recently there has been growing evidence of the role of Epstein-Barr virus, as well as other viruses (HHV6, HHV8, Parvovirus B19, HIV- and HTLV-1) in the pathogenesis of KFD.[1] However, many independent studies have failed to identify the presence of these infectious agents in cases of Kikuchi lymphadenopathy.[7] In addition, serologic tests including antibodies to a host of viruses have consistently proven noncontributory and no viral particles have been identified ultrastructurally. It is now proposed that KFD is a nonspecific hyperimmune reaction to a variety of infectious, chemical, physical and neoplastic agents. In addition to SLE, other autoimmune conditions and manifestations such as antiphospholipid syndrome, polymyositis, systemic juvenile idiopathic arthritis, bilateral uveitis, arthritis and cutaneous necrotizing vasculitis have been linked to KFD. It is possible that KFD may represent an exuberant T-cell mediated immune response in a genetically susceptible individual to a variety of non-specific stimuli.[1]
Clinical Features
The signs and symptoms of Kikuchi's disease are fever, lymphadenopathy, skin rashes and headache. Rarely hepatosplenomegaly and nervous system involvement resembling meningitis is seen. Differential diagnosis includes SLE, disseminated tuberculosis, lymphoma, Sarcoidosis, and viral lymphadenitis.Clinical findings sometimes may include positive results for IgM/IgG/IgA Antibodies.
For other causes of lymph node enlargement, see lymphadenopathy.
Diagnosis
It is diagnosed by lymph node excision biopsy.
Kikuchi's disease is a self-limiting illness which has symptoms which may overlap with Hodgkin's lymphoma leading to misdiagnosis in some patients.
ANA, APLA, Anti-dsDNA, RF are usually negative, and may help in differentiating from SLE.
Management
No specific cure. Treatment largely supportive. NSAIDs for tender lymphnodes and fever, corticosteroids are useful in severe extranodal or generalized disease.
Symptomatic measures aimed at relieving the distressing local and systemic complaints have been described as the main line of management of KFD. Analgesics, antipyretics, nonsteroidal anti-inflammatory drugs(NSAIDs) and corticosteroids have been used. If the clinical course is more severe, with multiple flares of bulky cervical lymphadenopathy and fever, then a low-dose corticosteroid treatment has been suggested.
See also
- Jessner lymphocytic infiltrate of the skin
- List of cutaneous conditions
References
- ↑ 1.0 1.1 1.2 1.3 Rammohan A, Cherukuri SD, Manimaran AB, Manohar RR, Naidu RM (June 2012). "Kikuchi-Fujimoto Disease: A Sheep in Wolf's Clothing". J Otolaryngol Head Neck Surg 41 (3): 222–226. PMID 22762705.
- ↑ Kaushik V, Malik TH, Bishop PW, Jones PH (June 2004). "Histiocytic necrotising lymphadenitis (Kikuchi's disease): a rare cause of cervical lymphadenopathy". Surgeon 2 (3): 179–82. doi:10.1016/s1479-666x(04)80084-2. PMID 15570824.
- ↑ Bosch X, Guilabert A (2006). "Kikuchi-Fujimoto disease". Orphanet J Rare Dis 1: 18. doi:10.1186/1750-1172-1-18. PMC 1481509. PMID 16722618.
- ↑ Bosch X, Guilabert A, Miquel R, Campo E (July 2004). "Enigmatic Kikuchi-Fujimoto disease: a comprehensive review". Am. J. Clin. Pathol. 122 (1): 141–52. doi:10.1309/YF08-1L4T-KYWV-YVPQ. PMID 15272543.
- ↑ Kikuchi M. Lymphadenitis showing focal reticulum cell hyperplasia with nuclear debris and phagocytes. Acta Hematol Jpn 1972;35:379–80.
- ↑ Atwater AR, Longley BJ, Aughenbaugh WD (July 2008). "Kikuchi's disease: case report and systematic review of cutaneous and histopathologic presentations". J. Am. Acad. Dermatol. 59 (1): 130–6. doi:10.1016/j.jaad.2008.03.012. PMID 18462833.
- ↑ Rosado, F. G.; Tang, Y. W.; Hasserjian, R. P.; McClain, C. M.; Wang, B; Mosse, C. A. (2013). "Kikuchi-Fujimoto lymphadenitis: Role of parvovirus B-19, Epstein-Barr virus, human herpesvirus 6, and human herpesvirus 8". Human Pathology 44 (2): 255–9. doi:10.1016/j.humpath.2012.05.016. PMID 22939574.
| ||||||||||||||||||||||||||||||||||||