Hypothalamus
| Hypothalamus | |
|---|---|
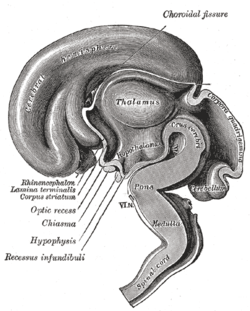
 Location of the human hypothalamus | |
 Location of the hypothalamus, in relation to the pituitary and to the rest of the brain | |
| Details | |
| Latin | hypothalamus |
| Identifiers | |
| Gray's | p.812 |
| MeSH | A08.186.211.730.385.357 |
| NeuroNames | hier-358 |
| NeuroLex ID | Hypothalamus |
| TA |
A14.1.08.401 A14.1.08.901 |
| FMA | 62008 |
| Anatomical terms of neuroanatomy | |
The hypothalamus (from Greek ὑπό, "under" and θάλαμος, "room, chamber") is a portion of the brain that contains a number of small nuclei with a variety of functions. One of the most important functions of the hypothalamus is to link the nervous system to the endocrine system via the pituitary gland (hypophysis).
The hypothalamus is located below the thalamus, just above the brainstem and is part of the limbic system.[1] In the terminology of neuroanatomy, it forms the ventral part of the diencephalon. All vertebrate brains contain a hypothalamus. In humans, it is roughly the size of an almond.
The hypothalamus is responsible for certain metabolic processes and other activities of the autonomic nervous system. It synthesizes and secretes certain neurohormones, often called releasing hormones or hypothalamic hormones, and these in turn stimulate or inhibit the secretion of pituitary hormones. The hypothalamus controls body temperature, hunger, important aspects of parenting and attachment behaviors, thirst,[2] fatigue, sleep, and circadian rhythms.
Structure

The hypothalamus is a brain structure made up of distinct nuclei as well as less anatomically distinct areas. It is found in all vertebrate nervous systems. In mammals, the axons of magnocellular neurosecretory cells in the paraventricular nucleus and the supraoptic nucleus (both located in the hypothalamus) contain oxytocin and vasopressin (antidiuretic hormone), and project into the posterior pituitary. Much smaller parvocellular neurosecretory cells, neurons of the paraventricular nucleus, release corticotropin-releasing hormone and other hormones into the hypophyseal portal system, where these hormones diffuse to the anterior pituitary.
Nuclei
The hypothalamic nuclei include the following:[3][4][5]
| Region | Area | Nucleus | Function[6] |
| Anterior | Preoptic | Preoptic nucleus | |
| Medial | Medial preoptic nucleus |
| |
| Supraoptic nucleus |
| ||
| Paraventricular nucleus |
| ||
| Anterior hypothalamic nucleus |
| ||
| Suprachiasmatic nucleus |
| ||
| Lateral | |||
| Lateral nucleus | |||
| Tuberal | Medial | Dorsomedial hypothalamic nucleus |
|
| Ventromedial nucleus |
| ||
| Arcuate nucleus |
| ||
| Lateral | Lateral nucleus | ||
| Lateral tuberal nuclei | |||
| Posterior | Medial | Mammillary nuclei (part of mammillary bodies) | |
| Posterior nucleus |
| ||
| Lateral | Lateral nucleus | ||
| Tuberomammillary nucleus[7] |
|
See also: ventrolateral preoptic nucleus, periventricular nucleus.
-

A cross section of the monkey hypothalamus displays 2 of the major hypothalamic nuclei on either side of the fluid-filled 3rd ventricle.
-
Hypothalamic nuclei
-
Hypothalamic nuclei on one side of the hypothalamus, shown in a 3-D computer reconstruction[1]
- ^ Brain Research Bulletin 35:323-327, 1994
Neural connections
The hypothalamus is highly interconnected with other parts of the central nervous system, in particular the brainstem and its reticular formation. As part of the limbic system, it has connections to other limbic structures including the amygdala and septum, and is also connected with areas of the autonomous nervous system.
The hypothalamus receives many inputs from the brainstem, the most notable from the nucleus of the solitary tract, the locus coeruleus, and the ventrolateral medulla.
Most nerve fibres within the hypothalamus run in two ways (bidirectional).
- Projections to areas caudal to the hypothalamus go through the medial forebrain bundle, the mammillotegmental tract and the dorsal longitudinal fasciculus.
- Projections to areas rostral to the hypothalamus are carried by the mammillothalamic tract, the fornix and terminal stria.
- Projections to areas of the sympathetic motor system (lateral horn spinal segments T1-L2/L3) are carried by the hypothalamospinal tract and they activate the sympathetic motor pathway
Sexual dimorphism
Several hypothalamic nuclei are sexually dimorphic; i.e., there are clear differences in both structure and function between males and females.
Some differences are apparent even in gross neuroanatomy: most notable is the sexually dimorphic nucleus within the preoptic area. However most of the differences are subtle changes in the connectivity and chemical sensitivity of particular sets of neurons.
The importance of these changes can be recognised by functional differences between males and females. For instance, males of most species prefer the odor and appearance of females over males, which is instrumental in stimulating male sexual behavior. If the sexually dimorphic nucleus is lesioned, this preference for females by males diminishes. Also, the pattern of secretion of growth hormone is sexually dimorphic, and this is one reason why in many species, adult males are much larger than females.
- Responsiveness to ovarian steroids
Other striking functional dimorphisms are in the behavioral responses to ovarian steroids of the adult. Males and females respond to ovarian steroids in different ways, partly because the expression of estrogen-sensitive neurons in the hypothalamus is sexually dimorphic; i.e., estrogen receptors are expressed in different sets of neurons.
Estrogen and progesterone can influence gene expression in particular neurons or induce changes in cell membrane potential and kinase activation, leading to diverse non-genomic cellular functions. Estrogen and progesterone bind to their cognate nuclear hormone receptors, which translocate to the cell nucleus and interact with regions of DNA known as hormone response elements (HREs) or get tethered to another transcription factor's binding site. Estrogen receptor (ER) has been shown to transactivate other transcription factors in this manner, despite the absence of an estrogen response element (ERE) in the proximal promoter region of the gene. In general, ERs and progesterone receptors (PRs) are gene activators, with increased mRNA and subsequent protein synthesis following hormone exposure.
Male and female brains differ in the distribution of estrogen receptors, and this difference is an irreversible consequence of neonatal steroid exposure. Estrogen receptors (and progesterone receptors) are found mainly in neurons in the anterior and mediobasal hypothalamus, notably:
- the preoptic area (where LHRH neurons are located)
- the periventricular nucleus (where somatostatin neurons are located)
- the ventromedial hypothalamus (which is important for sexual behavior).
Development
In neonatal life, gonadal steroids influence the development of the neuroendocrine hypothalamus. For instance, they determine the ability of females to exhibit a normal reproductive cycle, and of males and females to display appropriate reproductive behaviors in adult life.
- If a female rat is injected once with testosterone in the first few days of postnatal life (during the "critical period" of sex-steroid influence), the hypothalamus is irreversibly masculinized; the adult rat will be incapable of generating an LH surge in response to estrogen (a characteristic of females), but will be capable of exhibiting male sexual behaviors (mounting a sexually receptive female).
- By contrast, a male rat castrated just after birth will be feminized, and the adult will show female sexual behavior in response to estrogen (sexual receptivity, lordosis behavior).
In primates, the developmental influence of androgens is less clear, and the consequences are less understood. Within the brain, testosterone is aromatized to (estradiol), which is the principal active hormone for developmental influences. The human testis secretes high levels of testosterone from about week 8 of fetal life until 5–6 months after birth (a similar perinatal surge in testosterone is observed in many species), a process that appears to underlie the male phenotype. Estrogen from the maternal circulation is relatively ineffective, partly because of the high circulating levels of steroid-binding proteins in pregnancy.
Sex steroids are not the only important influences upon hypothalamic development; in particular, pre-pubertal stress in early life (of rats) determines the capacity of the adult hypothalamus to respond to an acute stressor.[8] Unlike gonadal steroid receptors, glucocorticoid receptors are very widespread throughout the brain; in the paraventricular nucleus, they mediate negative feedback control of CRF synthesis and secretion, but elsewhere their role is not well understood.
Function
Hormone release

The hypothalamus has a central neuroendocrine function, most notably by its control of the anterior pituitary, which in turn regulates various endocrine glands and organs. Releasing hormones (also called releasing factors) are produced in hypothalamic nuclei then transported along axons to either the median eminence or the posterior pituitary, where they are stored and released as needed.[9]
- Anterior pituitary
In the hypothalamic–adenohypophyseal axis, releasing hormones, also known as hypophysiotropic or hypothalamic hormones, are released from the median eminence, a prolongation of the hypothalamus, into the hypophyseal portal system, which carries them to the anterior pituitary where they exert their regulatory functions on the secretion of adenohypopyseal hormones.[10]
| Secreted hormone | Abbreviation | Produced by | Effect |
|---|---|---|---|
| Thyrotropin-releasing hormone (Prolactin-releasing hormone) |
TRH, TRF, or PRH | Parvocellular neurosecretory cells of the paraventricular nucleus | Stimulate thyroid-stimulating hormone (TSH) release from anterior pituitary (primarily) Stimulate prolactin release from anterior pituitary |
| Corticotropin-releasing hormone | CRH or CRF | Parvocellular neurosecretory cells of the paraventricular nucleus | Stimulate adrenocorticotropic hormone (ACTH) release from anterior pituitary |
| Dopamine (Prolactin-inhibiting hormone) |
DA or PIH | Dopamine neurons of the arcuate nucleus | Inhibit prolactin release from anterior pituitary |
| Growth-hormone-releasing hormone | GHRH | Neuroendocrine neurons of the Arcuate nucleus | Stimulate growth-hormone (GH) release from anterior pituitary |
| Gonadotropin-releasing hormone | GnRH or LHRH | Neuroendocrine cells of the Preoptic area | Stimulate follicle-stimulating hormone (FSH) release from anterior pituitary Stimulate luteinizing hormone (LH) release from anterior pituitary |
| Somatostatin[11] (growth-hormone-inhibiting hormone) |
SS, GHIH, or SRIF | Neuroendocrine cells of the Periventricular nucleus | Inhibit growth-hormone (GH) release from anterior pituitary Inhibit (moderately) thyroid-stimulating hormone (TSH) release from anterior pituitary |
Other hormones secreted from the median eminence include vasopressin, oxytocin, neurotensin, and orexin.[12][13][14][15]
- Posterior pituitary
In the hypothalamic-neurohypophyseal axis, neurohypophysial hormones are released from the posterior pituitary, which is actually a prolongation of the hypothalamus, into the circulation.
| Secreted hormone | Abbreviation | Produced by | Effect |
|---|---|---|---|
| Oxytocin | OXY or OXT | Magnocellular neurosecretory cells of the paraventricular nucleus and supraoptic nucleus | Uterine contraction Lactation (letdown reflex) |
| Vasopressin (antidiuretic hormone) |
ADH or AVP | Magnocellular and parvocellular neurosecretory cells of the paraventricular nucleus, magnocellular cells in supraoptic nucleus | Increase in the permeability to water of the cells of distal tubule and collecting duct in the kidney and thus allows water reabsorption and excretion of concentrated urine |
It is also known that hypothalamic-pituitary-adrenal axis (HPA) hormones are related to certain skin diseases and skin homeostasis. There is evidence linking hyperactivity of HPA hormones to stress-related skin diseases and skin tumors.[16]
Stimulation
The hypothalamus coordinates many hormonal and behavioural circadian rhythms, complex patterns of neuroendocrine outputs, complex homeostatic mechanisms, and important behaviours. The hypothalamus must, therefore, respond to many different signals, some of which generated externally and some internally. Delta wave signalling arising either in the thalamus or in the cortex influences the secretion of releasing hormones; GHRH and prolactin are stimulated whilst TRH is inhibited.
The hypothalamus is responsive to:
- Light: daylength and photoperiod for regulating circadian and seasonal rhythms
- Olfactory stimuli, including pheromones
- Steroids, including gonadal steroids and corticosteroids
- Neurally transmitted information arising in particular from the heart, the stomach, and the reproductive tract
- Autonomic inputs
- Blood-borne stimuli, including leptin, ghrelin, angiotensin, insulin, pituitary hormones, cytokines, plasma concentrations of glucose and osmolarity etc.
- Stress
- Invading microorganisms by increasing body temperature, resetting the body's thermostat upward.
Olfactory stimuli
Olfactory stimuli are important for sexual reproduction and neuroendocrine function in many species. For instance if a pregnant mouse is exposed to the urine of a 'strange' male during a critical period after coitus then the pregnancy fails (the Bruce effect). Thus, during coitus, a female mouse forms a precise 'olfactory memory' of her partner that persists for several days. Pheromonal cues aid synchronisation of oestrus in many species; in women, synchronised menstruation may also arise from pheromonal cues, although the role of pheromones in humans is disputed.
Blood-borne stimuli
Peptide hormones have important influences upon the hypothalamus, and to do so they must pass through the blood–brain barrier. The hypothalamus is bounded in part by specialized brain regions that lack an effective blood–brain barrier; the capillary endothelium at these sites is fenestrated to allow free passage of even large proteins and other molecules. Some of these sites are the sites of neurosecretion - the neurohypophysis and the median eminence. However, others are sites at which the brain samples the composition of the blood. Two of these sites, the SFO (subfornical organ) and the OVLT (organum vasculosum of the lamina terminalis) are so-called circumventricular organs, where neurons are in intimate contact with both blood and CSF. These structures are densely vascularized, and contain osmoreceptive and sodium-receptive neurons that control drinking, vasopressin release, sodium excretion, and sodium appetite. They also contain neurons with receptors for angiotensin, atrial natriuretic factor, endothelin and relaxin, each of which important in the regulation of fluid and electrolyte balance. Neurons in the OVLT and SFO project to the supraoptic nucleus and paraventricular nucleus, and also to preoptic hypothalamic areas. The circumventricular organs may also be the site of action of interleukins to elicit both fever and ACTH secretion, via effects on paraventricular neurons.
It is not clear how all peptides that influence hypothalamic activity gain the necessary access. In the case of prolactin and leptin, there is evidence of active uptake at the choroid plexus from the blood into the cerebrospinal fluid (CSF). Some pituitary hormones have a negative feedback influence upon hypothalamic secretion; for example, growth hormone feeds back on the hypothalamus, but how it enters the brain is not clear. There is also evidence for central actions of prolactin.
Findings have suggested that thyroid hormone (T4) is taken up by the hypothalamic glial cells in the infundibular nucleus/ median eminence, and that it is here converted into T3 by the type 2 deiodinase (D2). Subsequent to this, T3 is transported into the thyrotropin-releasing hormone (TRH)-producing neurons in the paraventricular nucleus. Thyroid hormone receptors have been found in these neurons, indicating that they are indeed sensitive to T3 stimuli. In addition, these neurons expressed MCT8, a thyroid hormone transporter, supporting the theory that T3 is transported into them. T3 could then bind to the thyroid hormone receptor in these neurons and affect the production of thyrotropin-releasing hormone, thereby regulating thyroid hormone production.[17]
The hypothalamus functions as a type of thermostat for the body.[18] It sets a desired body temperature, and stimulates either heat production and retention to raise the blood temperature to a higher setting or sweating and vasodilation to cool the blood to a lower temperature. All fevers result from a raised setting in the hypothalamus; elevated body temperatures due to any other cause are classified as hyperthermia.[18] Rarely, direct damage to the hypothalamus, such as from a stroke, will cause a fever; this is sometimes called a hypothalamic fever. However, it is more common for such damage to cause abnormally low body temperatures.[18]
Steroids
The hypothalamus contains neurons that react strongly to steroids and glucocorticoids – (the steroid hormones of the adrenal gland, released in response to ACTH). It also contains specialized glucose-sensitive neurons (in the arcuate nucleus and ventromedial hypothalamus), which are important for appetite. The preoptic area contains thermosensitive neurons; these are important for TRH secretion.
Neural
Oxytocin secretion in response to suckling or vagino-cervical stimulation is mediated by some of these pathways; vasopressin secretion in response to cardiovascular stimuli arising from chemoreceptors in the carotid body and aortic arch, and from low-pressure atrial volume receptors, is mediated by others. In the rat, stimulation of the vagina also causes prolactin secretion, and this results in pseudo-pregnancy following an infertile mating. In the rabbit, coitus elicits reflex ovulation. In the sheep, cervical stimulation in the presence of high levels of estrogen can induce maternal behavior in a virgin ewe. These effects are all mediated by the hypothalamus, and the information is carried mainly by spinal pathways that relay in the brainstem. Stimulation of the nipples stimulates release of oxytocin and prolactin and suppresses the release of LH and FSH.
Cardiovascular stimuli are carried by the vagus nerve. The vagus also conveys a variety of visceral information, including for instance signals arising from gastric distension or emptying, to suppress or promote feeding, by signalling the release of leptin or gastrin, respectively. Again this information reaches the hypothalamus via relays in the brainstem.
In addition hypothalamic function is responsive to—and regulated by—levels of all three classical monoamine neurotransmitters, noradrenaline, dopamine, and serotonin (5-hydroxytryptamine), in those tracts from which it receives innervation. For example noradrenergic inputs arising from the locus coeruleus have important regulatory effects upon corticotropin-releasing hormone (CRH) levels.
Control of food intake
The extreme lateral part of the ventromedial nucleus of the hypothalamus is responsible for the control of food intake. Stimulation of this area causes increased food intake. Bilateral lesion of this area causes complete cessation of food intake. Medial parts of the nucleus have a controlling effect on the lateral part. Bilateral lesion of the medial part of the ventromedial nucleus causes hyperphagia and obesity of the animal. Further lesion of the lateral part of the ventromedial nucleus in the same animal produces complete cessation of food intake.
There are different hypotheses related to this regulation:[19]
- Lipostatic hypothesis: This hypothesis holds that adipose tissue produces a humoral signal that is proportionate to the amount of fat and acts on the hypothalamus to decrease food intake and increase energy output. It has been evident that a hormone leptin acts on the hypothalamus to decrease food intake and increase energy output.
- Gutpeptide hypothesis: gastrointestinal hormones like Grp, glucagons, CCK and others claimed to inhibit food intake. The food entering the gastrointestinal tract triggers the release of these hormones, which act on the brain to produce satiety. The brain contains both CCK-A and CCK-B receptors.
- Glucostatic hypothesis: The activity of the satiety center in the ventromedial nuclei is probably governed by the glucose utilization in the neurons. It has been postulated that when their glucose utilization is low and consequently when the arteriovenous blood glucose difference across them is low, the activity across the neurons decrease. Under these conditions, the activity of the feeding center is unchecked and the individual feels hungry. Food intake is rapidly increased by intraventricular administration of 2-deoxyglucose therefore decreasing glucose utilization in cells.
- Thermostatic hypothesis: According to this hypothesis, a decrease in body temperature below a given set-point stimulates appetite, whereas an increase above the set-point inhibits appetite.
Fear processing
The medial zone of hypothalamus is part of a circuitry that controls motivated behaviors, like defensive behaviors.[20] Analyses of Fos-labeling showed that a series of nuclei in the "behavioral control column" is important in regulating the expression of innate and conditioned defensive behaviors.[21]
- Antipredatory defensive behavior
Exposure to a predator (such as a cat) elicits defensive behaviors in laboratory rodents, even when the animal has never been exposed to a cat.[22] In the hypothalamus, this exposure causes an increase in Fos-labeled cells in the anterior hypothalamic nucleus, the dorsomedial part of the ventromedial nucleus, and in the ventrolateral part of the premammillary nucleus (PMDvl).[23] The premammillary nucleus has an important role in expression of defensive behaviors towards a predator, since lesions in this nucleus abolish defensive behaviors, like freezing and flight.[23][24] The PMD does not modulate defensive behavior in other situations, as lesions of this nucleus had minimal effects on post-shock freezing scores.[24] The PMD has important connections to the dorsal periaqueductal gray, an important structure in fear expression.[25][26] In addition, animals display risk assessment behaviors to the environment previously associated with the cat. Fos-labeled cell analysis showed that the PMDvl is the most activated structure in the hypothalamus, and inactivation with muscimol prior to exposure to the context abolishes the defensive behavior.[23] Therefore, the hypothalamus, mainly the PMDvl, has an important role in expression of innate and conditioned defensive behaviors to a predator.
- Social defeat
Likewise, the hypothalamus has a role in social defeat: Nuclei in medial zone are also mobilized during an encounter with an aggressive conspecific. The defeated animal has an increase in Fos levels in sexually dimorphic structures, such as the medial pre-optic nucleus, the ventrolateral part of ventromedial nucleus, and the ventral premammilary nucleus.[27] Such structures are important in other social behaviors, such as sexual and aggressive behaviors. Moreover, the premammillary nucleus also is mobilized, the dorsomedial part but not the ventrolateral part.[27] Lesions in this nucleus abolish passive defensive behavior, like freezing and the "on-the-back" posture.[27]
Sexual orientation
According to D. F. Swaab, writing in a July 2008 paper, "Neurobiological research related to sexual orientation in humans is only just gathering momentum, but the evidence already shows that humans have a vast array of brain differences, not only in relation to gender, but also in relation to sexual orientation."[28]
Swaab first reported on the relationship between sexual orientation in males and the hypothalamus's "clock", the suprachiasmatic nucleus (SCN). In 1990, Swaab and Hofman[29] reported that the suprachiasmatic nucleus in homosexual men was significantly larger than in heterosexual men. Then in 1995, Swaab et al.[30] linked brain development to sexual orientation by treating male rats both pre- and postnatally with ATD, an aromatase blocker in the brain. This produced an enlarged SCN and bisexual behavior in the adult male rats. In 1991, LeVay showed that part of the sexually dimorphic nucleus (SDN) known as the 3rd interstitial nucleus of the anterior hypothalamus (INAH 3), is nearly twice as large (in terms of volume) in heterosexual men than in homosexual men and heterosexual women. However, a study in 1992 has shown that the sexually dimorph nucleus of the preoptic area, which include the INAH3, are of similar size in homosexual males who died of AIDS to heterosexual males, and therefore larger than female. This clearly contradicts the hypothesis that homosexual males have a female hypothalamus. Furthermore, the SCN of homosexual males is extremely large (both the volume and the number of neurons are twice as many as in heterosexual males). These areas of the hypothalamus have not yet been explored in homosexual females nor bisexual males nor females. Although the functional implications of such findings still haven't been examined in detail, they cast serious doubt over the widely accepted Dörner hypothesis that homosexual males have a "female hypothalamus" and that the key mechanism of differentiating the "male brain from originally female brain" is the epigenetic influence of testosterone during prenatal development.[31][32]
In 2004 and 2006, two studies by Berglund, Lindström, and Savic[33][34] used positron emission tomography (PET) to observe how the hypothalamus responds to smelling common odors, the scent of testosterone found in male sweat, and the scent of estrogen found in female urine. These studies showed that the hypothalamus of heterosexual men and homosexual women both respond to estrogen. Also, the hypothalamus of homosexual men and heterosexual women both respond to testosterone. The hypothalamus of all four groups did not respond to the common odors, which produced a normal olfactory response in the brain.
Clinical significance
Disease
- Hypothalamic disease A neuro-immunological disease called fibromyalgia syndrome appears to be some disorder of hypothalamus. All the issues of this disease except muscle stiffness is explainable by abnormal functioning of hypothalamus, for example, low metabolism, loss of appetite, changed emotional behavior, infertility, memory loss, low TSH resulting in hypothyroidism, lower serotonin and dopamine levels, sleep disorder.
See also
- Hypothalamic-pituitary-adrenal axis (HPA axis)
- Hypothalamic–pituitary–gonadal axis (HPG axis)
- Hypothalamic–pituitary–thyroid axis (HPT axis)
- John Leonora
- Incertohypothalamic pathway
- Neuroendocrinology
- Neuroscience of sleep
Additional images
-
-
Human brain left dissected midsagittal view
-

Location of the hypothalamus
References
- ↑ https://en.wikipedia.org/wiki/Limbic_system
- ↑ Definition of hypothalamus - NCI Dictionary of Cancer Terms
- ↑ Diagram of Nuclei (psycheducation.org)
- ↑ Diagram of Nuclei (universe-review.ca)
- ↑ Diagram of Nuclei (utdallas.edu)
- ↑ Unless else specified in table, then ref is: Guyton Twelfth Edition
- ↑ Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 6: Widely Projecting Systems: Monoamines, Acetylcholine, and Orexin". In Sydor A, Brown RY. Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 175–176. ISBN 9780071481274.
Within the brain, histamine is synthesized exclusively by neurons with their cell bodies in the tuberomammillary nucleus (TMN) that lies within the posterior hypothalamus. There are approximately 64000 histaminergic neurons per side in humans. These cells project throughout the brain and spinal cord. Areas that receive especially dense projections include the cerebral cortex, hippocampus, neostriatum, nucleus accumbens, amygdala, and hypothalamus. ... While the best characterized function of the histamine system in the brain is regulation of sleep and arousal, histamine is also involved in learning and memory ... It also appears that histamine is involved in the regulation of feeding and energy balance.
- ↑ Romeo, Russell D; Rudy Bellani, Ilia N. Karatsoreos, Nara Chhua, Mary Vernov, Cheryl D. Conrad and Bruce S. McEwen (2005). "Stress History and Pubertal Development Interact to Shape Hypothalamic-Pituitary-Adrenal Axis Plasticity". Endocrinology (The Endocrine Society) 147 (4): 1664–1674. doi:10.1210/en.2005-1432. PMID 16410296. Retrieved 3 November 2013.
- ↑ Bowen, R. "Overview of Hypothalamic and Pituitary Hormones". Retrieved 5 October 2014.
- ↑ Melmed S, Jameson JL (2005). "Disorders of the anterior pituitary and hypothalamus". In Kasper DL, Braunwald E, Fauci AS et al. Harrison's Principles of Internal Medicine (16th ed.). New York, NY: McGraw-Hill. pp. 2076–97. ISBN 0-07-139140-1.
- ↑ Ben-Shlomo, Anat; Melmed, Shlomo (28 February 2010). "Pituitary somatostatin receptor signaling". Trends in Endocrinology & Metabolism 21 (3): 123–133. doi:10.1016/j.tem.2009.12.003. PMC 2834886. PMID 20149677.
- ↑ Horn, A. M.; Robinson, I. C. A. F.; Fink, G. (1 February 1985). "Oxytocin and vasopressin in rat hypophysial portal blood: experimental studies in normal and Brattleboro rats". Journal of Endocrinology 104 (2): 211–NP. doi:10.1677/joe.0.1040211. PMID 3968510.
- ↑ Date, Y; Mondal, MS; Matsukura, S; Ueta, Y; Yamashita, H; Kaiya, H; Kangawa, K; Nakazato, M (Mar 10, 2000). "Distribution of orexin/hypocretin in the rat median eminence and pituitary.". Brain research. Molecular brain research 76 (1): 1–6. doi:10.1016/s0169-328x(99)00317-4. PMID 10719209.
- ↑ Watanobe, H; Takebe, K (April 1993). "In vivo release of neurotensin from the median eminence of ovariectomized estrogen-primed rats as estimated by push-pull perfusion: correlation with luteinizing hormone and prolactin surges.". Neuroendocrinology 57 (4): 760–4. doi:10.1159/000126434. PMID 8367038.
- ↑ Spinazzi, R; Andreis, PG; Rossi, GP; Nussdorfer, GG (March 2006). "Orexins in the regulation of the hypothalamic-pituitary-adrenal axis.". Pharmacological reviews 58 (1): 46–57. doi:10.1124/pr.58.1.4. PMID 16507882.
- ↑ Jung Eun Kim, Baik Kee Cho, Dae Ho Cho, and Hyun Jeong Park (2013). "Expression of Hypothalamic-Pituitary-Adrenal Axis in Common Skin Diseases: Evidence of its Association with Stress-related Disease Activity". National Research Foundation of Korea. Retrieved 4 March 2014.
- ↑ Fliers, Eric; Unmehopa, Alkemade (7 June 2006). "Functional neuroanatomy of thyroid hormone feedback in the human hypothalamus and pituitary gland". Molecular and Cellular Endocrinology 251 (1–2): 1–8. doi:10.1016/j.mce.2006.03.042. PMID 16707210.
- ↑ 18.0 18.1 18.2 Fauci, Anthony et al. (2008). Harrison's Principles of Internal Medicine (17 ed.). McGraw-Hill Professional. pp. 117–121. ISBN 978-0-07-146633-2.
- ↑ Theologides A (1976). "Anorexia-producing intermediary metabolites". Am J Clin Nutr 29 (5): 552–8. PMID 178168.
- ↑ Swanson, L.W. (2000). "Cerebral Hemisphere Regulation of Motivated Behavior". Brain Research 886: 113–164. doi:10.1016/S0006-8993(00)02905-X.
- ↑ Canteras, N.S. (2002). "The medial hypothalamic defensive system:Hodological organization and functional implications". Pharmacology, Biochemistry & Behavior 71: 481–491. doi:10.1016/S0091-3057(01)00685-2.
- ↑ Ribeiro-Barbosa, E.R.; et al. (2005). "An alternative experimental procedure for studying predator-related defensive responses.". Neuroscience & Biobehavioral Reviews 29 (8): 1255–1263. doi:10.1016/j.neubiorev.2005.04.006.
- ↑ 23.0 23.1 23.2 Cezário, A.F. (2008). "Hypothalamic sites responding to predator threats--the role of the dorsal premammillary nucleus in unconditioned and conditioned antipredatory defensive behavior.". European Journal of Neuroscience 28 (5): 1003–1015. doi:10.1111/j.1460-9568.2008.06392.x.
- ↑ 24.0 24.1 Blanchard, D.C. (2003). "Dorsal premammillary nucleus differentially modulates defensive behaviors induced by different threat stimuli in rats". Neuroscience Letters 345 (3): 145–148. doi:10.1016/S0304-3940(03)00415-4.
- ↑ Canteras, N.S.; Swanson, L.W. (1992). "The dorsal premammillary nucleus: an unusual component of the mammillary body.". PNAS 89 (21): 10089–10093. doi:10.1073/pnas.89.21.10089.
- ↑ Behbehani, M.M. (1995). "Functional characteristics of the midbrain periaqueductal gray.". Progress in Neurobiology 46 (6): 575–605. doi:10.1016/0301-0082(95)00009-K.
- ↑ 27.0 27.1 27.2 Motta, S.C.; et al. (2009). "Dissecting the brain's fear system reveals the hypothalamus is critical for responding in subordinate conspecific intruders." (PDF). PNAS 106 (12): 4870–4875. doi:10.1073/pnas.0900939106.
- ↑ Swaab DF (2008). "Sexual orientation and its basis in brain structure and function". PNAS 105 (30): 10273–10274. doi:10.1073/pnas.0805542105. PMC 2492513. PMID 18653758.
- ↑ Swaab DF, Hofman MA (1990). "An enlarged suprachiasmatic nucleus in homosexual men". Brain Res. 537 (1–2): 141–8. doi:10.1016/0006-8993(90)90350-K. PMID 2085769.
- ↑ Swaab DF, Slob AK, Houtsmuller EJ, Brand T, Zhou JN (1995). "Increased number of vasopressin neurons in the suprachiasmatic nucleus (SCN) of 'bisexual' adult male rats following perinatal treatment with the aromatase blocker ATD". Developmental Brain Research 85 (2): 273–279. doi:10.1016/0165-3806(94)00218-O. PMID 7600674.
- ↑ http://www.hiim.unizg.hr/images/knjiga/CNS41.pdf - Judaš, M., Kostović, I., The Fundamentals of Neuroscience, ch. 41, Neurobiology of emotions and sexuality, p. 408 (in Croatian)
- ↑ "Gender and sexual orientation in relation to hypothalamic structures.". Horm Res. 38 Suppl 2: 51–61. 1992. doi:10.1159/000182597. PMID 1292983.
- ↑ Savic I, Berglund H, Lindström P (2005). "Brain response to putative pheromones in homosexual men". PNAS 102 (20): 7356–7361. doi:10.1073/pnas.0407998102. PMC 1129091. PMID 15883379.
- ↑ Savic I, Berglund H, Lindström P (2006). "Brain response to putative pheromones in lesbian women". PNAS 103 (21): 8269–8274. doi:10.1073/pnas.0600331103. PMC 1570103. PMID 16705035.
Further reading
- de Vries, GJ, and Sodersten P (2009) Sex differences in the brain: the relation between structure and function. Hormones and Behavior 55:589-596.
External links
- Stained brain slice images which include the "Hypothalamus" at the BrainMaps project
- The Hypothalamus and Pituitary at endotexts.org
- NIF Search - Hypothalamus via the Neuroscience Information Framework
- Space-filling and cross-sectional diagrams of hypothalamic nuclei: right hypothalamus, anterior, tubular, posterior.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||


