Hypertension
| Hypertension | |
|---|---|
 Automated arm blood pressure meter showing arterial hypertension (shown a systolic blood pressure 158 mmHg, diastolic blood pressure 99 mmHg and heart rate of 80 beats per minute) | |
| Classification and external resources | |
| ICD-10 |
I10,I11,I12, I13,I15 |
| ICD-9 | 401 |
| OMIM | 145500 |
| DiseasesDB | 6330 |
| MedlinePlus | 000468 |
| eMedicine | med/1106 ped/1097 emerg/267 |
| Patient UK | Hypertension |
| MeSH | D006973 |
Hypertension (HTN or HT), also known as high blood pressure or arterial hypertension, is a chronic medical condition in which the blood pressure in the arteries is elevated. Blood pressure is expressed by two measurements, the systolic and diastolic pressures, which are the maximum and minimum pressures, respectively, in the arterial system. The systolic pressure occurs when the left ventricle is most contracted; the diastolic pressure occurs when the left ventricle is most relaxed prior to the next contraction. Normal blood pressure at rest is within the range of 100–140 mmHg systolic and 60–90 mmHg diastolic. Hypertension is present if the blood pressure is persistently at or above 140/90 millimeters mercury (mmHg) for most adults; different criteria apply to children.[1]
Hypertension usually does not cause symptoms initially, but sustained hypertension over time is a major risk factor for hypertensive heart disease, coronary artery disease,[2] stroke, aortic aneurysm, peripheral artery disease, and chronic kidney disease.
Hypertension is classified as either primary (essential) hypertension or secondary hypertension. About 90–95% of cases are categorized as primary hypertension, defined as high blood pressure with no obvious underlying cause.[3] The remaining 5–10% of cases are categorized as secondary hypertension, defined as hypertension due to an identifiable cause, such as chronic kidney disease, narrowing of the aorta or kidney arteries, or an endocrine disorder such as excess aldosterone, cortisol, or catecholamines.
Dietary and lifestyle changes can improve blood pressure control and decrease the risk of health complications, although treatment with medication is still often necessary in people for whom lifestyle changes are not enough or not effective. The treatment of moderately high arterial blood pressure (defined as >160/100 mmHg) with medications is associated with an improved life expectancy.[4][5] The benefits of treatment of blood pressure that is between 140/90 mmHg and 160/100 mmHg are less clear, with some reviews finding no benefit[4][5] and other reviews finding benefit.[6]
Signs and symptoms
Hypertension is rarely accompanied by any symptoms, and its identification is usually through screening, or when seeking healthcare for an unrelated problem. Some with high blood pressure report headaches (particularly at the back of the head and in the morning), as well as lightheadedness, vertigo, tinnitus (buzzing or hissing in the ears), altered vision or fainting episodes.[7] These symptoms, however, might be related to associated anxiety rather than the high blood pressure itself.[8]
On physical examination, hypertension may be associated with the presence of changes in the optic fundus seen by ophthalmoscopy.[9] The severity of the changes typical of hypertensive retinopathy is graded from I–IV; grades I and II may be difficult to differentiate.[9] The severity of the retinopathy correlates roughly with the duration and/or the severity of the hypertension.[7]
Secondary hypertension
Hypertension with certain specific additional signs and symptoms may suggest secondary hypertension, i.e. hypertension due to an identifiable cause. For example, Cushing's syndrome frequently causes truncal obesity, glucose intolerance, moon face, a hump of fat behind the neck/shoulder, and purple abdominal stretch marks.[10] Hyperthyroidism frequently causes weight loss with increased appetite, fast heart rate, bulging eyes, and tremor. Renal artery stenosis (RAS) may be associated with a localized abdominal bruit to the left or right of the midline (unilateral RAS), or in both locations (bilateral RAS). Coarctation of the aorta frequently causes a decreased blood pressure in the lower extremities relative to the arms, and/or delayed or absent femoral arterial pulses. . Pheochromocytoma may cause abrupt ("paroxysmal") hypertension accompanied by headache, palpitations, pale appearance, and excessive sweating.[10]
Hypertensive crisis
Severely elevated blood pressure (equal to or greater than a systolic 180 or diastolic of 110—sometimes termed malignant or accelerated hypertension) is referred to as a "hypertensive crisis", as blood pressure at this level confers a high risk of complications. People with blood pressures in this range may have no symptoms, but are more likely to report headaches (22% of cases)[11] and dizziness than the general population.[7] Other symptoms accompanying a hypertensive crisis may include visual deterioration due to retinopathy, breathlessness due to heart failure, or a general feeling of malaise due to kidney failure.[10] Most people with a hypertensive crisis are known to have elevated blood pressure, but additional triggers may have led to a sudden rise.[12]
A "hypertensive emergency" is diagnosed when there is evidence of direct damage to one or more organs as a result of severely elevated blood pressure greater than 180 systolic or 120 diastolic.[13] This may include hypertensive encephalopathy, caused by brain swelling and dysfunction, and characterized by headaches and an altered level of consciousness (confusion or drowsiness). Retinal papilledema and/or fundal bleeds and exudates are another sign of target organ damage. Chest pain may indicate heart muscle damage (which may progress to myocardial infarction) or sometimes aortic dissection, the tearing of the inner wall of the aorta. Breathlessness, cough, and the coughing up of blood-stained sputum are characteristic signs of pulmonary edema, the swelling of lung tissue due to left ventricular failure an inability of the left ventricle of the heart to adequately pump blood from the lungs into the arterial system.[12] Rapid deterioration of kidney function (acute kidney injury) and microangiopathic hemolytic anemia (destruction of blood cells) may also occur.[12] In these situations, rapid reduction of the blood pressure is mandated to stop ongoing organ damage.[12] In contrast there is no evidence that blood pressure needs to be lowered rapidly in hypertensive urgencies where there is no evidence of target organ damage and over aggressive reduction of blood pressure is not without risks.[10] Use of oral medications to lower the BP gradually over 24 to 48h is advocated in hypertensive urgencies.[12]
Pregnancy
Hypertension occurs in approximately 8–10% of pregnancies.[10] Two blood pressure measurements six hours apart of greater than 140/90 mm Hg is considered diagnostic of hypertension in pregnancy.[14] Most women with hypertension in pregnancy have pre-existing primary hypertension, but high blood pressure in pregnancy may be the first sign of pre-eclampsia, a serious condition of the second half of pregnancy and puerperium.[10] Pre-eclampsia is characterised by increased blood pressure and the presence of protein in the urine.[10] It occurs in about 5% of pregnancies and is responsible for approximately 16% of all maternal deaths globally.[10] Pre-eclampsia also doubles the risk of perinatal mortality.[10] Usually there are no symptoms in pre-eclampsia and it is detected by routine screening. When symptoms of pre-eclampsia occur the most common are headache, visual disturbance (often "flashing lights"), vomiting, epigastric pain, and edema. Pre-eclampsia can occasionally progress to a life-threatening condition called eclampsia, which is a hypertensive emergency and has several serious complications including vision loss, brain swelling, seizures or convulsions, kidney failure, pulmonary edema, and disseminated intravascular coagulation (a blood clotting disorder).[10][15]
Children
Failure to thrive, seizures, irritability, lack of energy, and difficulty breathing[16] can be associated with hypertension in neonates and young infants. In older infants and children, hypertension can cause headache, unexplained irritability, fatigue, failure to thrive, blurred vision, nosebleeds, and facial paralysis.[16][17]
Cause
Primary hypertension
Hypertension results from a complex interaction of genes and environmental factors. Numerous common genetic variants with small effects on blood pressure have been identified[18] as well as some rare genetic variants with large effects on blood pressure,[19] but the genetic basis of hypertension is still poorly understood.
Blood pressure rises with aging and the risk of becoming hypertensive in later life is considerable.[20] Several environmental factors influence blood pressure. High salt intake raises the blood pressure in salt sensitive individuals; lack of exercise, obesity, stress,[8] and depression[21] can play a role in individual cases. The possible role of other factors such as caffeine consumption,[22] and vitamin D deficiency[23] are less clear. Insulin resistance, which is common in obesity and is a component of syndrome X (or the metabolic syndrome), is also thought to contribute to hypertension.[24] Events in early life, such as low birth weight, maternal smoking, and lack of breast feeding may be risk factors for adult essential hypertension,[25] although the mechanisms linking these exposures to adult hypertension remain unclear.[25]
Secondary hypertension
Secondary hypertension results from an identifiable cause. Kidney disease is the most common secondary cause of hypertension.[10] Hypertension can also be caused by endocrine conditions, such as Cushing's syndrome, hyperthyroidism, hypothyroidism, acromegaly, Conn's syndrome or hyperaldosteronism, hyperparathyroidism and pheochromocytoma.[10][26] Other causes of secondary hypertension include obesity, sleep apnea, pregnancy, coarctation of the aorta, excessive liquorice consumption and certain prescription medicines, herbal remedies and illegal drugs.[10][27]
Pathophysiology


In most people with established essential (primary) hypertension, increased resistance to blood flow (total peripheral resistance) accounts for the high pressure while cardiac output remains normal.[28] There is evidence that some younger people with prehypertension or 'borderline hypertension' have high cardiac output, an elevated heart rate and normal peripheral resistance, termed hyperkinetic borderline hypertension.[29] These individuals develop the typical features of established essential hypertension in later life as their cardiac output falls and peripheral resistance rises with age.[29] Whether this pattern is typical of all people who ultimately develop hypertension is disputed.[30] The increased peripheral resistance in established hypertension is mainly attributable to structural narrowing of small arteries and arterioles,[31] although a reduction in the number or density of capillaries may also contribute.[32] Whether increased active arteriolar vasoconstriction plays a role in established essential hypertension is unclear.[33] Hypertension is also associated with decreased peripheral venous compliance[34] which may increase venous return, increase cardiac preload and, ultimately, cause diastolic dysfunction.
Pulse pressure (the difference between systolic and diastolic blood pressure) is frequently increased in older people with hypertension. This can mean that systolic pressure is abnormally high, but diastolic pressure may be normal or low — a condition termed isolated systolic hypertension.[35] The high pulse pressure in elderly people with hypertension or isolated systolic hypertension is explained by increased arterial stiffness, which typically accompanies aging and may be exacerbated by high blood pressure.[36]
Many mechanisms have been proposed to account for the rise in peripheral resistance in hypertension. Most evidence implicates either disturbances in the kidneys' salt and water handling (particularly abnormalities in the intrarenal renin-angiotensin system)[37] and/or abnormalities of the sympathetic nervous system.[38] These mechanisms are not mutually exclusive and it is likely that both contribute to some extent in most cases of essential hypertension. It has also been suggested that endothelial dysfunction and vascular inflammation may also contribute to increased peripheral resistance and vascular damage in hypertension.[39][40] Interleukin 17 has garnered interest for its role in increasing the production of several other immune system chemical signals thought to be involved in hypertension such as tumor necrosis factor alpha, interleukin 1, interleukin 6, and interleukin 8.[41]
Diagnosis
| System | Tests |
|---|---|
| Kidney | Microscopic urinalysis, protein in the urine, BUN and/or creatinine |
| Endocrine | Serum sodium, potassium, calcium, TSH |
| Metabolic | Fasting blood glucose, HDL, LDL, and total cholesterol, triglycerides |
| Other | Hematocrit, electrocardiogram, and chest radiograph |
| Sources: Harrison's principles of internal medicine[42] others[43][44][45][46][47] | |
Hypertension is diagnosed on the basis of a persistently high blood pressure. Traditionally, the National Institute of Clinical Excellence recommends three separate sphygmomanometer measurements at one monthly intervals.[48][49] The American Heart Association recommends at least three measurements on at least two separate health care visits.[50] An exception to this is those with very high blood pressure readings especially when there is poor organ function.[49] Initial assessment of the hypertensive people should include a complete history and physical examination. With the availability of 24-hour ambulatory blood pressure monitors and home blood pressure machines, the importance of not wrongly diagnosing those who have white coat hypertension has led to a change in protocols. In the United Kingdom, current best practice is to follow up a single raised clinic reading with ambulatory measurement, or less ideally with home blood pressure monitoring over the course of 7 days.[49] Pseudohypertension in the elderly or noncompressibility artery syndrome may also require consideration. This condition is believed to be due to calcification of the arteries resulting in abnormally high blood pressure readings with a blood pressure cuff while intra arterial measurements of blood pressure are normal.[51] Orthostatic hypertension is when blood pressure increases upon standing.[52]
Once the diagnosis of hypertension has been made, physicians will attempt to identify the underlying cause based on risk factors and other symptoms, if present. Secondary hypertension is more common in preadolescent children, with most cases caused by kidney disease. Primary or essential hypertension is more common in adolescents and has multiple risk factors, including obesity and a family history of hypertension.[53] Laboratory tests can also be performed to identify possible causes of secondary hypertension, and to determine whether hypertension has caused damage to the heart, eyes, and kidneys. Additional tests for diabetes and high cholesterol levels are usually performed because these conditions are additional risk factors for the development of heart disease and may require treatment.[3]
Serum creatinine is measured to assess for the presence of kidney disease, which can be either the cause or the result of hypertension. Serum creatinine alone may overestimate glomerular filtration rate and recent guidelines advocate the use of predictive equations such as the Modification of Diet in Renal Disease (MDRD) formula to estimate glomerular filtration rate (eGFR).[54] eGFR can also provide a baseline measurement of kidney function that can be used to monitor for side effects of certain antihypertensive drugs on kidney function. Additionally, testing of urine samples for protein is used as a secondary indicator of kidney disease. Electrocardiogram (EKG/ECG) testing is done to check for evidence that the heart is under strain from high blood pressure. It may also show whether there is thickening of the heart muscle (left ventricular hypertrophy) or whether the heart has experienced a prior minor disturbance such as a silent heart attack. A chest X-ray or an echocardiogram may also be performed to look for signs of heart enlargement or damage to the heart.[10]
Adults
| Classification (JNC7)[54] | Systolic pressure | Diastolic pressure | ||
|---|---|---|---|---|
| mmHg | kPa | mmHg | kPa | |
| Normal | 90–119 | 12–15.9 | 60–79 | 8.0–10.5 |
| High normal[55] (Prehypertension) | 120–139 | 16.0–18.5 | 80–89 | 10.7–11.9 |
| Stage 1 hypertension | 140–159 | 18.7–21.2 | 90–99 | 12.0–13.2 |
| Stage 2 hypertension | 160–179 | ≥21.3 | 100–109 | ≥13.3 |
| Stage 3 hypertension[56][57] (Hypertensive emergency) | ≥180 | ≥110 | ||
| Isolated systolic hypertension | ≥140 | ≥18.7 | <90 | <12.0 |
In people aged 18 years or older hypertension is defined as a systolic and/or a diastolic blood pressure measurement consistently higher than an accepted normal value (currently 139 mmHg systolic, 89 mmHg diastolic: see table —Classification (JNC7)). Lower thresholds are used (135 mmHg systolic or 85 mmHg diastolic) if measurements are derived from 24-hour ambulatory or home monitoring.[49] Recent international hypertension guidelines have also created categories below the hypertensive range to indicate a continuum of risk with higher blood pressures in the normal range. JNC7 (2003)[54] uses the term prehypertension for blood pressure in the range 120-139 mmHg systolic and/or 80-89 mmHg diastolic, while ESH-ESC Guidelines (2007)[56] and BHS IV (2004)[57] use optimal, normal and high normal categories to subdivide pressures below 140 mmHg systolic and 90 mmHg diastolic. Hypertension is also sub-classified: JNC7 distinguishes hypertension stage I, hypertension stage II, and isolated systolic hypertension. Isolated systolic hypertension refers to elevated systolic pressure with normal diastolic pressure and is common in the elderly.[54] The ESH-ESC Guidelines (2007)[56] and BHS IV (2004)[57] additionally define a third stage (stage III hypertension) for people with systolic blood pressure exceeding 179 mmHg or a diastolic pressure over 109 mmHg. Hypertension is classified as "resistant" if medications do not reduce blood pressure to normal levels.[54]
Children
Hypertension occurs in around 0.2 to 3% of newborns; however, blood pressure is not measured routinely in healthy newborns.[17] Hypertension is more common in high risk newborns. A variety of factors, such as gestational age, postconceptional age and birth weight needs to be taken into account when deciding if a blood pressure is normal in a newborn.[17]
Hypertension defined as elevated blood pressure over several visits affects 1% to 5% of children and adolescents and is associated with long term risks of ill-health.[58] Blood pressure rises with age in childhood and, in children, hypertension is defined as an average systolic or diastolic blood pressure on three or more occasions equal or higher than the 95th percentile appropriate for the sex, age and height of the child. High blood pressure must be confirmed on repeated visits however before characterizing a child as having hypertension.[58] Prehypertension in children has been defined as average systolic or diastolic blood pressure that is greater than or equal to the 90th percentile, but less than the 95th percentile.[58] In adolescents, it has been proposed that hypertension and pre-hypertension are diagnosed and classified using the same criteria as in adults.[58]
The value of routine screening for hypertension in children over the age of 3 years is debated.[59][60] In 2004 the National High Blood Pressure Education Program recommended that children aged 3 years and older have blood pressure measurement at least once at every health care visit[58] and the National Heart, Lung, and Blood Institute and American Academy of Pediatrics made a similar recommendation.[61] However, the American Academy of Family Physicians[62] support the view of the U.S. preventive Services Task Force that evidence is insufficient to determine the balance of benefits and harms of screening for hypertension in children and adolescents who do not have symptoms.[63]
Prevention
Much of the disease burden of high blood pressure is experienced by people who are not labelled as hypertensive.[57] Consequently, population strategies are required to reduce the consequences of high blood pressure and reduce the need for antihypertensive drug therapy. Lifestyle changes are recommended to lower blood pressure, before starting drug therapy. The 2004 British Hypertension Society guidelines[57] proposed the following lifestyle changes consistent with those outlined by the US National High BP Education Program in 2002[64] for the primary prevention of hypertension:
- maintain normal body weight for adults (e.g. body mass index 20–25 kg/m2)
- reduce dietary sodium intake to <100 mmol/ day (<6 g of sodium chloride or <2.4 g of sodium per day)
- engage in regular aerobic physical activity such as brisk walking (≥30 min per day, most days of the week)
- limit alcohol consumption to no more than 3 units/day in men and no more than 2 units/day in women
- consume a diet rich in fruit and vegetables (e.g. at least five portions per day);
Effective lifestyle modification may lower blood pressure as much as an individual antihypertensive drug. Combinations of two or more lifestyle modifications can achieve even better results.[57]
Management
Lifestyle modifications
The first line of treatment for hypertension is identical to the recommended preventive lifestyle changes[65] and includes dietary changes,[66] physical exercise, and weight loss. These have all been shown to significantly reduce blood pressure in people with hypertension.[67] Their potential effectiveness is similar to and at times exceeds a single medication.[55] If hypertension is high enough to justify immediate use of medications, lifestyle changes are still recommended in conjunction with medication.
Dietary change, such as a low sodium diet and a vegetarian diet are beneficial. A long term (more than 4 weeks) low sodium diet is effective in reducing blood pressure, both in people with hypertension and in people with normal blood pressure.[68] Also, the DASH diet, a diet rich in nuts, whole grains, fish, poultry, fruit and vegetables lowers blood pressure. A major feature of the plan is limiting intake of sodium, although the diet is also rich in potassium, magnesium, calcium, as well as protein.[69] A vegetarian diet is associated with a lower blood pressure and switching to such a diet may be useful for reducing high blood pressure.[70] A diet high in potassium lowers blood pressure in those with high blood pressure and may improve outcomes in those with normal kidney function.[71]
Some programs aimed to reduce psychological stress such as biofeedback or transcendental meditation may be reasonable add-ons to other treatment to reduce hypertension.[72] However several techniques, namely yoga, relaxation and other forms of meditation do not appear to reduce blood pressure,[73] and there are major methodological limitations with many studies of stress reduction techniques.[74] There is no clear evidence that the modest reduction in blood pressure with stress reduction techniques results in prevention of cardiovascular disease.[73][74]
Several exercise regimes—including isometric resistance exercise, aerobic exercise, resistance exercise, and device-guided breathing—may be useful in reducing blood pressure.[73]
Medications
Several classes of medications, collectively referred to as antihypertensive medications, are available for treating hypertension. Use should take into account the person's cardiovascular risk (including risk of myocardial infarction and stroke) as well as blood pressure readings, in order to gain a more accurate picture of the person's risks.[75] Benefit of medications is related to a person's cardiac disease risk.[76] Evidence for medications in those with mild hypertension (between 140/90 mmHg and 160/100 mmHg) and no other health problems is less clear with some reviews finding no benefit[4][5] and other reviews finding benefit.[6] Medications are not recommended for people with prehypertension or high normal blood pressure.[55]
If treatment with medication is initiated the Joint National Committee on High Blood Pressure (JNC-7)[54] recommended that the physician not only monitor for response to treatment but should also seek any side effects resulting from the medication. Reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34%, of ischaemic heart disease by 21%, and reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease.[77] For most people, recommendations are to reduce blood pressure to less than or equal to somewhere between 140/90 mmHg to 160/100 mmHg.[75][78] Attempting to achieve lower levels have not been shown to improve outcomes[78] while there is evidence that it increases side effects.[79] In those with diabetes or kidney disease some recommend levels below 120/80 mmHg;[75][80] however, evidence does not support these lower levels.[78][81] If the blood pressure goal is not met, a change in treatment should be made as therapeutic inertia is a clear impediment to blood pressure control.[82]
The best first line medication is disputed.[83] The Cochrane collaboration, World Health Organization and the United States guidelines support low dose thiazide-based diuretic as first line treatment.[1][67][83][84] The UK guidelines emphasise calcium channel blockers (CCB) in preference for people over the age of 55 years or if of African or Caribbean family origin, with angiotensin converting enzyme inhibitors (ACE-I) used first line for younger people.[85] In Japan starting with any one of six classes of medications including: CCB, ACEI/ARB, thiazide diuretics, beta-blockers, and alpha-blockers is deemed reasonable, while in Canada and Europe all of these but alpha-blockers are recommended as options.[55][83] When compared to placebo and other anti-hypertensive medications as first-line therapy for hypertension, beta-blockers have greater benefit in stroke reduction, but no difference on coronary heart disease or all-cause mortality.[86] However, three-quarters of active beta-blocker treatment in the randomised controlled trials included in the review were with atenolol and none with the newer vasodilating beta-blockers.[87]
Medication combinations
The majority of people require more than one medication to control their hypertension. In those with a systolic blood pressure greater than 160 mmHg or a diastolic blood pressure greater than 100 mmHg the American Heart Association recommends starting both a thiazide and an ACEI, ARB or CCB.[67] An ACEI and CCB combination can be used as well.[67]
Unacceptable combinations are non-dihydropyridine calcium blockers (such as verapamil or diltiazem) and beta-blockers, dual renin–angiotensin system blockade (e.g. angiotensin converting enzyme inhibitor + angiotensin receptor blocker), renin–angiotensin system blockers and beta-blockers, beta-blockers and centrally acting medications.[88] Combinations of an ACE-inhibitor or angiotensin II–receptor antagonist, a diuretic and an NSAID (including selective COX-2 inhibitors and non-prescribed medications such as ibuprofen) should be avoided whenever possible due to a high documented risk of acute kidney failure. The combination is known colloquially as a "triple whammy" in the Australian health industry.[65] Tablets containing fixed combinations of two classes of medications are available and while convenient for the people, may be best reserved for those who have been established on the individual components.[89] Additionally, the use of treatments with vasoactive agents for people with pulmonary hypertension with left heart disease or hypoxemic lung diseases may cause harm and unnecessary expense.[90]
Elderly
Treating moderate to severe hypertension decreases death rates and cardiovascular morbidity and mortality in people aged 60 and older.[91] The recommended BP goal is advised as <150/90 mm Hg with thiazide diuretic, CCB, ACEI, or ARB being the first line medication in the United States,[92] and in the revised UK guidelines calcium-channel blockers are advocated as first line with targets of clinic readings <150/90, or <145/85 on ambulatory or home blood pressure monitoring.[85]
There are no randomized clinical trials addressing the goal blood pressure of hypertensives over 79 years old. A recent review concluded that antihypertensive treatment reduced cardiovascular deaths and disease, but did not significantly reduce total death rates.[91] Two professional organizations have published guidelines for the management of hypertension in persons over 79 years old.[93][94]
Resistant hypertension
Resistant hypertension is defined as hypertension that remains above goal blood pressure in spite of using, at once, three antihypertensive medications belonging to different drug classes. Guidelines for treating resistant hypertension have been published in the UK[95] and US.[96] It has been proposed that a proportion of resistant hypertension may be the result of chronic high activity of the autonomic nervous system; this concept is known as "neurogenic hypertension".[97] Low adherence to treatment is an important cause of resistant hypertension.[98]
Epidemiology

no data
<110
110-220
220-330
330-440
440-550
550-660
|
660-770
770-880
880-990
990-1100
1100-1600
>1600
|
Adults
As of 2000, nearly one billion people or ~26% of the adult population of the world had hypertension.[100] It was common in both developed (333 million) and undeveloped (639 million) countries.[100] However, rates vary markedly in different regions with rates as low as 3.4% (men) and 6.8% (women) in rural India and as high as 68.9% (men) and 72.5% (women) in Poland.[101] In Europe hypertension occurs in about 30-45% of people as of 2013.[55]
In 1995 it was estimated that 43 million people in the United States had hypertension or were taking antihypertensive medication, almost 24% of the adult United States population.[102] The prevalence of hypertension in the United States is increasing and reached 29% in 2004.[103][104] As of 2006 hypertension affects 76 million US adults (34% of the population) and African American adults have among the highest rates of hypertension in the world at 44%.[105] It is more common in blacks and less in whites and Mexican Americans, rates increase with age, and is greater in the southeastern United States.[3][106] Hypertension is more common in men (though menopause tends to decrease this difference) and in those of low socioeconomic status.[3]
Children
Rates of high blood pressure in children and adolescents have increased in the last 20 years in the United States.[107] Childhood hypertension, particularly in preadolescents, is more often secondary to an underlying disorder than in adults. Kidney disease is the most common secondary cause of hypertension in children and adolescents. Nevertheless, primary or essential hypertension accounts for most cases.[108]
Outcomes

Hypertension is the most important preventable risk factor for premature death worldwide.[109] It increases the risk of ischemic heart disease[110] strokes,[10] peripheral vascular disease,[111] and other cardiovascular diseases, including heart failure, aortic aneurysms, diffuse atherosclerosis, chronic kidney disease, and pulmonary embolism.[10] Hypertension is also a risk factor for cognitive impairment and dementia.[10] Other complications include hypertensive retinopathy and hypertensive nephropathy.[54]
History
_Venenbild.jpg)
Measurement
Modern understanding of the cardiovascular system began with the work of physician William Harvey (1578–1657), who described the circulation of blood in his book "De motu cordis". The English clergyman Stephen Hales made the first published measurement of blood pressure in 1733.[112][113] However hypertension as a clinical entity came into being in 1896 with the invention of the cuff-based sphygmomanometer by Scipione Riva-Rocci in 1896.[114] This allowed the measurement of blood pressure in the clinic. In 1905, Nikolai Korotkoff improved the technique by describing the Korotkoff sounds that are heard when the artery is ausculated with a stethoscope while the sphygmomanometer cuff is deflated.[113]
Identification
The symptoms similar to symptoms of patients with hypertensive crisis are discussed in medieval Persian medical texts in the chapter of "fullness disease".[115] This symptoms include headache, heaviness in the head, sluggish movements, general redness and warm to touch feel of the body, prominent, distended and tense vessels, fullness of the pulse, distension of the skin, coloured and dense urine, loss of appetite, weak eyesight, impairment of thinking, yawning, drowsiness, vascular rupture, and hemorrhagic stroke.[116] Fullness disease was presumed to be due to an excessive amount of blood within the blood vessels.
Descriptions of hypertension as a disease came among others from Thomas Young in 1808 and especially Richard Bright in 1836.[112] The first report of elevated blood pressure in a person without evidence of kidney disease was made by Frederick Akbar Mahomed (1849–1884).[117]
Treatment
Historically the treatment for what was called the "hard pulse disease" consisted in reducing the quantity of blood by bloodletting or the application of leeches.[112] This was advocated by The Yellow Emperor of China, Cornelius Celsus, Galen, and Hippocrates.[112] The therapeutic approach for the treatment of hard pulse disease included changes in lifestyle (staying away from anger and sexual intercourse) and dietary program for patients (avoiding the consumption of wine, meat, and pastries, reducing the volume of food in a meal, maintaining a low-energy diet and the dietary usage of spinach and vinegar).
In the 19th and 20th centuries, before effective pharmacological treatment for hypertension became possible, three treatment modalities were used, all with numerous side-effects: strict sodium restriction (for example the rice diet[112]), sympathectomy (surgical ablation of parts of the sympathetic nervous system), and pyrogen therapy (injection of substances that caused a fever, indirectly reducing blood pressure).[112][118]
The first chemical for hypertension, sodium thiocyanate, was used in 1900 but had many side effects and was unpopular.[112] Several other agents were developed after the Second World War, the most popular and reasonably effective of which were tetramethylammonium chloride and its derivative hexamethonium; hydralazine; and reserpine (derived from the medicinal plant Rauwolfia serpentina). A major breakthrough was achieved with the discovery of the first well-tolerated orally available agents. The first was chlorothiazide, the first thiazide diuretic and developed from the antibiotic sulfanilamide, which became available in 1958.[112][119] Subsequently beta blockers, calcium channel blockers, angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers and renin inhibitors were developed as antihypertensive agents.
Society and culture
Awareness
The World Health Organization has identified hypertension, or high blood pressure, as the leading cause of cardiovascular mortality. The World Hypertension League (WHL), an umbrella organization of 85 national hypertension societies and leagues, recognized that more than 50% of the hypertensive population worldwide are unaware of their condition.[120] To address this problem, the WHL initiated a global awareness campaign on hypertension in 2005 and dedicated May 17 of each year as World Hypertension Day (WHD). Over the past three years, more national societies have been engaging in WHD and have been innovative in their activities to get the message to the public. In 2007, there was record participation from 47 member countries of the WHL. During the week of WHD, all these countries – in partnership with their local governments, professional societies, nongovernmental organizations and private industries – promoted hypertension awareness among the public through several media and public rallies. Using mass media such as Internet and television, the message reached more than 250 million people. As the momentum picks up year after year, the WHL is confident that almost all the estimated 1.5 billion people affected by elevated blood pressure can be reached.[121]
Economics
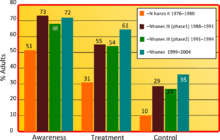
High blood pressure is the most common chronic medical problem prompting visits to primary health care providers in USA. The American Heart Association estimated the direct and indirect costs of high blood pressure in 2010 as $76.6 billion.[105] In the US 80% of people with hypertension are aware of their condition, 71% take some antihypertensive medication, but only 48% of people aware that they have hypertension adequately control it.[105] Adequate management of hypertension can be hampered by inadequacies in the diagnosis, treatment, and/or control of high blood pressure.[122] Health care providers face many obstacles to achieving blood pressure control, including resistance to taking multiple medications to reach blood pressure goals. People also face the challenges of adhering to medicine schedules and making lifestyle changes. Nonetheless, the achievement of blood pressure goals is possible, and most importantly, lowering blood pressure significantly reduces the risk of death due to heart disease and stroke, the development of other debilitating conditions, and the cost associated with advanced medical care.[123][124]
Research
Pregnancy
Regarding research in hypertension that occurs during pregnancy, it has been recommended that basic research be directed toward increasing understanding of the genetics and pathogenesis of oxidative stress in preeclampsia; and that clinical trials be initiated to assess which interventions are effective in preventing oxidative stress during pregnancy. Regarding the management of essential hypertension in the woman who becomes pregnant, the recommendation is that clinical trials be initiated to assess the effectiveness of various medication regimens, and their effect on mother and fetus.[125]
Non-drug treatment
Regarding research to find a more effective treatment for severe resistant hypertension: selective radiofrequency ablation is being used. It employs a catheter-based device to cause thermal injury to the sympathetic nerves surrounding the renal arteries, with the aim to reduce renal sympathetic overactivity (so-called "renal denervation") and thereby reduce blood pressure. It has been employed in clinical trials for resistant hypertension.[126] However, a prospective, single-blind, randomized, sham-controlled clinical trial failed to confirm a beneficial effect.[127] Infrequent renal artery dissection, femoral artery pseudoaneurysm, excessive decreases in blood pressure and heart rate have been reported.[128] A 2014 consensus statement from The Joint UK Societies recommended radiofrequency ablation not be used for the treatment of resistant hypertension,[129] but supported continuing clinical trials. Patient selection, with attention to measurement of pre- and post-procedure sympathetic nerve activity and norepinephrine levels, may help differentiate responders from non-responders to this procedure.[130]
Although considered an experimental treatment in the United States and the United Kingdom, it is an approved treatment in Europe, Australia, and Asia.[131][132]
References
- ↑ 1.0 1.1 James, PA.; Oparil, S.; Carter, BL.; Cushman, WC.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, DT.; Lefevre, ML. et al. (Dec 2013). "2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report From the Panel Members Appointed to the Eighth Joint National Committee (JNC 8)". JAMA 311 (5): 507–20. doi:10.1001/jama.2013.284427. PMID 24352797.
- ↑ Lewington, S; Clarke, R; Qizilbash, N; Peto, R; Collins, R; Prospective Studies, Collaboration (Dec 14, 2002). "Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies.". Lancet 360 (9349): 1903–13. doi:10.1016/s0140-6736(02)11911-8. PMID 12493255.
- ↑ 3.0 3.1 3.2 3.3 Carretero OA, Oparil S; Oparil (January 2000). "Essential hypertension. Part I: definition and etiology". Circulation 101 (3): 329–35. doi:10.1161/01.CIR.101.3.329. PMID 10645931.
- ↑ 4.0 4.1 4.2 Diao, D; Wright, JM; Cundiff, DK; Gueyffier, F (Aug 15, 2012). "Pharmacotherapy for mild hypertension.". The Cochrane database of systematic reviews 8: CD006742. doi:10.1002/14651858.CD006742.pub2. PMID 22895954.
- ↑ 5.0 5.1 5.2 Arguedas, JA; Leiva, V; Wright, JM (Oct 30, 2013). "Blood pressure targets for hypertension in people with diabetes mellitus.". The Cochrane database of systematic reviews 10: CD008277. doi:10.1002/14651858.cd008277.pub2. PMID 24170669.
- ↑ 6.0 6.1 Sundström, Johan; Arima, Hisatomi; Jackson, Rod; Turnbull, Fiona; Rahimi, Kazem; Chalmers, John; Woodward, Mark; Neal, Bruce (February 2015). "Effects of Blood Pressure Reduction in Mild Hypertension". Annals of Internal Medicine 162: 184–91. doi:10.7326/M14-0773. PMID 25531552.
- ↑ 7.0 7.1 7.2 Fisher ND, Williams GH (2005). "Hypertensive vascular disease". In Kasper DL, Braunwald E, Fauci AS et al. Harrison's Principles of Internal Medicine (16th ed.). New York, NY: McGraw-Hill. pp. 1463–81. ISBN 0-07-139140-1.
- ↑ 8.0 8.1 Marshall, IJ; Wolfe, CD; McKevitt, C (Jul 9, 2012). "Lay perspectives on hypertension and drug adherence: systematic review of qualitative research". BMJ (Clinical research ed.) 345: e3953. doi:10.1136/bmj.e3953. PMC 3392078. PMID 22777025.
- ↑ 9.0 9.1 Wong T, Mitchell P; Mitchell (February 2007). "The eye in hypertension". Lancet 369 (9559): 425–35. doi:10.1016/S0140-6736(07)60198-6. PMID 17276782.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 10.7 10.8 10.9 10.10 10.11 10.12 10.13 10.14 10.15 10.16 O'Brien, Eoin; Beevers, D. G.; Lip, Gregory Y. H. (2007). ABC of hypertension. London: BMJ Books. ISBN 1-4051-3061-X.
- ↑ Papadopoulos DP, Mourouzis I, Thomopoulos C, Makris T, Papademetriou V; Mourouzis; Thomopoulos; Makris; Papademetriou (December 2010). "Hypertension crisis". Blood Press. 19 (6): 328–36. doi:10.3109/08037051.2010.488052. PMID 20504242.
- ↑ 12.0 12.1 12.2 12.3 12.4 Marik PE, Varon J; Varon (June 2007). "Hypertensive crises: challenges and management". Chest 131 (6): 1949–62. doi:10.1378/chest.06-2490. PMID 17565029.
- ↑ Chobanian, AV; Bakris, GL; Black, HR; Cushman, WC; Green, LA; Izzo JL, Jr; Jones, DW; Materson, BJ; Oparil, S; Wright JT, Jr; Roccella, EJ; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood, Institute; National High Blood Pressure Education Program Coordinating, Committee (Dec 2003). "Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure". Hypertension 42 (6): 1206–52. doi:10.1161/01.hyp.0000107251.49515.c2. PMID 14656957.
- ↑ Harrison's principles of internal medicine. (18th ed.). New York: McGraw-Hill. 2011. pp. 55–61. ISBN 9780071748896.
- ↑ Gibson, Paul (July 30, 2009). "Hypertension and Pregnancy". eMedicine Obstetrics and Gynecology. Medscape. Retrieved 16 June 2009.
- ↑ 16.0 16.1 Rodriguez-Cruz, Edwin; Ettinger, Leigh M (April 6, 2010). "Hypertension". eMedicine Pediatrics: Cardiac Disease and Critical Care Medicine. Medscape. Retrieved 16 June 2009.
- ↑ 17.0 17.1 17.2 Dionne JM, Abitbol CL, Flynn JT; Abitbol; Flynn (January 2012). "Hypertension in infancy: diagnosis, management and outcome". Pediatr. Nephrol. 27 (1): 17–32. doi:10.1007/s00467-010-1755-z. PMID 21258818.
- ↑ Ehret GB; Munroe PB; Rice KM et al. (October 2011). "Genetic variants in novel pathways influence blood pressure and cardiovascular disease risk". Nature 478 (7367): 103–9. doi:10.1038/nature10405. PMC 3340926. PMID 21909115.
- ↑ Lifton, RP; Gharavi, AG, Geller, DS (2001-02-23). "Molecular mechanisms of human hypertension". Cell 104 (4): 545–56. doi:10.1016/S0092-8674(01)00241-0. PMID 11239411.
- ↑ Vasan, RS; Beiser, A; Seshadri, S; Larson, MG; Kannel, WB; D'Agostino, RB; Levy, D (2002-02-27). "Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study". JAMA: the Journal of the American Medical Association 287 (8): 1003–10. doi:10.1001/jama.287.8.1003. PMID 11866648.
- ↑ Meng, L; Chen, D; Yang, Y; Zheng, Y; Hui, R (May 2012). "Depression increases the risk of hypertension incidence: a meta-analysis of prospective cohort studies.". Journal of hypertension 30 (5): 842–51. doi:10.1097/hjh.0b013e32835080b7. PMID 22343537.
- ↑ Mesas, AE; Leon-Muñoz, LM; Rodriguez-Artalejo, F; Lopez-Garcia, E (October 2011). "The effect of coffee on blood pressure and cardiovascular disease in hypertensive individuals: a systematic review and meta-analysis". The American journal of clinical nutrition 94 (4): 1113–26. doi:10.3945/ajcn.111.016667. PMID 21880846.
- ↑ Vaidya A, Forman JP; Forman (November 2010). "Vitamin D and hypertension: current evidence and future directions". Hypertension 56 (5): 774–9. doi:10.1161/HYPERTENSIONAHA.109.140160. PMID 20937970.
- ↑ Sorof J, Daniels S; Daniels (October 2002). "Obesity hypertension in children: a problem of epidemic proportions". Hypertension 40 (4): 441–447. doi:10.1161/01.HYP.0000032940.33466.12. PMID 12364344. Retrieved 3 June 2009.
- ↑ 25.0 25.1 Lawlor, DA; Smith, GD (May 2005). "Early life determinants of adult blood pressure". Current Opinion in Nephrology and Hypertension 14 (3): 259–64. doi:10.1097/01.mnh.0000165893.13620.2b. PMID 15821420.
- ↑ Dluhy RG, Williams GH eds (1998). "Endocrine hypertension". In Wilson JD, Foster DW, Kronenberg HM. Williams textbook of endocrinology (9th ed.). Philadelphia ; Montreal: W.B. Saunders. pp. 729–49. ISBN 0721661521.
- ↑ Grossman E, Messerli FH; Messerli (January 2012). "Drug-induced Hypertension: An Unappreciated Cause of Secondary Hypertension". Am. J. Med. 125 (1): 14–22. doi:10.1016/j.amjmed.2011.05.024. PMID 22195528.
- ↑ Conway J (April 1984). "Hemodynamic aspects of essential hypertension in humans". Physiol. Rev. 64 (2): 617–60. PMID 6369352.
- ↑ 29.0 29.1 Palatini P, Julius S; Julius (June 2009). "The role of cardiac autonomic function in hypertension and cardiovascular disease". Curr. Hypertens. Rep. 11 (3): 199–205. doi:10.1007/s11906-009-0035-4. PMID 19442329.
- ↑ Andersson OK, Lingman M, Himmelmann A, Sivertsson R, Widgren BR; Lingman; Himmelmann; Sivertsson; Widgren (2004). "Prediction of future hypertension by casual blood pressure or invasive hemodynamics? A 30-year follow-up study". Blood Press. 13 (6): 350–4. doi:10.1080/08037050410004819. PMID 15771219.
- ↑ Folkow B (April 1982). "Physiological aspects of primary hypertension". Physiol. Rev. 62 (2): 347–504. PMID 6461865.
- ↑ Struijker Boudier HA, le Noble JL, Messing MW, Huijberts MS, le Noble FA, van Essen H; Le Noble; Messing; Huijberts; Le Noble; Van Essen (December 1992). "The microcirculation and hypertension". J Hypertens Suppl 10 (7): S147–56. doi:10.1097/00004872-199212000-00016. PMID 1291649.
- ↑ Schiffrin EL (February 1992). "Reactivity of small blood vessels in hypertension: relation with structural changes. State of the art lecture". Hypertension 19 (2 Suppl): II1–9. doi:10.1161/01.HYP.19.2_Suppl.II1-a. PMID 1735561.
- ↑ Safar ME, London GM; London (August 1987). "Arterial and venous compliance in sustained essential hypertension". Hypertension 10 (2): 133–9. doi:10.1161/01.HYP.10.2.133. PMID 3301662.
- ↑ Chobanian AV (August 2007). "Clinical practice. Isolated systolic hypertension in the elderly". N. Engl. J. Med. 357 (8): 789–96. doi:10.1056/NEJMcp071137. PMID 17715411.
- ↑ Zieman SJ, Melenovsky V, Kass DA; Melenovsky; Kass (May 2005). "Mechanisms, pathophysiology, and therapy of arterial stiffness". Arterioscler. Thromb. Vasc. Biol. 25 (5): 932–43. doi:10.1161/01.ATV.0000160548.78317.29. PMID 15731494.
- ↑ Navar LG (December 2010). "Counterpoint: Activation of the intrarenal renin-angiotensin system is the dominant contributor to systemic hypertension". J. Appl. Physiol. 109 (6): 1998–2000; discussion 2015. doi:10.1152/japplphysiol.00182.2010a. PMC 3006411. PMID 21148349.
- ↑ Esler M, Lambert E, Schlaich M; Lambert; Schlaich (December 2010). "Point: Chronic activation of the sympathetic nervous system is the dominant contributor to systemic hypertension". J. Appl. Physiol. 109 (6): 1996–8; discussion 2016. doi:10.1152/japplphysiol.00182.2010. PMID 20185633.
- ↑ Versari D, Daghini E, Virdis A, Ghiadoni L, Taddei S; Daghini; Virdis; Ghiadoni; Taddei (June 2009). "Endothelium-dependent contractions and endothelial dysfunction in human hypertension". Br. J. Pharmacol. 157 (4): 527–36. doi:10.1111/j.1476-5381.2009.00240.x. PMC 2707964. PMID 19630832.
- ↑ Marchesi C, Paradis P, Schiffrin EL; Paradis; Schiffrin (July 2008). "Role of the renin-angiotensin system in vascular inflammation". Trends Pharmacol. Sci. 29 (7): 367–74. doi:10.1016/j.tips.2008.05.003. PMID 18579222.
- ↑ Gooch JL, Sharma AC; Sharma (July 2014). "Targeting the immune system to treat hypertension: where are we?". Curr Opin Nephrol Hypertens 23 (5): 000–000. doi:10.1097/MNH.0000000000000052. PMID 25036747.
- ↑ Loscalzo, Joseph; Fauci, Anthony S.; Braunwald, Eugene; Dennis L. Kasper; Hauser, Stephen L; Longo, Dan L. (2008). Harrison's principles of internal medicine. McGraw-Hill Medical. ISBN 0-07-147691-1.
- ↑ Padwal RS; Hemmelgarn BR; Khan NA et al. (May 2009). "The 2009 Canadian Hypertension Education Program recommendations for the management of hypertension: Part 1 – blood pressure measurement, diagnosis and assessment of risk". Canadian Journal of Cardiology 25 (5): 279–86. doi:10.1016/S0828-282X(09)70491-X. PMC 2707176. PMID 19417858.
- ↑ Padwal RJ; Hemmelgarn BR; Khan NA et al. (June 2008). "The 2008 Canadian Hypertension Education Program recommendations for the management of hypertension: Part 1 – blood pressure measurement, diagnosis and assessment of risk". Canadian Journal of Cardiology 24 (6): 455–63. doi:10.1016/S0828-282X(08)70619-6. PMC 2643189. PMID 18548142.
- ↑ Padwal RS; Hemmelgarn BR; McAlister FA et al. (May 2007). "The 2007 Canadian Hypertension Education Program recommendations for the management of hypertension: Part 1 – blood pressure measurement, diagnosis and assessment of risk". Canadian Journal of Cardiology 23 (7): 529–38. doi:10.1016/S0828-282X(07)70797-3. PMC 2650756. PMID 17534459.
- ↑ Hemmelgarn BR; McAlister FA; Grover S et al. (May 2006). "The 2006 Canadian Hypertension Education Program recommendations for the management of hypertension: Part I – Blood pressure measurement, diagnosis and assessment of risk". Canadian Journal of Cardiology 22 (7): 573–81. doi:10.1016/S0828-282X(06)70279-3. PMC 2560864. PMID 16755312.
- ↑ Hemmelgarn BR; McAllister FA; Myers MG et al. (June 2005). "The 2005 Canadian Hypertension Education Program recommendations for the management of hypertension: part 1- blood pressure measurement, diagnosis and assessment of risk". Canadian Journal of Cardiology 21 (8): 645–56. PMID 16003448.
- ↑ North of England Hypertension Guideline Development Group (1 August 2004). "Frequency of measurements". Essential hypertension (NICE CG18) (PDF). National Institute for Health and Clinical Excellence. p. 53. Retrieved 22 December 2011.
- ↑ 49.0 49.1 49.2 49.3 National Clinical Guideline Centre (August 2011). "7 Diagnosis of Hypertension, 7.5 Link from evidence to recommendations". Hypertension (NICE CG 127) (PDF). National Institute for Health and Clinical Excellence. p. 102. Retrieved 22 December 2011.
- ↑ Aronow, WS; Fleg, JL; Pepine, CJ; Artinian, NT; Bakris, G; Brown, AS; Ferdinand, KC; Ann Forciea, M; Frishman, WH; Jaigobin, C; Kostis, JB; Mancia, G; Oparil, S; Ortiz, E; Reisin, E; Rich, MW; Schocken, DD; Weber, MA; Wesley, DJ; Harrington, RA; Bates, ER; Bhatt, DL; Bridges, CR; Eisenberg, MJ; Ferrari, VA; Fisher, JD; Gardner, TJ; Gentile, F; Gilson, MF; Hlatky, MA; Jacobs, AK; Kaul, S; Moliterno, DJ; Mukherjee, D; Rosenson, RS; Stein, JH; Weitz, HH; Wesley, DJ (Jul–Aug 2011). "ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension". Journal of the American Society of Hypertension : JASH 5 (4): 259–352. doi:10.1016/j.jash.2011.06.001. PMID 21771565.
- ↑ Franklin, SS; Wilkinson, IB; McEniery, CM (February 2012). "Unusual hypertensive phenotypes: what is their significance?". Hypertension 59 (2): 173–8. doi:10.1161/HYPERTENSIONAHA.111.182956. PMID 22184330.
- ↑ Kario, K (Jun 2009). "Orthostatic hypertension: a measure of blood pressure variation for predicting cardiovascular risk.". Circulation journal : official journal of the Japanese Circulation Society 73 (6): 1002–7. PMID 19430163.
- ↑ Luma GB, Spiotta RT; Spiotta (May 2006). "Hypertension in children and adolescents". Am Fam Physician 73 (9): 1558–68. PMID 16719248.
- ↑ 54.0 54.1 54.2 54.3 54.4 54.5 54.6 Chobanian AV; Bakris GL; Black HR; Cushman WC; Green LA; Izzo Jr. JL; Jones DW; Materson BJ; Oparil S; Wright Jr. JT; Roccella EJ et al. (December 2003). "Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure". Hypertension (Joint National Committee On Prevention) 42 (6): 1206–52. doi:10.1161/01.HYP.0000107251.49515.c2. PMID 14656957.
- ↑ 55.0 55.1 55.2 55.3 55.4 Giuseppe, Mancia; Fagard, R; Narkiewicz, K; Redon, J; Zanchetti, A; Bohm, M; Christiaens, T; Cifkova, R; De Backer, G; Dominiczak, A; Galderisi, M; Grobbee, DE; Jaarsma, T; Kirchhof, P; Kjeldsen, SE; Laurent, S; Manolis, AJ; Nilsson, PM; Ruilope, LM; Schmieder, RE; Sirnes, PA; Sleight, P; Viigimaa, M; Waeber, B; Zannad, F; Redon, J; Dominiczak, A; Narkiewicz, K; Nilsson, PM et al. (July 2013). "2013 ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)". European heart journal 34 (28): 2159–219. doi:10.1093/eurheartj/eht151. PMID 23771844.
- ↑ 56.0 56.1 56.2 Mancia G; De Backer G; Dominiczak A et al. (September 2007). "2007 ESH-ESC Practice Guidelines for the Management of Arterial Hypertension: ESH-ESC Task Force on the Management of Arterial Hypertension". J. Hypertens. 25 (9): 1751–62. doi:10.1097/HJH.0b013e3282f0580f. PMID 17762635.
- ↑ 57.0 57.1 57.2 57.3 57.4 57.5 Williams, B; Poulter, NR, Brown, MJ, Davis, M, McInnes, GT, Potter, JF, Sever, PS, McG Thom, S, British Hypertension, Society (March 2004). "Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004-BHS IV". Journal of Human Hypertension 18 (3): 139–85. doi:10.1038/sj.jhh.1001683. PMID 14973512.
- ↑ 58.0 58.1 58.2 58.3 58.4 National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (August 2004). "The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents". Pediatrics 114 (2 Suppl 4th Report): 555–76. doi:10.1542/peds.114.2.S2.555. PMID 15286277.
- ↑ Chiolero, A; Bovet, P; Paradis, G (Mar 1, 2013). "Screening for elevated blood pressure in children and adolescents: a critical appraisal.". JAMA pediatrics 167 (3): 266–73. doi:10.1001/jamapediatrics.2013.438. PMID 23303490.
- ↑ Daniels, SR.; Gidding, SS. (Mar 2013). "Blood pressure screening in children and adolescents: is the glass half empty or more than half full?". JAMA Pediatr 167 (3): 302–4. doi:10.1001/jamapediatrics.2013.439. PMID 23303514.
- ↑ Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute (Dec 2011). "Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report". Pediatrics. 128 Suppl 5: S213–56. doi:10.1542/peds.2009-2107C. PMID 22084329.
- ↑ http://www.aafp.org/patient-care/clinical-recommendations/all/hypertension.html
- ↑ Moyer, VA.; U.S. Preventive Services Task Force (October 2013). "Screening for Primary Hypertension in Children and Adolescents: U.S. Preventive Services Task Force Recommendation Statement*". Annals of Internal Medicine 159 (9): 613–9. doi:10.7326/0003-4819-159-9-201311050-00725. PMID 24097285.
- ↑ Whelton PK et al. (2002). "Primary prevention of hypertension. Clinical and public health advisory from the National High Blood Pressure Education Program". JAMA 288 (15): 1882–1888. doi:10.1001/jama.288.15.1882. PMID 12377087.
- ↑ 65.0 65.1 "NPS Prescribing Practice Review 52: Treating hypertension". NPS Medicines Wise. September 1, 2010. Retrieved 5 November 2010.
- ↑ Siebenhofer, A; Jeitler, K; Berghold, A; Waltering, A; Hemkens, LG; Semlitsch, T; Pachler, C; Strametz, R; Horvath, K (2011-09-07). Siebenhofer, Andrea, ed. "Long-term effects of weight-reducing diets in hypertensive patients". Cochrane Database of Systematic Reviews 9 (9): CD008274. doi:10.1002/14651858.CD008274.pub2. PMID 21901719.
- ↑ 67.0 67.1 67.2 67.3 Go, AS; Bauman, M; King, SM; Fonarow, GC; Lawrence, W; Williams, KA; Sanchez, E (Nov 15, 2013). "An Effective Approach to High Blood Pressure Control: A Science Advisory From the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention". Hypertension 63 (4): 878–885. doi:10.1161/HYP.0000000000000003. PMID 24243703.
- ↑ He, FJ; MacGregor, GA (2004). MacGregor, Graham A, ed. "Effect of longer-term modest salt reduction on blood pressure". Cochrane Database of Systematic Reviews (3): CD004937. doi:10.1002/14651858.CD004937. PMID 15266549.
- ↑ "Your Guide To Lowering Your Blood Pressure With DASH" (PDF). Retrieved 8 June 2009.
- ↑ Yokoyama, Yoko; Nishimura, Kunihiro; Barnard, Neal D.; Takegami, Misa; Watanabe, Makoto; Sekikawa, Akira; Okamura, Tomonori; Miyamoto, Yoshihiro (2014). "Vegetarian Diets and Blood Pressure". JAMA Internal Medicine 174 (4): 577. doi:10.1001/jamainternmed.2013.14547. ISSN 2168-6106.
- ↑ Aburto, NJ; Hanson, S; Gutierrez, H; Hooper, L; Elliott, P; Cappuccio, FP (3 April 2013). "Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses.". BMJ (Clinical research ed.) 346: f1378. doi:10.1136/bmj.f1378. PMID 23558164.
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/22855971
- ↑ 73.0 73.1 73.2 Brook, RD; Appel, LJ; Rubenfire, M; Ogedegbe, G; Bisognano, JD; Elliott, WJ; Fuchs, FD; Hughes, JW; Lackland, DT; Staffileno, BA; Townsend, RR; Rajagopalan, S; American Heart Association Professional Education Committee of the Council for High Blood Pressure Research, Council on Cardiovascular and Stroke Nursing, Council on Epidemiology and Prevention, and Council on Nutrition, Physical, Activity (Jun 2013). "Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the american heart association". Hypertension 61 (6): 1360–83. doi:10.1161/HYP.0b013e318293645f. PMID 23608661.
- ↑ 74.0 74.1 Nagele, Eva; Jeitler, Klaus; Horvath, Karl; Semlitsch, Thomas; Posch, Nicole; Herrmann, Kirsten H.; Grouven, Ulrich; Hermanns, Tatjana; Hemkens, Lars G.; Siebenhofer, Andrea (2014). "Clinical effectiveness of stress-reduction techniques in patients with hypertension". Journal of Hypertension 32 (10): 1936–1944. doi:10.1097/HJH.0000000000000298. ISSN 0263-6352.
- ↑ 75.0 75.1 75.2 Nelson, Mark. "Drug treatment of elevated blood pressure". Australian Prescriber (33): 108–112. Retrieved 11 August 2010.
- ↑ Blood Pressure Lowering Treatment Trialists', Collaboration; Sundström, J; Arima, H; Woodward, M; Jackson, R; Karmali, K; Lloyd-Jones, D; Baigent, C; Emberson, J; Rahimi, K; MacMahon, S; Patel, A; Perkovic, V; Turnbull, F; Neal, B (Aug 16, 2014). "Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data.". Lancet 384 (9943): 591–8. doi:10.1016/s0140-6736(14)61212-5. PMID 25131978.
- ↑ Law M, Wald N, Morris J; Wald; Morris (2003). "Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy" (PDF). Health Technol Assess 7 (31): 1–94. doi:10.3310/hta7310. PMID 14604498.
- ↑ 78.0 78.1 78.2 Arguedas, JA; Perez, MI; Wright, JM (Jul 8, 2009). Arguedas, Jose Agustin, ed. "Treatment blood pressure targets for hypertension". Cochrane Database of Systematic Reviews (3): CD004349. doi:10.1002/14651858.CD004349.pub2. PMID 19588353.
- ↑ "Treating blood pressure between 140/90 and 160/95 mmHg: no proven benefit.". Prescrire Int 148 (23): 106. April 2014. PMID 24860904.
- ↑ Shaw, Gina (2009-03-07). "Prehypertension: Early-stage High Blood Pressure". WebMD. Retrieved 3 July 2009.
- ↑ Arguedas, JA; Leiva, V; Wright, JM (Oct 30, 2013). "Blood pressure targets for hypertension in people with diabetes mellitus.". The Cochrane database of systematic reviews 10: CD008277. doi:10.1002/14651858.cd008277.pub2. PMID 24170669.
- ↑ Eni C. Okonofua; Kit N. Simpson; Ammar Jesri; Shakaib U. Rehman; Valerie L. Durkalski; Brent M. Egan (January 23, 2006). "Therapeutic Inertia Is an Impediment to Achieving the Healthy People 2010 Blood Pressure Control Goals". Hypertension 47 (2006;47:345): 345–51. doi:10.1161/01.HYP.0000200702.76436.4b. PMID 16432045. Retrieved 22 November 2009.
- ↑ 83.0 83.1 83.2 Klarenbach, SW; McAlister, FA, Johansen, H, Tu, K, Hazel, M, Walker, R, Zarnke, KB, Campbell, NR, Canadian Hypertension Education, Program (May 2010). "Identification of factors driving differences in cost effectiveness of first-line pharmacological therapy for uncomplicated hypertension". The Canadian journal of cardiology 26 (5): e158–63. doi:10.1016/S0828-282X(10)70383-4. PMC 2886561. PMID 20485695.
- ↑ Wright JM, Musini VM; Musini (2009). Wright, James M, ed. "First-line drugs for hypertension". Cochrane Database of Systematic Reviews (3): CD001841. doi:10.1002/14651858.CD001841.pub2. PMID 19588327.
- ↑ 85.0 85.1 National Institute Clinical Excellence (August 2011). "1.5 Initiating and monitoring antihypertensive drug treatment, including blood pressure targets". GC127 Hypertension: Clinical management of primary hypertension in adults. Retrieved 23 December 2011.
- ↑ Wiysonge, CS; Bradley, HA; Volmink, J; Mayosi, BM; Mbewu, A; Opie, LH (Nov 14, 2012). "Beta-blockers for hypertension". The Cochrane database of systematic reviews 11: CD002003. doi:10.1002/14651858.CD002003.pub4. PMID 23152211.
- ↑ Opie, LH; Wiysonge, CS (Feb 26, 2014). "β-Blocker therapy for patients with hypertension--reply.". JAMA: the Journal of the American Medical Association 311 (8): 862–3. doi:10.1001/jama.2014.336. PMID 24570254.
- ↑ Sever PS, Messerli FH; Messerli (October 2011). "Hypertension management 2011: optimal combination therapy". Eur. Heart J. 32 (20): 2499–506. doi:10.1093/eurheartj/ehr177. PMID 21697169.
- ↑ "2.5.5.1 Angiotensin-converting enzyme inhibitors". British National Formulary. No. 62. September 2011.
- ↑ American College of Chest Physicians; American Thoracic Society (September 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation (American College of Chest Physicians and American Thoracic Society), retrieved 6 January 2013
- ↑ 91.0 91.1 Musini VM, Tejani AM, Bassett K, Wright JM; Tejani; Bassett; Wright (2009). Musini, Vijaya M, ed. "Pharmacotherapy for hypertension in the elderly". Cochrane Database of Systematic Reviews (4): CD000028. doi:10.1002/14651858.CD000028.pub2. PMID 19821263.
- ↑ James, Paul A.; Oparil, Suzanne; Carter, Barry L.; Cushman, William C.; Dennison-Himmelfarb, Cheryl; Handler, Joel; Lackland, Daniel T.; LeFevre, Michael L.; MacKenzie, Thomas D.; Ogedegbe, Olugbenga; Smith, Sidney C.; Svetkey, Laura P.; Taler, Sandra J.; Townsend, Raymond R.; Wright, Jackson T.; Narva, Andrew S.; Ortiz, Eduardo (18 December 2013). "2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults". JAMA 311 (5): 507–20. doi:10.1001/jama.2013.284427. PMID 24352797.
- ↑ Aronow WS, Fleg JL, Pepine CJ, Artinian NT, Bakris G, Brown AS, Ferdinand KC, Forciea MA, Frishman WH, Jaigobin C, Kostis JB, Mancia G, Oparil S, Ortiz E, Reisin E, Rich MW, Schocken DD, Weber MA, Wesley DJ, Harrington RA; ACCF Task Force (May 2011). "ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents". Circulation 123 (21): 2434–506. doi:10.1161/CIR.0b013e31821daaf6. PMID 21518977.
- ↑ Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F; Task Force Members (July 2013). "2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)". Journal of Hypertension 31 (7): 1281–357. doi:10.1097/01.hjh.0000431740.32696.cc. PMID 23817082.
- ↑ "CG34 Hypertension - quick reference guide" (PDF). National Institute for Health and Clinical Excellence. 28 June 2006. Retrieved 4 March 2009.
- ↑ Calhoun DA; Jones D; Textor S et al. (June 2008). "Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research". Hypertension 51 (6): 1403–19. doi:10.1161/HYPERTENSIONAHA.108.189141. PMID 18391085.
- ↑ Zubcevic J, Waki H, Raizada MK, Paton JF; Waki; Raizada; Paton (June 2011). "Autonomic-immune-vascular interaction: an emerging concept for neurogenic hypertension". Hypertension 57 (6): 1026–33. doi:10.1161/HYPERTENSIONAHA.111.169748. PMC 3105900. PMID 21536990.
- ↑ Santschi, V; Chiolero, A; Burnier, M (Nov 2009). "Electronic monitors of drug adherence: tools to make rational therapeutic decisions.". Journal of hypertension 27 (11): 2294–5; author reply 2295. doi:10.1097/hjh.0b013e328332a501. PMID 20724871.
- ↑ "WHO Disease and injury country estimates". World Health Organization. 2009. Retrieved 11 November 2009.
- ↑ 100.0 100.1 Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J; Whelton; Reynolds; Muntner; Whelton; He (2005). "Global burden of hypertension: analysis of worldwide data". Lancet 365 (9455): 217–23. doi:10.1016/S0140-6736(05)17741-1. PMID 15652604.
- ↑ Kearney PM, Whelton M, Reynolds K, Whelton PK, He J; Whelton; Reynolds; Whelton; He (January 2004). "Worldwide prevalence of hypertension: a systematic review". J. Hypertens. 22 (1): 11–9. doi:10.1097/00004872-200401000-00003. PMID 15106785.
- ↑ Burt VL; Whelton P; Roccella EJ et al. (March 1995). "Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988–1991". Hypertension 25 (3): 305–13. doi:10.1161/01.HYP.25.3.305. PMID 7875754. Retrieved 5 June 2009.
- ↑ 103.0 103.1 Burt VL; Cutler JA; Higgins M et al. (July 1995). "Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population. Data from the health examination surveys, 1960 to 1991". Hypertension 26 (1): 60–9. doi:10.1161/01.HYP.26.1.60. PMID 7607734. Retrieved 5 June 2009.
- ↑ Ostchega Y, Dillon CF, Hughes JP, Carroll M, Yoon S; Dillon; Hughes; Carroll; Yoon (July 2007). "Trends in hypertension prevalence, awareness, treatment, and control in older U.S. adults: data from the National Health and Nutrition Examination Survey 1988 to 2004". Journal of the American Geriatrics Society 55 (7): 1056–65. doi:10.1111/j.1532-5415.2007.01215.x. PMID 17608879.
- ↑ 105.0 105.1 105.2 Lloyd-Jones D; Adams RJ; Brown TM et al. (February 2010). "Heart disease and stroke statistics--2010 update: a report from the American Heart Association". Circulation 121 (7): e46–e215. doi:10.1161/CIRCULATIONAHA.109.192667. PMID 20019324.
- ↑ "Culture-Specific of Health Risk". Stanford. Retrieved 12 April 2014.
- ↑ Falkner B (May 2009). "Hypertension in children and adolesents: epidemiology and natural history". Pediatr. Nephrol. 25 (7): 1219–24. doi:10.1007/s00467-009-1200-3. PMC 2874036. PMID 19421783.
- ↑ Luma GB, Spiotta RT; Spiotta (May 2006). "Hypertension in children and adolescents". Am Fam Physician 73 (9): 1558–68. PMID 16719248.
- ↑ "Global health risks: mortality and burden of disease attributable to selected major risks" (PDF). World Health Organization. 2009. Retrieved 10 February 2012.
- ↑ Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Clarke; Qizilbash; Peto; Collins; Prospective Studies (December 2002). "Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies". Lancet 360 (9349): 1903–13. doi:10.1016/S0140-6736(02)11911-8. PMID 12493255.
- ↑ Singer DR, Kite A; Kite (June 2008). "Management of hypertension in peripheral arterial disease: does the choice of drugs matter?". European Journal of Vascular and Endovascular Surgery 35 (6): 701–8. doi:10.1016/j.ejvs.2008.01.007. PMID 18375152.
- ↑ 112.0 112.1 112.2 112.3 112.4 112.5 112.6 112.7 Esunge PM (October 1991). "From blood pressure to hypertension: the history of research". J R Soc Med 84 (10): 621. PMC 1295564. PMID 1744849.
- ↑ 113.0 113.1 Kotchen TA (October 2011). "Historical trends and milestones in hypertension research: a model of the process of translational research". Hypertension 58 (4): 522–38. doi:10.1161/HYPERTENSIONAHA.111.177766. PMID 21859967.
- ↑ Postel-Vinay N, ed. (1996). A century of arterial hypertension 1896–1996. Chichester: Wiley. p. 213. ISBN 0-471-96788-2.
- ↑ "The medieval origins of the concept of hypertension". Heart Views 15 (3): 96–98. 2014. doi:10.4103/1995-705X.144807. Retrieved 25 November 2014.
- ↑ "Avicenna's doctrine about arterial hypertension.". Acta Med Hist Adriat 12: 157–62. 2014. PMID 25310615. Retrieved 25 November 2014.
- ↑ Swales JD, ed. (1995). Manual of hypertension. Oxford: Blackwell Science. pp. xiii. ISBN 0-86542-861-1.
- ↑ Dustan HP, Roccella EJ, Garrison HH; Roccella; Garrison (September 1996). "Controlling hypertension. A research success story". Arch. Intern. Med. 156 (17): 1926–35. doi:10.1001/archinte.156.17.1926. PMID 8823146.
- ↑ Novello FC, Sprague JM; Sprague (1957). "Benzothiadiazine dioxides as novel diuretics". J. Am. Chem. Soc. 79 (8): 2028–2029. doi:10.1021/ja01565a079.
- ↑ Chockalingam A (May 2007). "Impact of World Hypertension Day". Canadian Journal of Cardiology 23 (7): 517–9. doi:10.1016/S0828-282X(07)70795-X. PMC 2650754. PMID 17534457.
- ↑ Chockalingam A (June 2008). "World Hypertension Day and global awareness". Canadian Journal of Cardiology 24 (6): 441–4. doi:10.1016/S0828-282X(08)70617-2. PMC 2643187. PMID 18548140.
- ↑ Alcocer L, Cueto L; Cueto (June 2008). "Hypertension, a health economics perspective". Therapeutic Advances in Cardiovascular Disease 2 (3): 147–55. doi:10.1177/1753944708090572. PMID 19124418. Retrieved 20 June 2009.
- ↑ William J. Elliott (October 2003). "The Economic Impact of Hypertension". The Journal of Clinical Hypertension 5 (4): 3–13. doi:10.1111/j.1524-6175.2003.02463.x. PMID 12826765.
- ↑ Coca A (2008). "Economic benefits of treating high-risk hypertension with angiotensin II receptor antagonists (blockers)". Clinical Drug Investigation 28 (4): 211–20. doi:10.2165/00044011-200828040-00002. PMID 18345711.
- ↑ Roberts, J. M.; Pearson, G.; Cutler, J.; Lindheimer, M. (10 February 2003). "Summary of the NHLBI Working Group on Research on Hypertension During Pregnancy". Hypertension 41 (3): 437–445. doi:10.1161/01.HYP.0000054981.03589.E9. PMID 12623940.
- ↑ name=Gulati13>Gulati, V.; White, WB. (August 2013). "Review of the state of renal nerve ablation for patients with severe and resistant hypertension". J Am Soc Hypertens 7 (6): 484–93. doi:10.1016/j.jash.2013.07.003. PMID 23953998.
- ↑ Bhatt, Deepak L.; Kandzari, David E.; O'Neill, William W.; D'Agostino, Ralph; Flack, John M.; Katzen, Barry T.; Leon, Martin B.; Liu, Minglei; Mauri, Laura; Negoita, Manuela; Cohen, Sidney A.; Oparil, Suzanne; Rocha-Singh, Krishna; Townsend, Raymond R.; Bakris, George L. (2014). "A Controlled Trial of Renal Denervation for Resistant Hypertension". New England Journal of Medicine 370 (15): 1393–1401. doi:10.1056/NEJMoa1402670. ISSN 0028-4793.
- ↑ Gulati, V.; White, WB. (August 2013). "Review of the state of renal nerve ablation for patients with severe and resistant hypertension". J Am Soc Hypertens 7 (6): 484–93. doi:10.1016/j.jash.2013.07.003. PMID 23953998.
- ↑ Lobo, M. D.; de Belder, M. A.; Cleveland, T.; Collier, D.; Dasgupta, I.; Deanfield, J.; Kapil, V.; Knight, C.; Matson, M.; Moss, J.; Paton, J. F. R.; Poulter, N.; Simpson, I.; Williams, B.; Caulfield, M. J. (2014). "Joint UK societies' 2014 consensus statement on renal denervation for resistant hypertension". Heart 101 (1): 10–16. doi:10.1136/heartjnl-2014-307029. ISSN 1355-6037.
- ↑ Kaplan's Clinical Hypertension, 2010, page 51.
- ↑ Kaplan's Clinical Hypertension, 2015, p 45
- ↑ Schmieder, RE; Redon, J; Grassi, G; Kjeldsen, SE; Mancia, G; Narkiewicz, K; Parati, G; Ruilope, L; van de Borne, P; Tsioufis, C (May 2012). "ESH position paper: renal denervation - an interventional therapy of resistant hypertension.". Journal of hypertension 30 (5): 837–41. PMID 22469838.
Further reading
- James, Paul A.; Oparil, Suzanne; Carter, Barry L.; Cushman, William C.; Dennison-Himmelfarb, Cheryl; Handler, Joel; Lackland, Daniel T.; Lefevre, Michael L.; MacKenzie, Thomas D.; Ogedegbe, Olugbenga; Smith, Sidney C.; Svetkey, Laura P.; Taler, Sandra J.; Townsend, Raymond R.; Wright, Jackson T.; Narva, Andrew S.; Ortiz, Eduardo (18 December 2013). "2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults". JAMA 311 (5): 507–20. doi:10.1001/jama.2013.284427. PMID 24352797.
External links
| Wikimedia Commons has media related to Hypertension. |
- Hypertension at DMOZ
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||