Fructosamine
Fructosamines are compounds that result from glycation reactions between a sugar (such as fructose or glucose) and a primary amine, followed by isomerization via the Amadori rearrangement. Biologically, fructosamines are recognized by fructosamine-3-kinase, which may trigger the degradation of advanced glycation end-products (though the true clinical significance of this pathway is unclear). Fructosamine can also refer to the specific compound 1-amino-1-deoxy-D-fructose (isoglucosamine), first synthesized by Nobel laureate Hermann Emil Fischer in 1886.
Most commonly, fructosamine refers to a laboratory test for diabetes management that it is rarely used in clinical practice (simple blood glucose monitoring or hemoglobin A1c testing are preferred). Many direct-to-consumer lab testing companies sell fructosamine tests, but these are unnecessary and of limited clinical value.
Use in medicine
In diabetes, maintaining a normal blood glucose is essential to preventing many medical complications, including heart attacks and blindness. Most commonly, blood sugars are measured by either blood glucose monitoring which measures the current blood glucose level, or by Glycated hemoglobin (HbA1c) which measures average glucose levels over approximately 3 months.
In a similar way to hemoglobin A1c testing (which measures the glycation of hemoglobin), fructosamine testing determines the fraction of total serum proteins that have undergone glycation (the glycated serum proteins). Since albumin is the most abundant protein in blood, fructosamine levels typically reflect albumin glycation. (Some fructosamine tests specifically quantify the glycation of albumin, or glycated serum albumin instead of all proteins.). Because albumin has a half-life of approximately 20 days, the plasma fructosamine concentration reflects relatively recent (1-2 week) changes in blood glucose.
In patients with diseases that reduce red blood cell lifespan, such as hemolytic anaemia or hemoglobinopathies such as sickle-cell disease, a hemoglobin-based A1c test can be misleadingly low. A1c results may also be falsely high or low in hemoglobinopathies because abnormal hemoglobin variants can interfere in the analysis. In these cases, fructosamine measurement can be used as a marker of blood sugar levels, as its measurements are based on albumin instead of hemoglobin. However, any condition that changes serum albumin (such as the nephrotic syndrome) will affect the fructosamine result.
In practice, fructosamine is rarely measured clinically (even in individuals with hemoglobinopathies or other red cell disorders) due to a number of pragmatic concerns. First, diabetes care is rarely changed in short (1-4 week) intervals, since diabetes medications can take months to reach a steady state. An exception to this is pregnancy, where medication needs can change more rapidly and fructosamine may help provide closer short-term monitoring. Second, fructosamine has higher variability than A1c tests. Third, the overwhelming majority of studies in diabetes care are based on A1c measurements, which can make fructosamine results difficult to interpret. Fourth, the A1c test is incredibly well standardized[1] and trusted due to its nearly universal use. A variety of more advanced forms of the A1c test (e.g. some types of HPLC, immunoassay and capillary electrophoresis) can more accurately assay A1c levels during complex hemoglobinopathies and other conditions.[2] However this does not overcome the effect on A1c results of reduced red cell lifespan.
Interpretation of results
There is no standard reference range available for this test. The reference values depends upon the factors of patient age, gender, sample population, and test method. Hence, each laboratory report will include the patient's specific reference range for the test. An increase in fructosamine in lab testing results usually means an increase in glucose in the blood.
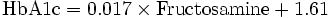
On average, each change of 3.3 mmol (60 mg/dl) in average blood sugar levels will give rise to changes of 2% HbA1c and 75 µmol fructosamine values.[3] However, this overemphasizes the upper-limit of many laboratories' reference ranges of 285 μmol/L as equivalent to HbA1c 7.5% rather than 6.5%. A comparative study,[4] which has been used in official advice for Quality and Outcomes Framework guidance in the UK[5] and summaried by the United States' National Quality Measures Clearinghouse:[6] gives the following formula and resulting values:
- Hence:

| Fructosamine (µmol) | HbA1c % | HbA1c IFCC (mmol/mol) |
|---|---|---|
| 200 | 5 | 31 |
| 258 | 6 | 42 |
| 288 | 6.5 | 48 |
| 317 | 7 | 53 |
| 346 | 7.5 | 58 |
| 375 | 8 | 64 |
| 435 | 9 | 75 |
| 494 | 10 | 86 |
| 552 | 11 | 97 |
| 611 | 12 | 108 |
See also
Footnotes
- ↑ National Glycohemoglobin Standardization Program, http://www.ngsp.org
- ↑ Sacks, D. B. (2003). "Hemoglobin variants and hemoglobin A1c analysis: Problem solved?". Clinical chemistry 49 (8): 1245–1247. doi:10.1373/49.8.1245. PMID 12881436.
- ↑ Bartol T (2000-12-01). "Comparison of Blood Glucose, HbA1c, and Fructosamine". Retrieved 2007-06-04. - gives a comparison chart and cites following source:
- Nathan DM, Singer DE, Hurxthal K, Goodson JD (1984). "The clinical information value of the glycosylated hemoglobin assay". N. Engl. J. Med. 310 (6): 341–6. doi:10.1056/NEJM198402093100602. PMID 6690962.
- ↑ Cohen RM, Holmes YR, Chenier TC, Joiner CH (2003). "Discordance between HbA1c and fructosamine: evidence for a glycosylation gap and its relation to diabetic nephropathy". Diabetes Care 26 (1): 163–7. doi:10.2337/diacare.26.1.163. PMID 12502674.
- ↑ "Diabetes (DM) Indicator 20 The percentage of patients with diabetes in whom the last HbA1c is 7.5 or less (or equivalent test/reference range depending on local laboratory) in the previous 15 months". Quality and outcomes framework Guidance 2006 (PDF). BMA. p. 39. Retrieved 2008-01-02.
- ↑ "Diabetes mellitus: the percentage of patients with diabetes in whom the last HbA1c is 7.5 or less (or equivalent test/reference range depending on local laboratory) in the previous 15 months". National Quality Measures Clearinghouse. 2007-12-31. Retrieved 2008-01-02.
External links
- Fructosamine at Lab Tests Online
- Fructosamine: analyte monograph - The Association for Clinical Biochemistry and Laboratory Medicine
| ||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||