Flexor retinaculum of the hand
| Flexor retinaculum of the hand | |
|---|---|
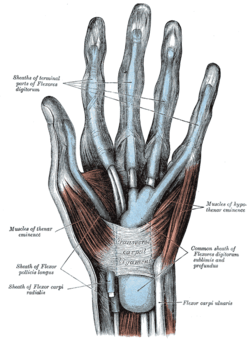 The mucous sheaths of the tendons on the front of the wrist and digits. (Transverse carpal ligament labeled at center.) | |
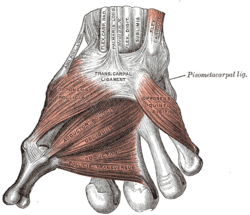 The muscles of the thumb. (Trans. carpal ligament labeled at center.) | |
| Details | |
| Latin | retinaculum musculorum flexorum manus (obsolete: ligamentum transversum carpi)[1] |
| Identifiers | |
| Gray's | p.456 |
| Dorlands /Elsevier | r_10/12706090 |
| TA | A04.6.03.013 |
| Anatomical terminology | |
The flexor retinaculum (transverse carpal ligament, or anterior annular ligament) is a strong, fibrous band that arches over the carpus, converting the deep groove on the front of the carpal bones into a tunnel, the carpal tunnel, through which the Flexor tendons of the digits and the median nerve pass.
It is attached, medially, to the pisiform and the hamulus of the hamate bone; laterally, to the tubercle of the scaphoid, and to the medial part of the volar surface and the ridge of the trapezium.
It is continuous, superficially, with the volar carpal ligament; and deep, with the palmar aponeurosis. It is crossed by the ulnar vessels and nerve, and the cutaneous branches of the median and ulnar nerves.
At its lateral end is the tendon of the flexor carpi radialis, which lies in the groove on the greater multangular between the attachments of the ligament to the bone.
On its volar surface the tendons of the palmaris longus and flexor carpi ulnaris are partly inserted; below, it gives origin to the short muscles of the thumb and little finger.
Clinical Significance

In carpal tunnel syndrome, inflammation of one of the nine tendons passing through the carpal tunnel causes pressure against the flexor retinaculum. However, the flexor retinaculum, being a sheath of tough connective tissue, has very limited stretching capabilities and is unable to accommodate the space necessary to relieve such pressure. Due to this increased pressure with no room to expand against either the bones of the wrist or the flexor retinaculum, the median nerve is ultimately compressed, resulting in the symptoms of carpal tunnel syndrome.[2]
In treating carpal tunnel syndrome with surgical intervention (usually done after all non-surgical methods of treatment have been exhausted), the flexor retinaculum is always the structure targeted to relieve pressure in the carpal tunnel. In these surgeries, the flexor retinaculum is either simply severed or lengthened. When surgery is done to divide the flexor retinaculum (which is by far the more common procedure), scar tissue will eventually fill the gap left by surgery. The intent is that this will lengthen the flexor retinaculum enough to accommodate inflamed or damaged tendons and reduce the effects of compression on the median nerve. In a 2004 double blind-study, researchers concluded that there was no perceivable benefit gained from lengthening the flexor retinaculum during surgery and so division of the ligament remains the preferred method of surgery.[3]
See also
- Peroneal retinacula
- Dorsal carpal ligament
- Extensor retinaculum of the hand
Additional images
-

Transverse section across the wrist and digits.
-
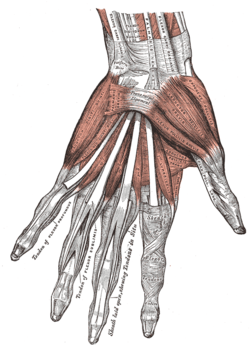
The muscles of the left hand. Palmar surface.
-
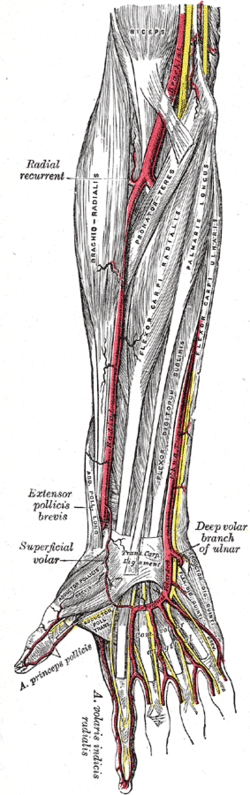
The radial and ulnar arteries.
-
Flexor retinaculum of the hand
References
This article incorporates text in the public domain from the 20th edition of Gray's Anatomy (1918)
- ↑ Kachlika, David; Bozdechovac, Ivana; Cechd, Pavel; Musile, Vladimir; Bacaa, Vaclav (2009). "Mistakes in the usage of anatomical terminology in clinical practice" (PDF). Biomedical papers of the Medical Faculty of the University Palacky, Olomouc, Czechoslovakia 153 (2): 157–61. PMID 19771143.
- ↑ Saladin, Kenneth S. Anatomy & Physiology The Unity of Form and Function. 6th. New York: McGraw-Hill, 2012.
- ↑ Dias, J J, et al. "Carpal tunnel decompression. Is lengthening of the flexor retinaculum better than simple division?" J Hand Surg Br. (2004): 271-6.
External links
- Anatomy figure: 08:04-08 at Human Anatomy Online, SUNY Downstate Medical Center
- Hand kinesiology at the University of Kansas Medical Center
- lesson5flexretinac&palmapon at The Anatomy Lesson by Wesley Norman (Georgetown University)
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
