Heroin
 | |
 | |
| Systematic (IUPAC) name | |
|---|---|
| (5α,6α)-7,8-didehydro-4,5-epoxy-17-methylmorphinan-3,6-diol diacetate | |
| Clinical data | |
| AHFS/Drugs.com | entry |
| |
|
Physical: Very high Psychological: Very high | |
| Very high | |
| Inhalation, transmucosal, intravenous, oral, intranasal, rectal, intramuscular | |
| Pharmacokinetic data | |
| Bioavailability | <35% (oral), 44–61% (inhaled)[1] |
| Protein binding | 0% (morphine metabolite 35%) |
| Metabolism | hepatic |
| Half-life | 2–3 minutes[2] |
| Excretion | 90% renal as glucuronides, rest biliary |
| Identifiers | |
|
561-27-3 | |
| N07BC06 | |
| PubChem | CID 5462328 |
| DrugBank |
DB01452 |
| ChemSpider |
4575379 |
| UNII |
8H672SHT8E |
| ChEBI |
CHEBI:27808 |
| ChEMBL |
CHEMBL459324 |
| Synonyms | Diamorphine, Diacetylmorphine, Acetomorphine, (Dual) Acetylated morphine, Morphine diacetate |
| Chemical data | |
| Formula | C21H23NO5 |
| 369.41 g/mol | |
|
SMILES
| |
| |
| | |
Heroin /ˈhɛroʊɪn/ (diacetylmorphine or morphine diacetate, also known as diamorphine (BAN, INN[3])) and commonly known by its street names of H, smack, boy, horse, brown, black, tar, and others[4] is an opioid analgesic originally synthesized by C.R. Alder Wright in 1874 by adding two acetyl groups to the molecule morphine, which is found naturally in the opium poppy. It is the 3,6-diacetyl ester of morphine. Administered intravenously by injection, heroin is two to four times more potent than morphine and is faster in its onset of action.[5]
Illicit heroin is sometimes available in freebase form, dulling the sheen and consistency to a matte-white powder.[6] Because of its lower boiling point, the freebase form of heroin is also smokable. It is prevalent in heroin coming from Afghanistan, which in 2004 produced roughly 87% of the world supply in illicit raw opium.[7] However, the production rate in Mexico has risen sixfold from 2007 to 2011, changing that percentage and placing Mexico as the second largest opium producer in the world.[8]
As with other opioids, diacetylmorphine is used as both a legal, medically prescribed drug (e.g., as an analgesic, cough suppressant and as an anti-diarrhea drug) and a recreational drug, in which case the user is seeking euphoria. Frequent and regular administration is associated with tolerance and physical dependence. Internationally, diacetylmorphine is controlled under Schedules I and IV of the Single Convention on Narcotic Drugs.[9] It is illegal to manufacture, possess, or sell diacetylmorphine without a license.
It is also available for prescription to long-term users as a form of opioid replacement therapy in the United Kingdom, Netherlands, Switzerland, Germany, and Denmark, alongside psycho-social care—in the same manner that methadone or buprenorphine are used in the United States and Canada—and a similar programme is being campaigned for by liberal political parties in Norway.[10]
Usage


The United Nations estimated in 2005 that there were over 50 million people worldwide who regularly used cocaine, heroin, and synthetic drugs.[12]
Medical use
Under the chemical name diamorphine, diacetylmorphine is prescribed as a strong analgesic in the United Kingdom, where it is given via subcutaneous, intramuscular, intrathecal or intravenous route. Its use includes treatment for acute pain, such as in severe physical trauma, myocardial infarction, post-surgical pain, and chronic pain, including end-stage cancer and other terminal illnesses. In other countries it is more common to use morphine or other strong opioids in these situations. In 2004, the National Institute for Health and Clinical Excellence, a non-departmental public body of the Department of Health in the United Kingdom, produced guidance on the management of caesarian section, which recommended the use of intrathecal or epidural diacetylmorphine for post-operative pain relief.[13]
In 2005, there was a shortage of diacetylmorphine in the UK, because of a problem at the main UK manufacturers.[14] Because of this, many hospitals changed to using morphine instead of diacetylmorphine. Although there is no longer a problem with the manufacturing of diacetylmorphine in the UK, some hospitals there have continued to use morphine. The majority, however, continue to use diacetylmorphine, and diacetylmorphine tablets are supplied for pain management.
Diacetylmorphine continues to be widely used in palliative care in the UK, where it is commonly given by the subcutaneous route, often via a syringe driver, if patients cannot easily swallow oral morphine solution. The advantage of diacetylmorphine over morphine is that diacetylmorphine is more fat soluble and therefore more potent by injection, so smaller doses of it are needed for the same analgesic effect. Both of these factors are advantageous if giving high doses of opioids via the subcutaneous route, which is often necessary in palliative care.
The medical use of diacetylmorphine, in common with other strong opioids such as morphine, fentanyl and oxycodone, is controlled in the UK by the Misuse of Drugs Act 1971. In the UK, it is a class A controlled drug and as such is subject to guidelines surrounding its storage, administration and destruction. Possession of diamorphine without a prescription is an arrestable offence. When diamorphine is prescribed in a hospital or similar environment, its administration must be supervised by two people who must then complete and sign a controlled drugs register (CD register) detailing the patient's name, amount, time, date and route of administration. In the case of a physician administering diamorphine, then he/she may administer the drug alone, however the rule requiring two registered practitioners, such as a nurse, midwife or another physician to sign the CD register still applies. The use of a witness when administering diamorphine is to avoid the possibility of the drug being diverted onto the black market.
For safety reasons, many UK National Health Service hospitals now only permit the administration of intravenous diamorphine in designated areas. In practice this usually means a critical care unit, an accident and emergency department, operating theatres by an anaesthetist or nurse anaesthetist or other such areas where close monitoring and support from senior staff is immediately available. However, administration by other routes is permitted in other areas of the hospital. This includes subcutaneous, intramuscular, intravenously as part of a patient controlled analgesia setup, and as an already established epidural infusion pump. Subcutaneous infusion, along with subcutaneous and intramuscular injection (bolus administration), is often used in the patient's own home, in order to treat severe pain in terminal illness.
Diacetylmorphine is also used as a maintenance drug to treat certain groups of addicts, normally long-term chronic intravenous (IV) heroin users, and even in these situations it is only prescribed following exhaustive efforts at treatment via other means. It is thought that heroin users can walk into a clinic and walk out with a prescription, but the process takes many weeks before a prescription for diacetylmorphine is issued. Though this is somewhat controversial among proponents of a zero-tolerance drug policy, it has proven superior to methadone in improving the social and health situation of addicts.[15] See: Heroin prescription for addicts
Recreational use
Diacetylmorphine, almost always still called by its original trade name of heroin in non-medical settings, is used as a recreational drug for the intense euphoria it induces. Anthropologist Michael Agar once described heroin as "the perfect whatever drug."[16] Tolerance develops quickly, and increased doses are needed in order to achieve the same effects. Its popularity with recreational drug users, compared to morphine, reportedly stems from its perceived different effects.[17] In particular, users report an intense rush, an acute transcendent state of euphoria, which occurs while diacetylmorphine is being metabolized into 6-monoacetylmorphine (6-MAM) and morphine in the brain. Some believe that heroin produces more euphoria than other opioids upon injection; one possible explanation is the presence of 6-monoacetylmorphine, a metabolite unique to heroin – although a more likely explanation is the rapidity of onset. While other opioids of recreational use produce only morphine, heroin also leaves 6-MAM, also a psycho-active metabolite. However, this perception is not supported by the results of clinical studies comparing the physiological and subjective effects of injected heroin and morphine in individuals formerly addicted to opioids; these subjects showed no preference for one drug over the other. Equipotent injected doses had comparable action courses, with no difference in subjects' self-rated feelings of euphoria, ambition, nervousness, relaxation, drowsiness, or sleepiness.[18]
Short-term addiction studies by the same researchers demonstrated that tolerance developed at a similar rate to both heroin and morphine. When compared to the opioids hydromorphone, fentanyl, oxycodone, and pethidine/meperidine, former addicts showed a strong preference for heroin and morphine, suggesting that heroin and morphine are particularly susceptible to abuse and addiction. Morphine and heroin were also much more likely to produce euphoria and other positive subjective effects when compared to these other opioids.[18]
Some researchers have attempted to explain heroin use and the culture that surrounds it through the use of sociological theories. In Righteous Dopefiend, Philippe Bourgois and Jeff Schonberg use anomie theory to explain why people begin using heroin. By analyzing a community in San Francisco, they demonstrated that heroin use was caused in part by internal and external factors such as violent homes and parental neglect. This lack of emotional, social, and financial support causes strain and influences individuals to engage in deviant acts, including heroin usage.[19] They further found that heroin users practiced "retreatism", a behavior first described by Howard Abadinsky, in which those suffering from such strain reject society's goals and institutionalized means of achieving them.[20]
Prescription for addicts
The UK Department of Health's Rolleston Committee Report[21] in 1926 established the British approach to diacetylmorphine prescription to users, which was maintained for the next 40 years: dealers were prosecuted, but doctors could prescribe diacetylmorphine to users when withdrawing from it would cause harm or severe distress to the patient. This "policing and prescribing" policy effectively controlled the perceived diacetylmorphine problem in the UK until 1959 when the number of diacetylmorphine addicts doubled every 16 months during a period of ten years, 1959–68.[22] In 1964, the Brain Committee recommended that only selected approved doctors working at approved specialised centres be allowed to prescribe diacetylmorphine and benzoylmethylecgonine (cocaine) to users. The law was made more restrictive in 1968. Beginning in the 1970s, the emphasis shifted to abstinence and the use of methadone; until now only a small number of users in the UK are prescribed diacetylmorphine.[23]
In 1994, Switzerland began a trial diamorphine maintenance program for users that had failed multiple withdrawal programs. The aim of this program was to maintain the health of the user by avoiding medical problems stemming from the illicit use of diacetylmorphine. The first trial in 1994 involved 340 users, although enrollment was later expanded to 1000 based on the apparent success of the program.
The trials proved diamorphine maintenance to be superior to other forms of treatment in improving the social and health situation for this group of patients.[24] It has also been shown to save money, despite high treatment expenses, as it significantly reduces costs incurred by trials, incarceration, health interventions and delinquency.[25] Patients appear twice daily at a treatment center, where they inject their dose of diamorphine under the supervision of medical staff. They are required to contribute about 450 Swiss francs per month to the treatment costs.[26] A national referendum in November 2008 showed 68% of voters supported the plan,[27] introducing diacetylmorphine prescription into federal law. The trials before were based on time-limited executive ordinances. The success of the Swiss trials led German, Dutch,[28] and Canadian[29] cities to try out their own diamorphine prescription programs.[30] Some Australian cities (such as Sydney) have instituted legal diacetylmorphine supervised injecting centers, in line with other wider harm minimization programs.
Since January 2009, Denmark has prescribed diamorphine to a few addicts that have tried methadone and subutex without success.[31] Beginning in February 2010, addicts in Copenhagen and Odense will be eligible to receive free diacetylmorphine. Later in 2010 other cities including Århus and Esbjerg will join the scheme. In total, around 230 addicts will be able to receive free diacetylmorphine.[32] However, Danish addicts will only be able to inject heroin according to the policy set by Danish National Board of Health.[33] Of the estimated 1500 drug users who do not benefit from the current oral substitution treatment, approximately 900 will not be in the target group for treatment with injectable diacetylmorphine, either because of "massive multiple drug abuse of non-opioids" or "not wanting treatment with injectable diacetylmorphine".[34]
In July 2009, the German Bundestag passed a law allowing diacetylmorphine prescription as a standard treatment for addicts; a large-scale trial of diacetylmorphine prescription had been authorized in that country in 2002.[35]
Detection in biological fluids
The major metabolites of diacetylmorphine, 6-MAM, morphine, morphine-3-glucuronide and morphine-6-glucuronide, may be quantitated in blood, plasma or urine to monitor for abuse, confirm a diagnosis of poisoning or assist in a medicolegal death investigation. Most commercial opiate screening tests cross-react appreciably with these metabolites, as well as with other biotransformation products likely to be present following usage of street-grade diacetylmorphine such as 6-acetylcodeine and codeine. However, chromatographic techniques can easily distinguish and measure each of these substances. When interpreting the results of a test, it is important to consider the diacetylmorphine usage history of the individual, since a chronic user can develop tolerance to doses that would incapacitate an opiate-naive individual, and the chronic user often has high baseline values of these metabolites in his system. Furthermore, some testing procedures employ a hydrolysis step before quantitation that converts many of the metabolic products to morphine, yielding a result that may be 2 times larger than with a method that examines each product individually.[36]
Adverse effects

Like most opioids, unadulterated heroin does not cause many long-term complications other than dependence and constipation.[37] The average purity of street heroin in the UK varies between 30% and 50% and heroin that has been seized at the border has purity levels between 40% and 60%; this variation has led to people suffering from overdoses as a result of the heroin missing a stage on its journey from port to end user, as each set of hands that the drug passes through adds further adulterants, the strength of the drug reduces, with the effect that if steps are missed, the purity of the drug reaching the end user is higher than they are used to.[38] Intravenous use of heroin (and any other substance) with non-sterile needles and syringes or other related equipment may lead to:
- The risk of contracting blood-borne pathogens such as HIV and hepatitis by the sharing of needles
- The risk of contracting bacterial or fungal endocarditis and possibly venous sclerosis
- Abscesses
- Poisoning from contaminants added to "cut" or dilute heroin
- Decreased kidney function (although it is not currently known if this is because of adulterants or infectious diseases)[39]
Many countries and local governments have begun funding programs that supply sterile needles to people who inject illegal drugs in an attempt to reduce these contingent risks, and especially the spread of blood-borne diseases. The Drug Policy Alliance reports that up to 75% of new AIDS cases among women and children are directly or indirectly a consequence of drug use by injection. The United States federal government does not operate needle exchanges, although some state and local governments do support such programs.
Anthropologists Philippe Bourgois and Jeff Schonberg performed a decade of fieldwork among homeless heroin and cocaine addicts in San Francisco, published in 2009. They reported that the African-American addicts they observed were more inclined to "direct deposit" heroin into a vein, while "skin-popping" was a far more widespread practice: "By the midpoint of our fieldwork, most of the whites had given up searching for operable veins and skin-popped. They sank their needles perfunctorily, often through their clothing, into their fatty tissue." Bourgois and Schonberg describes how the cultural difference between the African-Americans and the whites leads to this contrasting behavior, and also points out that the two different ways to inject heroin comes with different health risks. Skin-popping more often results in abscesses, and direct injection more often leads to fatal overdose and also to hepatitis C and HIV infection.[19]
Heroin overdose is usually treated with an opioid antagonist, such as naloxone (Narcan), or naltrexone, which has high affinity for opioid receptors but does not activate them. This reverses the effects of heroin and other opioid agonists and causes an immediate return of consciousness but may precipitate withdrawal symptoms. The half-life of naloxone is much shorter than that of most opioid agonists, so that antagonist typically has to be administered multiple times until the opioid has been metabolized by the body.
Depending on drug interactions and numerous other factors, death from overdose can take anywhere from several minutes to several hours because of anoxia resulting from the breathing reflex being suppressed by agonism of µ-opioid receptors. An overdose is immediately reversible with an opioid antagonist injection. Heroin overdoses can occur because of an unexpected increase in the dose or purity or because of diminished opioid tolerance. However, many fatalities reported as overdoses are probably caused by interactions with other depressant drugs such as alcohol or benzodiazepines.[40] It should also be noted that since heroin can cause nausea and vomiting, a significant number of deaths attributed to heroin overdose are caused by aspiration of vomit by an unconscious victim. Some sources quote the median lethal dose (for an average 75 kg opiate-naive individual) as being between 75 and 600 mg.[41][42] Experiments on simians have demonstrated therapeutic indexes up to 50.[43] Illicit heroin is of widely varying and unpredictable purity. This means that the user may prepare what they consider to be a moderate dose while actually taking far more than intended. Also, tolerance typically decreases after a period of abstinence. If this occurs and the user takes a dose comparable to their previous use, the user may experience drug effects that are much greater than expected, potentially resulting in a dangerous overdose. It has been speculated that an unknown portion of heroin-related deaths are the result of an overdose or allergic reaction to quinine, which may sometimes be used as a cutting agent.[44]
A final factor contributing to overdoses is environment-conditioned tolerance, in which the body associates the environment in which the drug is used with the drug itself. While the mechanism is not yet clearly understood, long-term heroin users display increased tolerance to the drug in locations where they have repeatedly administered it. When the drug is used in a different location, this environment-conditioned tolerance does not occur, resulting in a greater drug effect. Thus, a dose administered in an unfamiliar environment may be too high and potentially fatal. This tendency toward conditioning is exacerbated by the fact that heroin use is a highly ritualized behavior, which means that there are many cues for conditioning.[45]
A small percentage of heroin smokers, and occasionally IV users, may develop symptoms of toxic leukoencephalopathy. The cause has yet to be identified, but one speculation is that the disorder is caused by an uncommon adulterant that is only active when heated.[46][47][48] Symptoms include slurred speech and difficulty walking.
Cocaine is sometimes used in combination with heroin, and is referred to as a speedball when injected or moonrocks when smoked together. Cocaine acts as a stimulant, whereas heroin acts as a depressant. Coadministration provides an intense rush of euphoria with a high that combines both effects of the drugs, while excluding the negative effects, such as anxiety and sedation. The effects of cocaine wear off far more quickly than heroin, so if an overdose of heroin was used to compensate for cocaine, the end result is fatal respiratory depression.
-
Preparing heroin for injection
-

Modified syringe for suppository administration
-

One stamp of heroin
-

Chunky "No.3" heroin
Withdrawal
The withdrawal syndrome from heroin (the so-called "cold turkey") may begin within 6 to 24 hours of discontinuation of the drug; however, this time frame can fluctuate with the degree of tolerance as well as the amount of the last consumed dose. Symptoms may include:[49] sweating, malaise, anxiety, depression, akathisia, priapism, extra sensitivity of the genitals in females, general feeling of heaviness, excessive yawning or sneezing, tears, rhinorrhea, sleep difficulties (insomnia), cold sweats, chills, severe muscle and bone aches, nausea, vomiting, diarrhea, cramps, watery eyes,[50] fever and cramp-like pains and involuntary spasms in the limbs (thought to be an origin of the term "kicking the habit"[51]).
Pharmacology
When taken orally, heroin undergoes extensive first-pass metabolism via deacetylation, making it a prodrug for the systemic delivery of morphine.[5] When the drug is injected, however, it avoids this first-pass effect, very rapidly crossing the blood–brain barrier because of the presence of the acetyl groups, which render it much more fat soluble than morphine itself.[52] Once in the brain, it then is deacetylated variously into the inactive 3-monoacetylmorphine and the active 6-monoacetylmorphine (6-MAM), and then to morphine, which bind to μ-opioid receptors, resulting in the drug's euphoric, analgesic (pain relief), and anxiolytic (anti-anxiety) effects; heroin itself exhibits relatively low affinity for the μ receptor.[53] Unlike hydromorphone and oxymorphone, however, administered intravenously, heroin creates a larger histamine release, similar to morphine, resulting in the feeling of a greater subjective "body high" to some, but also instances of pruritus (itching) when they first start using.[54]
Both morphine and 6-MAM are μ-opioid agonists that bind to receptors present throughout the brain, spinal cord, and gut of all mammals. The μ-opioid receptor also binds endogenous opioid peptides such as β-endorphin, Leu-enkephalin, and Met-enkephalin. Repeated use of heroin results in a number of physiological changes, including an increase in the production of μ-opioid receptors (upregulation). These physiological alterations lead to tolerance and dependence, so that cessation of heroin use results in a set of remarkably uncomfortable symptoms including pain, anxiety, muscle spasms, and insomnia called the opioid withdrawal syndrome. Depending on usage it has an onset four to 24 hours after the last dose of heroin. Morphine also binds to δ- and κ-opioid receptors.
There is also evidence that 6-MAM binds to a subtype of μ-opioid receptors that are also activated by the morphine metabolite morphine-6β-glucuronide but not morphine itself.[55] The third subtype of third opioid type is the mu-3 receptor, which may be a commonality to other six-position monoesters of morphine. The contribution of these receptors to the overall pharmacology of heroin remains unknown.
A subclass of morphine derivatives, namely the 3,6 esters of morphine, with similar effects and uses, includes the clinically used strong analgesics nicomorphine (Vilan), and dipropanoylmorphine; there is also the latter's dihydromorphine analogue, diacetyldihydromorphine (Paralaudin). Two other 3,6 diesters of morphine invented in 1874–75 along with diacetylmorphine, dibenzoylmorphine and acetylpropionylmorphine, were made as substitutes after it was outlawed in 1925 and, therefore, sold as the first "designer drugs" until they were outlawed by the League of Nations in 1930.
Etymology
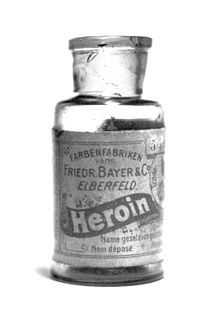
In 1895, the German drug company Bayer marketed diacetylmorphine as an over-the-counter drug under the trademark name Heroin.[56] The name was derived from the Greek word heros because of its perceived "heroic" effects upon a user.[56] It was developed chiefly as a morphine substitute for cough suppressants that did not have morphine's addictive side-effects. Morphine at the time was a popular recreational drug, and Bayer wished to find a similar but non-addictive substitute to market. However, contrary to Bayer's advertising as a "non-addictive morphine substitute," heroin would soon have one of the highest rates of dependence among its users.[57]
History
The opium poppy was cultivated in lower Mesopotamia as long ago as 3400 BCE.[58] The chemical analysis of opium in the 19th century revealed that most of its activity could be ascribed to two alkaloids, codeine and morphine.
Diacetylmorphine was first synthesized in 1874 by C. R. Alder Wright, an English chemist working at St. Mary's Hospital Medical School in London. He had been experimenting with combining morphine with various acids. He boiled anhydrous morphine alkaloid with acetic anhydride for several hours and produced a more potent, acetylated form of morphine, now called diacetylmorphine or morphine diacetate. The compound was sent to F. M. Pierce of Owens College in Manchester for analysis. Pierce told Wright:
Doses ... were subcutaneously injected into young dogs and rabbits ... with the following general results ... great prostration, fear, and sleepiness speedily following the administration, the eyes being sensitive, and pupils constrict, considerable salivation being produced in dogs, and slight tendency to vomiting in some cases, but no actual emesis. Respiration was at first quickened, but subsequently reduced, and the heart's action was diminished, and rendered irregular. Marked want of coordinating power over the muscular movements, and loss of power in the pelvis and hind limbs, together with a diminution of temperature in the rectum of about 4°.[59]

Wright's invention did not lead to any further developments, and diacetylmorphine became popular only after it was independently re-synthesized 23 years later by another chemist, Felix Hoffmann.[60] Hoffmann, working at Bayer pharmaceutical company in Elberfeld, Germany, was instructed by his supervisor Heinrich Dreser to acetylate morphine with the objective of producing codeine, a constituent of the opium poppy, pharmacologically similar to morphine but less potent and less addictive. Instead, the experiment produced an acetylated form of morphine one and a half to two times more potent than morphine itself. The head of Bayer's research department reputedly coined the drug's new name, "heroin," based on the German heroisch, which means "heroic, strong.'Bayer scientists were not the first to make heroin, but their scientists discovered ways to make it, and Bayer led commercialization of heroin.[61]
From 1898 through to 1910, diacetylmorphine was marketed under the trademark name Heroin as a non-addictive morphine substitute and cough suppressant.[62]
In the U.S.A., the Harrison Narcotics Tax Act was passed in 1914 to control the sale and distribution of diacetylmorphine and other opioids, which allowed the drug to be prescribed and sold for medical purposes. In 1924, the United States Congress banned its sale, importation, or manufacture. It is now a Schedule I substance, which makes it illegal for non-medical use in signatory nations of the Single Convention on Narcotic Drugs treaty, including the United States.
The Health Committee of the League of Nations banned diacetylmorphine in 1925, although it took more than three years for this to be implemented. In the meantime, the first designer drugs, viz. 3,6 diesters and 6 monoesters of morphine and acetylated analogues of closely related drugs like hydromorphone and dihydromorphine, were produced in massive quantities to fill the worldwide demand for diacetylmorphine—this continued until 1930 when the Committee banned diacetylmorphine analogues with no therapeutic advantage over drugs already in use, the first major legislation of this type.
Later, as with Aspirin, Bayer lost some of its trademark rights to heroin under the 1919 Treaty of Versailles following the German defeat in World War I.[63]
Routes of administration
Recreational uses:
Medicinal uses:
|
Contraindications:
|
Central nervous system:
Neurological:
Psychological:
Cardiovascular & Respiratory: Gastrointestinal:
Musculoskeletal:
Skin:
Miscellaneous:
Diamorphine ampoules for medicinal use |
The onset of heroin's effects depends upon the route of administration. Studies have shown that the subjective pleasure of drug use (the reinforcing component of addiction) is proportional to the rate at which the blood level of the drug increases.[64] Intravenous injection is the fastest route of drug administration, causing blood concentrations to rise the most quickly, followed by smoking, suppository (anal or vaginal insertion), insufflation (snorting), and ingestion (swallowing).
Ingestion does not produce a rush as forerunner to the high experienced with the use of heroin, which is most pronounced with intravenous use. While the onset of the rush induced by injection can occur in as little as a few seconds, the oral route of administration requires approximately half an hour before the high sets in. Thus, with both higher the dosage of heroin used and faster the route of administration used, the higher potential risk for psychological addiction.
Large doses of heroin can cause fatal respiratory depression, and the drug has been used for suicide or as a murder weapon. The serial killer Dr Harold Shipman used diamorphine on his victims, and the subsequent Shipman Inquiry led to a tightening of the regulations surrounding the storage, prescribing and destruction of controlled drugs in the UK. Dr John Bodkin Adams (see his victim Edith Alice Morrell) is also known to have used heroin as a murder weapon.
Because significant tolerance to respiratory depression develops quickly with continued use and is lost just as quickly during withdrawal, it is often difficult to determine whether a heroin lethal overdose was accidental, suicide or homicide. Examples include the overdose deaths of Sid Vicious, Janis Joplin, Tim Buckley, Hillel Slovak, Layne Staley, Bradley Nowell, Ted Binion, and River Phoenix.[65]
Chronic use of heroin and other opioids has been shown to be a potential cause of hyponatremia, resultant because of excess vasopressin secretion.
Oral
Oral use of heroin is less common than other methods of administration, mainly because there is little to no "rush", and the effects are less potent.[66] Heroin is entirely converted to morphine by means of first-pass metabolism, resulting in deacetylation when ingested. Heroin's oral bioavailability is both dose-dependent (as is morphine's) and significantly higher than oral use of morphine itself, reaching up to 64.2% for high doses and 45.6% for low doses; opiate-naive users showed far less absorption of the drug at low doses, having bioavailabilities of only up to 22.9%. The maximum plasma concentration of morphine following oral administration of heroin was around twice as much as that of oral morphine.[67]
Injection
Injection, also known as "slamming", "banging", "shooting up", "digging" or "mainlining", is a popular method which carries relatively greater risks than other methods of administration. Heroin base (commonly found in Europe), when prepared for injection, will only dissolve in water when mixed with an acid (most commonly citric acid powder or lemon juice) and heated. Heroin in the east-coast United States is most commonly found in the hydrochloride salt form, requiring just water (and no heat) to dissolve. Users tend to initially inject in the easily accessible arm veins, but as these veins collapse over time, users resort to more dangerous areas of the body, such as the femoral vein in the groin. Users who have used this route of administration often develop a deep vein thrombosis. Intravenous users can use a various single dose range using a hypodermic needle. The dose of heroin used for recreational purposes is dependent on the frequency and level of use: thus a first-time user may use between 5 and 20 mg, while an established addict may require several hundred mg per day. As with the injection of any drug, if a group of users share a common needle without sterilization procedures, blood-borne diseases, such as HIV or hepatitis, can be transmitted. The use of a common dispenser for water for the use in the preparation of the injection, as well as the sharing of spoons and/or filters can also cause the spread of blood-borne diseases. Many countries now supply small sterile spoons and filters for single use in order to prevent the spread of disease.[68]
Smoking
Smoking heroin refers to vaporizing it to inhale the resulting fumes, not burning it to inhale the resulting smoke. It is commonly smoked in glass pipes made from glassblown Pyrex tubes and light bulbs. It can also be smoked off aluminium foil, which is heated underneath by a flame and the resulting smoke is inhaled through a tube of rolled up foil, This method is also known as "chasing the dragon" (whereas smoking methamphetamine is known as "chasing the white dragon").
Insufflation
Another popular route to intake heroin is insufflation (snorting), where a user crushes the heroin into a fine powder and then gently inhales it (sometimes with a straw or a rolled-up banknote, as with cocaine) into the nose, where heroin is absorbed through the soft tissue in the mucous membrane of the sinus cavity and straight into the bloodstream. This method of administration redirects first-pass metabolism, with a quicker onset and higher bioavailability than oral administration, though the duration of action is shortened. This method is sometimes preferred by users who do not want to prepare and administer heroin for injection or smoking, but still experience a fast onset. Snorting heroin becomes an often unwanted route, once a user begins to inject the drug. The user may still get high on the drug from snorting, and experience a nod, but will not get a rush. A "rush" is caused by a large amount of heroin entering the body at once. When the drug is taken in through the nose, the user does not get the rush because the drug is absorbed slowly rather than instantly.
Suppository
Little research has been focused on the suppository (anal insertion) or pessary (vaginal insertion) methods of administration, also known as "plugging". These methods of administration are commonly carried out using an oral syringe. Heroin can be dissolved and withdrawn into an oral syringe which may then be lubricated and inserted into the anus or vagina before the plunger is pushed. The rectum or the vaginal canal is where the majority of the drug would likely be taken up, through the membranes lining their walls.
Regulation
Asia
In Hong Kong, diacetylmorphine is regulated under Schedule 1 of Hong Kong's Chapter 134 Dangerous Drugs Ordinance. It is available by prescription. Anyone supplying diacetylmorphine without a valid prescription can be fined $10,000 (HKD). The penalty for trafficking or manufacturing diacetylmorphine is a $50,000 (HKD) fine and life imprisonment. Possession of diacetylmorphine without a license from the Department of Health is illegal with a $10,000 (HKD) fine and/or 7 years of jail time.[69]
Europe
In the Netherlands, diacetylmorphine is a List I drug of the Opium Law. It is available for prescription under tight regulation exclusively to long-term addicts for whom methadone maintenance treatment has failed. It cannot be used to treat severe pain or other illnesses.[70]
In the United Kingdom, diacetylmorphine is available by prescription, though it is a restricted Class A drug. According to the 50th edition of the British National Formulary (BNF), diamorphine hydrochloride may be used in the treatment of acute pain, myocardial infarction, acute pulmonary oedema, and chronic pain. The treatment of chronic non-malignant pain must be supervised by a specialist. The BNF notes that all opioid analgesics cause dependence and tolerance but that this is "no deterrent in the control of pain in terminal illness". When used in the palliative care of cancer patients, diacetylmorphine is often injected using a syringe driver.[71]
North America
In Canada, diacetylmorphine is a controlled substance[72] under Schedule I of the Controlled Drugs and Substances Act (CDSA).[73] Any person seeking or obtaining diacetylmorphine without disclosing authorization 30 days before obtaining another prescription from a practitioner is guilty of an indictable offense and subject to imprisonment for a term not exceeding seven years. Possession of diacetylmorphine for the purpose of trafficking is an indictable offense and subject to imprisonment for life.
In the United States, diacetylmorphine is a Schedule I drug according to the Controlled Substances Act of 1970, making it illegal to possess without a DEA license.[74] Possession of more than 100 grams of diacetylmorphine or a mixture containing diacetylmorphine is punishable with a minimum mandatory sentence of 5 years of imprisonment in a federal prison.
Production and trafficking
Production
Diacetylmorphine is produced from acetylation of morphine derived from natural opium sources. Numerous mechanical and chemical means are used to purify the final product. The final products have a different appearance depending on purity and have different names.[75]
Heroin grades
Heroin purity has been classified into four grades. No.4 is the purest form – white powder (salt) to be easily dissolved and injected. No.3 is "brown sugar" for smoking (base). No.1 and No.2 are unprocessed raw heroin (salt or base).[76]
Trafficking
Traffic is heavy worldwide, with the biggest producer being Afghanistan.[77] According to a U.N. sponsored survey,[7] in 2004, Afghanistan accounted for production of 87 percent of the world's diacetylmorphine.[78] Afghan opium kills around 100,000 people annually.[79]
The cultivation of opium in Afghanistan reached its peak in 1999, when 350 square miles (910 km2) of poppies were sown. The following year the Taliban banned poppy cultivation, a move which cut production by 94 percent. By 2001 only 30 square miles (78 km2) of land were in use for growing opium poppies. A year later, after American and British troops had removed the Taliban and installed the interim government, the land under cultivation leapt back to 285 square miles (740 km2), with Afghanistan supplanting Burma to become the world's largest opium producer once more.[80][81] Opium production in that country has increased rapidly since, reaching an all-time high in 2006. War in Afghanistan once again appeared as a facilitator of the trade.[82] Some 3.3 million Afghans are involved in producing opium.[83]
At present, opium poppies are mostly grown in Afghanistan, and in Southeast Asia, especially in the region known as the Golden Triangle straddling Burma, Thailand, Vietnam, Laos and Yunnan province in China. There is also cultivation of opium poppies in the Sinaloa region of Mexico and in Colombia. The majority of the heroin consumed in the United States comes from Mexico and Colombia. According to the United Nations Office on Drugs and Crime (UNODC), Pakistan has over 1,000 hectares (2,500 acres) of opium poppies under cultivation concentrated in the areas bordering Afghanistan and is the destination and transit point for 40 percent of the opiates produced in that country.[84]
Conviction for trafficking heroin carries the death penalty in most Southeast Asian, some East Asian and Middle Eastern countries (see Use of death penalty worldwide for details), among which Malaysia, Singapore and Thailand are the most strict. The penalty applies even to citizens of countries where the penalty is not in place, sometimes causing controversy when foreign visitors are arrested for trafficking, for example the arrest of nine Australians in Bali, the death sentence given to Nola Blake in Thailand in 1987, or the hanging of an Australian citizen Van Tuong Nguyen in Singapore.
Trafficking history

The origins of the present international illegal heroin trade can be traced back to laws passed in many countries in the early 1900s that closely regulated the production and sale of opium and its derivatives including heroin. At first, heroin flowed from countries where it was still legal into countries where it was no longer legal. By the mid-1920s, heroin production had been made illegal in many parts of the world. An illegal trade developed at that time between heroin labs in China (mostly in Shanghai and Tianjin) and other nations. The weakness of government in China and conditions of civil war enabled heroin production to take root there. Chinese triad gangs eventually came to play a major role in the illicit heroin trade. The French Connection route started in the 1930s.
Heroin trafficking was virtually eliminated in the U.S. during World War II because of temporary trade disruptions caused by the war. Japan's war with China had cut the normal distribution routes for heroin and the war had generally disrupted the movement of opium.
After World War II, the Mafia took advantage of the weakness of the postwar Italian government and set up heroin labs in Sicily. The Mafia took advantage of Sicily's location along the historic route opium took westward into Europe and the United States.[85]
Large-scale international heroin production effectively ended in China with the victory of the communists in the civil war in the late 1940s. The elimination of Chinese production happened at the same time that Sicily's role in the trade developed.
Although it remained legal in some countries until after World War II, health risks, addiction, and widespread recreational use led most western countries to declare heroin a controlled substance by the latter half of the 20th century.
In late 1960s and early 1970s, the CIA supported anti-Communist Chinese Nationalists settled near the Sino-Burmese border and Hmong tribesmen in Laos. This helped the development of the Golden Triangle opium production region, which supplied about one-third of heroin consumed in US after the 1973 American withdrawal from Vietnam. In 1999, Burma, the heartland of the Golden Triangle, was the second largest producer of heroin, after Afghanistan.[86]
The Soviet-Afghan war led to increased production in the Pakistani-Afghan border regions, as U.S.-backed mujaheddin militants raised money for arms from selling opium, contributing heavily to the modern Golden Crescent creation. By 1980, 60 percent of heroin sold in the U.S. originated in Afghanistan.[86] It increased international production of heroin at lower prices in the 1980s. The trade shifted away from Sicily in the late 1970s as various criminal organizations violently fought with each other over the trade. The fighting also led to a stepped-up government law enforcement presence in Sicily. Following the discovery at a Jordanian airport of a toner cartridge that had been modified into an improvised explosive device, the resultant increased level of airfreight scrutiny led to a major shortage (drought) of heroin from October 2010 until April 2011. This was reported in most of mainland Europe and the UK which led to a price increase of approximately 30 percent in the cost of street heroin and an increased demand for diverted methadone. The number of addicts seeking treatment also increased significantly during this period. Other heroin droughts (shortages) have been attributed to cartels restricting supply in order to force a price increase and also to a fungus that attacked the opium crop of 2009. Many people thought that the American government had introduced pathogens into the Afghanistan atmosphere in order to destroy the opium crop and thus starve insurgents of income.
On 13 March 2012, Haji Bagcho, with ties to the Taliban, was convicted by a U.S. District Court of conspiracy, distribution of heroin for importation into the United States and narco-terrorism.[87][88][89][90][91][91] Based on heroin production statistics[92] compiled by the United Nations Office on Drugs and Crime, in 2006, Bagcho's activities accounted for approximately 20 percent of the world's total production for that year.[88][89][90][91]
Street price
The European Monitoring Centre for Drugs and Drug Addiction reports that the retail price of brown heroin varies from €14.5 per gram in Turkey to €110 per gram in Sweden, with most European countries reporting typical prices of €35–40 per gram. The price of white heroin is reported only by a few European countries and ranged between €27 and €110 per gram.[93]
The United Nations Office on Drugs and Crime claims in its 2008 World Drug Report that typical US retail prices are US$172 per gram.[94]
Harm reduction
.svg.png)
Harm reduction is a public health philosophy that seeks to reduce the harms associated with the use of diacetylmorphine. One aspect of harm reduction initiatives focuses on the behaviour of individual users. This includes promoting safer means of taking the drug, such as smoking, nasal use, oral or rectal insertion. This attempts to avoid the higher risks of overdose, infections and blood-borne viruses associated with injecting the drug. Other measures include using a small amount of the drug first to gauge the strength, and minimize the risks of overdose. For the same reason, poly drug use (the use of two or more drugs at the same time) is discouraged. Injecting diacetylmorphine users are encouraged to use new needles, syringes, spoons/steri-cups and filters every time they inject and not share these with other users. Users are also encouraged to not use it on their own, as others can assist in the event of an overdose.
Governments that support a harm reduction approach usually fund needle and syringe exchange programs, which supply new needles and syringes on a confidential basis, as well as education on proper filtering before injection, safer injection techniques, safe disposal of used injecting gear and other equipment used when preparing diacetylmorphine for injection may also be supplied including citric acid sachets/vitamin C sachets, steri-cups, filters, alcohol pre-injection swabs, sterile water ampules and tourniquets (to stop use of shoe laces or belts).
Another harm reduction measure employed for example in Europe, Canada and Australia are safe injection sites where users can inject diacetylmorphine and cocaine under the supervision of medically trained staff. Safe injection sites are low threshold and allow social services to approach problem users that would otherwise be hard to reach.[96] In the UK the Criminal Justice System has a protocol in place that requires that any individual that is arrested and is suspected of having a substance misuse problem be offered the chance to enter a treatment program. This has had the effect of drastically reducing an area's crime rate as individuals arrested for theft in order to supply the funds for their drugs are no longer in the position of having to steal to purchase heroin because they have been placed onto a methadone program, quite often more quickly than would have been possible had they not been arrested. This aspect of harm reduction is seen as being beneficial to both the individual and the community at large, who are then protected from the possible theft of their goods.[97][98]
During the late 1980s and early 1990s, Swiss authorities ran the ZIPP-AIDS (Zurich Intervention Pilot Project), handing out free syringes in the officially tolerated drug scene in Platzspitz park.
Popular culture
Heroin is mentioned in hundreds of films. Sometimes the use or trafficking of the drug is the central theme of the film but many times it is almost incidental as part of a crime in a police drama, for example.
- The 1959 play The Connection by Jack Gelber, and the 1961 film adaptation of it, concern a group of addicts, some of whom are jazz musicians, waiting for their dealer.
- The film The Panic in Needle Park starring Al Pacino and Kitty Winn is the story of a young woman who falls in love with a heroin addict in New York. It was one of Pacino's first roles.
- The film American Gangster is loosely based on real-life drug dealer Frank Lucas, who sold heroin. Lucas was portrayed by Denzel Washington.[99]
- The film Gia, based on a true story of model Gia Carangi, is about her addiction to and use of heroin and how it affected her.[100]
- The film Christiane F. – Wir Kinder vom Bahnhof Zoo (We the children of Bahnhof Zoo) is about heroin use and street culture in West Berlin in the 1970s, centering on a 13-year-old girl's decision to experiment with the drug.
- The film Trainspotting chronicles the exploits of a group of heroin addicts in Edinburgh, Scotland, during the late 1980s.
- The film Requiem for a Dream tells the story of four drug (mainly heroin) addicts who can only witness their disastrous habits spiral out of control into the darkest, ugliest and dirtiest sides of humanity.[101]
- In season three of the American television series 24, the show's protagonist Jack Bauer is seen battling a heroin addiction after having spent months undercover working with a drug lord family in Mexico.
- The film The Basketball Diaries follows protagonist Jim Carrol's addiction to heroin and getting off heroin. Leonardo Dicaprio portrayed Carroll.
- The film Pulp Fiction, featuring John Travolta as Vincent Vega, shows IV use of the drug, and Uma Thurman's character Mia Wallace overdoses.
- The television series Breaking Bad features Jane Margolis, Jesse Pinkman's girlfriend/landlady, who is in rehab for heroin usage, but gets back into using it and introduces Jesse to it, but later dies due to the combination of an overdose and Walter White's refusal to save her life.
- The film Rush (1991) starring Jennifer Jason Leigh, Jason Patric, Sam Elliott and Gregg Allman is a fictionalized depiction of a heroin-trade-based corruption scandal that wracked the Tyler, Texas, US Police Department in the late seventies; undercover detective characters played by Leigh and Patric inadvertently become heroin addicts in the process of attempting to gather evidence against the local drug dealer played by Allman.
Use of heroin by jazz musicians in particular was prevalent in the mid-twentieth century, including Billie Holiday, sax legends Charlie Parker and Art Pepper, guitarist Joe Pass and piano player/singer Ray Charles; a "staggering number of jazz musicians were addicts".[102] It was also a problem with many rock musicians, particularly from the late 1960s through the 1990s. Pete Doherty is also a self-confessed user of heroin.[103] Nirvana frontman Kurt Cobain's heroin addiction was well documented.[104] Pantera frontman, Phil Anselmo, turned to heroin while touring during the 1990s to cope with his back pain.[105]
Songs
- "The Needle and the Spoon" by Lynyrd Skynyrd off their album Second Helping.
- "Heroin" and "I'm Waiting For The Man" by The Velvet Underground
- "The Needle and the Damage Done" by Neil Young
- "Golden Brown" by The Stranglers
- "Beetlebum" by Blur
- "She Talks to Angels" by The Black Crowes
- "Heroin Girl" by Everclear
- "She's Like Heroin" System Of A Down
- "Under the Bridge" by Red Hot Chili Peppers
- "The Needle Lies Again" from the The Deadlight Sessions EP by Heaven Below
- "King Heroin" by James Brown
- "Hurt" by Nine Inch Nails
- "Badfish" by Sublime
- "The Needle Lies" by Queensryche
- "Needle in the Hay" by Elliott Smith
- "Time to Pretend" by MGMT
- "The A Team" by Ed Sheeran
- "There She Goes" by The La's
- "Brown Sugar" and "Dead Flowers by The Rolling Stones
- The Heroin Diaries Soundtrack, the debut studio album of Sixx:A.M.
- "Mr Brownstone" by Guns N' Roses[106]
- "Cold Turkey" by John Lennon was about Lennon and Yoko Ono going cold turkey off of their heroin addictions.[107]
- "Space Oddity", David Bowie's first single, was seemingly about his experience with heroin, as his 1980 single "Ashes to Ashes" included lines that refer to Major Tom as "...a junkie/strung out on heaven's high/hitting an all-time low."[108]
- Two songs on the U2 album Rattle and Hum refer to heroin use:
- "Desire" uses heroin as a metaphor for lust, with the lyrics "She's the candle burnin' in my room/ Yeah, I'm like the needle/ The needle and spoon"
- "Hawkmoon 269", a song about the passionate need for one's lover, includes the lyric "Like a needle needs a vein"
- U2 songs "Daddy's Gonna Pay for Your Crashed Car" and "Bad" also refer to heroin.
- Songs such as "Junkhead", "Godsmack", "Dirt" "Hate to Feel" and "Angry Chair" from the album Dirt, including many others from other albums, by grunge band Alice in Chains.[109]
- "People Who Died" by The Jim Carroll Band. Several people in the song died of heroin-related causes.[110]
- "(He'll Never Be An) Ol' Man River", a satirical song by the Australian band TISM lists a number of celebrities whose deaths were related to heroin use, including the song's namesake River Phoenix.
See also
- Allegations of CIA drug trafficking
- First and Second Opium Wars
- History of opium in China
- The Politics of Heroin in Southeast Asia
- Cheese (recreational drug)
References
- ↑ Rook EJ, van Ree JM, van den Brink W, Hillebrand MJ, Huitema AD, Hendriks VM, Beijnen JH (2006). "Pharmacokinetics and pharmacodynamics of high doses of pharmaceutically prepared heroin, by intravenous or by inhalation route in opioid-dependent patients". Basic Clin. Pharmacol. Toxicol. 98 (1): 86–96. doi:10.1111/j.1742-7843.2006.pto_233.x. PMID 16433897.
- ↑ "Diamorphine Hydrochloride Injection 30 mg – Summary of Product Characteristics". electronic Medicines Compendium. ViroPharma Limited. 24 September 2013. Retrieved 30 March 2014.
- ↑ Rang HP, Dale MM, Flower RJ, Henderson G (2011). Rang & Dale's pharmacology (7th ed.). Edinburgh, UK: Churchill Livingstone. ISBN 978-0-70-203471-8.
- ↑ "Nicknames and Street Names for Heroin". Thecyn.com. Retrieved 12 October 2013.
- ↑ 5.0 5.1 Sawynok J (January 1986). "The therapeutic use of heroin: a review of the pharmacological literature". Can. J. Physiol. Pharmacol. 64 (1): 1–6. doi:10.1139/y86-001. PMID 2420426.
- ↑ "Basic Facts About Heroin". Alcoholism.about.com. Retrieved 20 October 2010.
- ↑ 7.0 7.1 "Afghanistan opium survey – 2004" (PDF). United Nations Office on Drugs and Crime. Retrieved 22 October 2006.
- ↑ BBC News, Latin American & Caribbean: "Mexico targets heroine (sic) poppy plantations." Eric Camara 16 November 2011
- ↑ "Yellow List: List of Narcotic Drugs Under International Control" (PDF). International Narcotics Control Board. December 2004. Archived from the original (PDF) on 10 May 2012. Retrieved 5 May 2006. Referring URL = http://www.incb.org/incb/yellow_list.html''
- ↑ Uchtenhagen AA (March 2011). "Heroin maintenance treatment: from idea to research to practice.". Drug and Alcohol Review 30 (2): 130–7. doi:10.1111/j.1465-3362.2010.00266.x. PMID 21375613.
- ↑ 11.0 11.1 "Office of National Drug Control Policy (ONDCP): Heroin Facts & Figures". Whitehousedrugpolicy.gov. Retrieved 20 July 2012.
- ↑ "World | Drugs Trade". BBC News. Retrieved 20 July 2012.
- ↑ "NICE Clinical Guideline 13: Caesarian section" (PDF). p. 20. Retrieved 20 July 2012.
- ↑ "Diamorphine shortage: UKHRA statement on the UK diamorphine shortage". Ukhra.org. 14 September 2005. Retrieved 20 October 2010.
- ↑ Haasen C, Verthein U, Degkwitz P, Berger J, Krausz M, Naber D (2007). "Heroin-assisted treatment for opioid dependence: Randomised controlled trial". The British Journal of Psychiatry 191: 55–62. doi:10.1192/bjp.bp.106.026112. PMID 17602126.
- ↑ Agar, Michael (2007). Dope Double Agent: The Naked Emperor on Drugs. Lulu.com. ISBN 1-4116-8103-7. Retrieved 22 October 2009.
What a great New York drug heroin was, I thought. Like any city, but more than most, New York is an information overload, a constant perceptual tornado that surrounds you most places you walk on the streets. Heroin is the audio-visual technology that helps manage that overload by dampening it in general and allowing a focus on some part of it that the human perceptual equipment was, in fact, designed to handle.
- ↑ "Time series modeling of heroin and morphine drug action – Springer". Link.springer.com. 1 January 2003. Retrieved 12 October 2013.
- ↑ 18.0 18.1 Martin WR, Fraser HF (September 1961). "A comparative study of physiological and subjective effects of heroin and morphine administered intravenously in postaddicts". Journal of Pharmacology and Experimental Therapeutics 133: 388–99. PMID 13767429.
- ↑ 19.0 19.1 Bourgois, Philippe; Jeff Schonberg (2009). Righteous Dopefiend. Berkeley and Los Angeles: University of California Press. ISBN 0-520-25498-8. Retrieved 13 October 2009.
- ↑ Abadinsky, Howard (2007). Organized Crime. Wadsworth.
- ↑ "Rolleston Report". Departmental Commission on Morphine and Heroin Addiction, United Kingdom. 1926. Retrieved 28 January 2011.
- ↑ "Nils Bejerot: The Swedish Addiction Epidemic in global perspective". Archived from the original on 22 June 2007.
- ↑ Goldacre, Ben (1998). "Methadone and Heroin: An Exercise in Medical Scepticism". Retrieved 18 December 2006.
- ↑ Haasen C, Verthein U, Degkwitz P, Berger J, Krausz M, Naber D (July 2007). "Heroin-assisted treatment for opioid dependence: randomised controlled trial". Br J Psychiatry 191: 55–62. doi:10.1192/bjp.bp.106.026112. PMID 17602126.
- ↑ "Heroin Assisted Treatment for Opiate Addicts – The Swiss Experience". Parl.gc.ca. 31 March 1995. Archived from the original on 20 January 2010. Retrieved 12 October 2013.
- ↑ Nadelmann, Ethan (10 July 1995). "Switzerland's Heroin Experiment". Drug Policy Alliance. Archived from the original on 29 November 2004. Retrieved 22 October 2006.
- ↑ "Swiss approve prescription heroin". BBC News Online. 30 November 2008. Retrieved 30 November 2008.
- ↑ "Heroin prescription 'cuts costs'". BBC News. 5 June 2005. Retrieved 22 October 2006.
- ↑ "About the study". North American Opiate Medication Initiative. Retrieved 22 October 2006.
- ↑ Nordt C, Stohler R (2006). "Incidence of heroin use in Zurich, Switzerland: a treatment case register analysis". The Lancet 367 (9525): 1830–4. doi:10.1016/S0140-6736(06)68804-1. PMID 16753485.
- ↑ "Danmark redo för skattebetalt heroin" (in Swedish). November 2008. Archived from the original on 3 December 2008. Retrieved 30 November 2008.
- ↑ "Gratis heroin klar til danske narkomaner" (in Danish). Information. January 2010. Retrieved 14 February 2010.
- ↑ "Heroin-behandling bliver kun i kanyler" (in Danish). Information. February 2009. Retrieved 14 February 2010.
- ↑ "Prescription of injectable heroin for drug users". Danish National Boad of Health. October 2007. Retrieved 14 February 2010.
- ↑ "Durchbruch für die Behandlung von Schwerstopiatabhängigen" [Breakthrough for the treatment of heavily addicted opiate users] (in German). Bundesministerium für Gesundheit (German ministry of health). 28 May 2009. Retrieved 28 April 2014.
- ↑ Baselt, R. (2011). Disposition of Toxic Drugs and Chemicals in Man (9th ed.). Seal Beach, CA: Biomedical Publications. pp. 793–7. ISBN 978-0-9626523-8-7.
- ↑ Merck Manual of Home Health Handbook – 2nd edition, 2003, p. 2097
- ↑ Bell, Bethany (26 June 2012). "BBC News – Afghan opium crop failure 'led to UK heroin shortage'". Bbc.co.uk. Retrieved 3 November 2012.
- ↑ Dettmeyer RB, Preuss J, Wollersen H, Madea B (2005). "Heroin-associated nephropathy". Expert Opinion on Drug Safety 4 (1): 19–28. doi:10.1517/14740338.4.1.19. PMID 15709895.
- ↑ Darke S, Zador D (1996). "Fatal heroin 'overdose': a review". Addiction 91 (12): 1765–1772. doi:10.1046/j.1360-0443.1996.911217652.x. PMID 8997759.
- ↑ "Toxic Substances in water". Lincoln.pps.k12.or.us. Retrieved 20 October 2010.
- ↑ Breecher, Edward. "The Consumers Union Report on Licit and Illicit Drugs".
- ↑ Kolb L, Du Mez AG (1931). "Experimental addiction of animals to opiates" (PDF). U.S. Public Health Weekly Reports 46 (13): 698–726. doi:10.2307/4579992. PMC 1996590. PMID 19315288.
- ↑ The "heroin overdose" mystery and other occupational hazards of addiction, Schaffer Library of Drug Policy
- ↑ Gerevich J, Bácskai E, Farkas L, Danics Z (2005). "A case report: Pavlovian conditioning as a risk factor of heroin 'overdose' death". Harm Reduction Journal 2: 11. doi:10.1186/1477-7517-2-11. PMC 1196296. PMID 16042795.
- ↑ Hill MD, Cooper PW, Perry JR (January 2000). "Chasing the dragon—neurological toxicity associated with inhalation of heroin vapour: case report". CMAJ 162 (2): 236–8. PMC 1232277. PMID 10674060.
- ↑ Halloran O, Ifthikharuddin S, Samkoff L (2005). "Leukoencephalopathy from "chasing the dragon"". Neurology 64 (10): 1755. doi:10.1212/01.WNL.0000149907.63410.DA. PMID 15911804.
- ↑ Offiah C, Hall E (2008). "Heroin-induced leukoencephalopathy: characterization using MRI, diffusion-weighted imaging, and MR spectroscopy". Clinical Radiology 63 (2): 146–52. doi:10.1016/j.crad.2007.07.021. PMID 18194689.
- ↑ "Narcotic Drug Withdrawal". Discovery Place. Retrieved 18 April 2014.
- ↑ Myaddiction (16 May 2012). "Heroin Withdrawal Symptoms". MyAddiction. Retrieved 16 May 2012.
- ↑ Stephens, Richard (1991). The Street Addict Role: A Theory of Heroin Addiction. SUNY Press. p. 7. ISBN 9780791406199.
- ↑ Klous MG, Van den Brink W, Van Ree JM, Beijnen JH (2005). "Development of pharmaceutical heroin preparations for medical co-prescription to opioid dependent patients". Drug and Alcohol Dependence 80 (3): 283–95. doi:10.1016/j.drugalcdep.2005.04.008. PMID 15916865.
- ↑ Inturrisi CE, Schultz M, Shin S, Umans JG, Angel L, Simon EJ (1983). "Evidence from opiate binding studies that heroin acts through its metabolites". Life Sciences 33: 773–6. doi:10.1016/0024-3205(83)90616-1. PMID 6319928.
- ↑ Histamine release by morphine and diamorphine in man. & Cutaneous Complications of Intravenous Drug Abuse
- ↑ Brown GP, Yang K, King MA, Rossi GC, Leventhal L, Chang A, Pasternak GW (1997). "3-Methoxynaltrexone, a selective heroin/morphine-6β-glucuronide antagonist". FEBS Letters 412 (1): 35–8. doi:10.1016/S0014-5793(97)00710-2. PMID 9257684.
- ↑ 56.0 56.1 "Online Etymology Dictionary". Etymonline.com. Retrieved 20 October 2010.
- ↑ "The Most Addictive Drugs". Archived from the original on 13 February 2010.
- ↑ "Opium Throughout History". PBS Frontline. Retrieved 22 October 2006.
- ↑ Wright, C.R.A. (12 August 2003). "On the Action of Organic Acids and their Anhydrides on the Natural Alkaloids". Archived from the original on 6 June 2004. Note: this is an annotated excerpt of Wright, C.R.A. (1874). "On the Action of Organic Acids and their Anhydrides on the Natural Alkaloids". Journal of the Chemical Society 27: 1031–1043. doi:10.1039/js8742701031.
- ↑ Chemical Heritage Foundation Felix Hoffmann biography Page accessed April 26, 2015
- ↑ Jim Edwards for Business Insider . November 17, 2011 Yes, Bayer Promoted Heroin for Children -- Here Are The Ads That Prove It
- ↑ Deborah Moore for the TimesUnion. August 24, 2014 Heroin: A brief history of unintended consequences
- ↑ "Treaty of Versailles, Part X, Section IV, Article 298". 28 June 1919. pp. Annex, Paragraph 5. Retrieved 25 October 2008.
- ↑ "Journal of Pharmacology and Experimental Therapeutics (JPET) | Onset of Action and Drug Reinforcement" (PDF). Retrieved 10 June 2012.
- ↑ Eason, Kevin; Naughton, Philippe (13 March 2012). "First murder charge over heroin mix that killed 400". London: Times Online. Retrieved 20 July 2012.
- ↑ sepulfreak (8 July 2005). "Erowid Experience Vaults: Heroin – Catching the Waves – 41495". Erowid.org. Retrieved 20 July 2012.
- ↑ Halbsguth U, Rentsch KM, Eich-Höchli D, Diterich I, Fattinger K (2008). "Oral diacetylmorphine (heroin) yields greater morphine bioavailability than oral morphine: Bioavailability related to dosage and prior opioid exposure". British Journal of Clinical Pharmacology 66 (6): 781–791. doi:10.1111/j.1365-2125.2008.03286.x. PMC 2675771. PMID 18945270.
- ↑ http://www.idaat.org/files/documents_file-4.pdf
- ↑ "HEROIN, THE POPPY". Addiction Recovery Expose. Randolph Online Solutions Inc. Retrieved 27 May 2012.
- ↑ "Heroin". Mahalo.com. Mahalo.com Incorporated. Retrieved 27 May 2012.
- ↑ "Heroin". NACADA. NACADA. Archived from the original on 3 December 2012. Retrieved 27 May 2012.
- ↑ Sheryl Ubelacker (12 March 2012). "Medically prescribed heroin more cost-effective than methadone, study suggests". thestar.com (The Toronto Star). Retrieved 27 May 2012.
- ↑ "Heroin Legal Status". Vaults of Erowid. Erowid.org. Retrieved 27 May 2012.
- ↑ 21 CFR 1308.11 (CSA Sched I) with changes through 77 FR 64032 (18 October 2012)
- ↑ "Documentation of a heroin manufacturing process in Afghanistan. BULLETIN ON NARCOTICS, Volume LVII, Nos. 1 and 2, 2005" (PDF). United Nations Office on Drugs and Crime. Retrieved 20 October 2010.
- ↑ "Heroin—Illicit Drug Report" (PDF). Government of Australia. 2004. Retrieved 31 March 2014.
- ↑ Nazemroaya, Mahdi Darius (17 October 2006). "The War in Afghanistan: Drugs, Money Laundering and the Banking System". GlobalResearch.ca. Retrieved 22 October 2006.
- ↑ McGirk, Tim (2 August 2004). "Terrorism's Harvest: How al-Qaeda is tapping into the opium trade to finance its operations and destabilize Afghanistan". Time Magazine Asia. Retrieved 22 October 2006.
- ↑ "World failing to dent heroin trade, U.N. warns". Cnn.com. 21 October 2009. Retrieved 20 July 2012.
- ↑ technatica. "Afghanistan Heroin". Orwelltoday.com. Retrieved 20 July 2012.
- ↑ Andrew North (10 February 2004). "The drugs threat to Afghanistan". BBC. Retrieved 28 July 2013.
- ↑ Gall, Carolotta (3 September 2006). "Opium Harvest at Record Level in Afghanistan". New York Times – Asia Pacific. Retrieved 22 October 2006.
- ↑ Declan Walsh (30 August 2007). "UN horrified by surge in opium trade in Helmand". London: Guardian. Retrieved 20 July 2012.
- ↑ "Country Profile: Pakistan". United Nations Office on Drugs and Crime. Retrieved 5 January 2015.
- ↑ Eric C. Schneider, Smack: Heroin and the American City, University of Pennsylvania Press, 2008, chapter one
- ↑ 86.0 86.1 "War Views: Afghan heroin trade will live on.". Richard Davenport-Hines (BBC). October 200q. Retrieved 30 October 2008. Check date values in:
|date=(help) - ↑ "Haji Bagcho Sentenced To Life in Prison on Narco-Terrorism, Drug Trafficking Charges – Funded Taliban, Responsible for Almost 20 Percent of World's Heroin Production, More Than a Quarter-Billion in Drug Proceeds, Property Forfeited". The Aiken Leader. Retrieved 7 June 2012.
- ↑ 88.0 88.1 "Haji Bagcho Convicted by Federal Jury in Washington, D.C., on Drug Trafficking and Narco-terrorism Charges – Afghan National Trafficked More Than 123,000 Kilograms of Heroin in 2006". US Department of Justice. Retrieved 7 June 2012.
- ↑ 89.0 89.1 "Haji Bagcho Sentenced to Life in Prison on Trafficking/Narco-Terrorism Charges". Surfky News. Archived from the original on 16 January 2014. Retrieved 7 June 2012.
- ↑ 90.0 90.1 Foster, Zachary. "Haji Bagcho, One of World's Largest Heroin Traffickers, Convicted on Drug Trafficking, Narco-Terrorism Charges". War on Terrorism Online. Retrieved 7 June 2012.
- ↑ 91.0 91.1 91.2 TUCKER, ERIC (12 June 2012). "Afghan heroin trafficker gets life in US prison". Associated Press. Retrieved 7 June 2012.
- ↑ "2007 WORLD DRUG REPORT" (PDF). United Nations Office on Drugs and Crime. Retrieved 26 July 2012.
- ↑ European Monitoring Centre for Drugs and Drug Addiction (2008). Annual report: the state of the drugs problem in Europe (PDF). Luxembourg: Office for Official Publications of the European Communities. p. 70. ISBN 978-92-9168-324-6.
- ↑ United Nations Office on Drugs and Crime (2008). World drug report (PDF). United Nations Publications. p. 49. ISBN 978-92-1-148229-4.
- ↑ Nutt, D.; King, L. A.; Saulsbury, W.; Blakemore, C. (2007). "Development of a rational scale to assess the harm of drugs of potential misuse". The Lancet 369 (9566): 1047–1053. doi:10.1016/S0140-6736(07)60464-4. PMID 17382831.
- ↑ Kimber J, Dolan K, Wodak A (2005). "Survey of drug consumption rooms: service delivery and perceived public health and amenity impact". Drug and Alcohol Review 24 (1): 21–4. doi:10.1080/09595230500125047. PMID 16191717.
- ↑ http://www.idaat.org/files/newsletters_file-8.pdf
- ↑ Lancashire Constabulary-Harm Reduction in the Community page 7
- ↑ Janelle Oswald (9 December 2007). "The Real American Gangster". voice-online. Archived from the original on 15 May 2011. Retrieved 8 March 2008.
She spent five years in prison for aiding her husband's narcotic smuggling trade. Having to get used to the public life again after living like a 'ghost' since her release, the making of her partner's life on the big screen has brought back many memories, some good and some bad.
- ↑ Vallely, Paul (10 September 2005). "Gia: The tragic tale of the world's first supermodel". The Independent (London). Retrieved 12 May 2009.
- ↑ Requiem for a Dream (2000) – IMDb
- ↑ Martin, Henry; Waters, Keith (25 January 2008). Essential Jazz: The First 100 Years. Cengage Learning. p. 168. ISBN 978-0-495-50525-9. Retrieved 26 August 2012.
- ↑ Guardian newspaper 28 June 2012
- ↑ See, e.g., Azerrad, Michael. Come as You Are: The Story of Nirvana. Doubleday, 1994, at 241. ISBN 0-385-47199-8.
- ↑ "Philip Anselmo Opens Up About His Heroin Addiction, Pantera's Breakup". Blabbermouth.net. 19 August 2009. Retrieved 12 October 2013.
- ↑ Sweeting, Adam (9 July 2004). "I died. I do remember that". The Guardian (London).
- ↑ Brown, Peter. The Love You Make: An Insider's Story of The Beatles. McGraw-Hill, 1983. New American Library, 2002. 331.
- ↑ Matthew Bates (December 2008). "Loaded – Great heroin songs of the rock era" (PDF). pp. 26–27. Archived from the original (PDF) on 9 April 2008. Retrieved 17 January 2008.
- ↑ Liner notes, Music Bank box set. 1999.
- ↑ "Slate Tribute to Jim Carroll". Retrieved 2 January 2014.
Further reading
- Diary of a Drug Fiend by Aleister Crowley (1922)
- Junkie by William S. Burroughs (1953) ISBN 0-14-200316-6
- Heroin (1998) ISBN 1-56838-153-0
- Heroin Century (2002) ISBN 0-415-27899-6
- Thick As Thieves by Steve Geng (2007) ISBN 0805080562
- This is Heroin (2002) ISBN 1-86074-424-9
- The Heroin User's Handbook by Francis Moraes (paperback 2004) ISBN 1-55950-216-9
- The Little Book of Heroin by Francis Moraes (paperback 2000) ISBN 0-914171-98-4
- Heroin: A True Story of Addiction, Hope and Triumph by Julie O'Toole (paperback 2005) ISBN 1-905379-01-3
- The Heroin Diaries: A Year in the Life of a Shattered Rockstar by Nikki Sixx (2007) ISBN 978-0-7434-8628-6
- Heroin: The Myths and the Facts by Richard Ashley (1972), St. Martin's Press, Library of Congress No. 72-89417
- "The Death Proclamation of Generation X: A Self-Fulfilling Prophesy of Goth, Grunge and Heroin" by Maxim W. Furek, M. (2008), i-Universe. ISBN 978-0-595-46319-0
- Seeds of Terror: How Heroin is Bankrolling the Taliban and Al Qaeda, by Gretchen Peters, publ. Thomas Dunne Books (2009)
- Forbes, Andrew ; Henley, David (2011). Traders of the Golden Triangle. Chiang Mai: Cognoscenti Books. ASIN: B006GMID5K
External links
| Wikimedia Commons has media related to Heroin. |
| Look up heroin in Wiktionary, the free dictionary. |
- UNODC – United Nations Office on Drugs and Crime – Afghan Opium Survey 2009
- NIDA InfoFacts on Heroin
- ONDCP Drug Facts
- Heroin news page – Alcohol and Drugs History Society
- Protocols of the Learned Experts on Heroin Thomas Szasz M.D.
- U.S. National Library of Medicine: Drug Information Portal – Heroin
- Geopium: Geopolitics of Illicit Drugs in Asia, especially opium and heroin production and trafficking in and around Afghanistan and Burma (Articles and maps and French and English)
- National Alliance of Advocates for Buprenorphine Treatment – non-profit education website for treatment of Heroin addiction
- United States Department of State fact sheet: anti-narcotics efforts in Pakistan – dated 7 June 2002
- BBC Article entitled 'When Heroin Was Legal'. References to the United Kingdom and the United States
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||
| ||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

