Eating disorder
| Eating disorder | |
|---|---|
| Classification and external resources | |
| ICD-10 | F50 |
| ICD-9 | 307.5 |
| MeSH | D001068 |
Eating disorders are psychological illnesses defined by abnormal eating habits that may involve either insufficient or excessive food intake to the detriment of an individual's physical and mental health. Bulimia nervosa and anorexia nervosa are the most common specific forms of eating disorders.[1] Other types of eating disorders include binge eating disorder and OSFED.
Bulimia nervosa is a disorder characterized by binge eating and purging. Purging can include self-induced vomiting, over-exercising, and the usage of diuretics, enemas, and laxatives. Anorexia nervosa is characterized by extreme food restriction to the point of self-starvation and excessive weight loss.[2] The extreme weight loss often causes women and girls who have begun menstruating to stop having menstrual periods, a condition known as amenorrhea, although some women who meet the other DSM-5 criteria for anorexia nervosa still report some menstrual activity.[3] The DSM-5 currently specifies two subtypes of anorexia nervosa—the restricting type and the binge/purge type. Those who suffer from the restricting type of anorexia nervosa lose weight by restricting food intake and sometimes by over-exercising, whereas those suffering from the binge/purge type overeat and/or compensate through some method of purging.[4] The difference between anorexia nervosa binge/purge type and bulimia nervosa is the body weight of a person. Those diagnosed with anorexia nervosa binge/purge type are well under a healthy bodyweight, while those with bulimia nervosa may have a body weight that falls within the range from normal to overweight and obese .[5][6] Though primarily thought of as affecting females (an estimated 5–10 million being affected in the UK), eating disorders affect males as well. An estimated 10 – 15% of people with eating disorders are males (Gorgan, 1999). (an estimated 1 million UK males being affected).[7][8][9]
Although eating disorders are increasing all over the world among both men and women, there is evidence to suggest that it is women in the Western world who are at the highest risk of developing them and the degree of westernization increases the risk.[10] Nearly half of all Americans personally know someone with an eating disorder.
The skill to comprehend the central processes of appetite has increased tremendously since leptin was discovered, and the skill to observe the functions of the brain as well.[11] Interactions between motivational, homeostatic and self-regulatory control processes are involved in eating behavior, which is a key component in eating disorders.[12]
The precise cause of eating disorders is not entirely understood, but there is evidence that it may be linked to other medical conditions and situations. Cultural idealization of thinness and youthfulness have contributed to eating disorders affecting diverse populations. One study showed that girls with ADHD have a greater chance of getting an eating disorder than those not affected by ADHD.[13][14] Another study suggested that women with PTSD, especially due to sexually related trauma, are more likely to develop anorexia nervosa.[15][16][17] One study showed that foster girls are more likely to develop bulimia nervosa.[18] Some think that peer pressure and idealized body-types seen in the media are also a significant factor. Some research shows that for certain people there are genetic reasons why they may be prone to developing an eating disorder.[19] Recent studies have found evidence of a correlation between patients with bulimia nervosa and substance use disorders. In addition, anxiety disorders and personality disorders are common occurrences with clients of eating disorders.[20] People with eating disorders may have a dysfunctional hunger cognitive module which causes various feelings of distress to make them feel hungry.[21][22]
While proper treatment can be highly effective for many suffering from specific types of eating disorders, the consequences of eating disorders can be severe, including death[23][23][24] (whether from direct medical effects of disturbed eating habits or from comorbid conditions such as suicidal thinking).[1][25]
Classification
Currently recognized in medical manuals
These eating disorders are specified as mental disorders in standard medical manuals, such as in the ICD-10,[26] the DSM-5, or both.
- Anorexia nervosa (AN), characterized by lack of maintenance of a healthy body weight, an obsessive fear of gaining weight or refusal to do so, and an unrealistic perception, or non-recognition of the seriousness, of current low body weight.[27] Anorexia can cause menstruation to stop, and often leads to bone loss, loss of skin integrity, etc. It greatly stresses the heart, increasing the risk of heart attacks and related heart problems. The risk of death is greatly increased in individuals with this disease.[28] The most underlining factor researchers are starting to take notice of is that it may not just be a vanity, social, or media issue, but it could also be related to biological and or genetic components.[29]The DSM- 5 contains many changes that better represent patients with these conditions. The DSM-IV required amenorrhea (the absence of the menstrual cycle) to be present in order to diagnose a patient with anorexia.[30] This is no longer a requirement in the DSM-5.
- Bulimia nervosa (BN), characterized by recurrent binge eating followed by compensatory behaviors such as purging (self-induced vomiting, excessive use of laxatives/diuretics, or excessive exercise). Fasting and over-exercising may also be used as a method of purging following a binge.
- Binge Eating Disorder (BED), characterized by recurring binge eating at least once a week for over a period of 3 months while experiencing lack of control[31] and guilt after overeating.[32] The disorder can develop within individuals of a wide range of ages and socioeconomic classes.[33][34]
- Other Specified Feeding or Eating Disorder (OSFED) is an eating or feeding disorder that does not meet full DSM-5 criteria for AN, BN, or BED. Examples of otherwise-specified eating disorders include individuals with atypical anorexia nervosa, who meet all criteria for AN except being underweight, despite substantial weight loss; atypical bulimia nervosa, who meet all criteria for BN except that bulimic behaviors are less frequent or have not been ongoing for long enough; purging disorder; and night eating syndrome.
Not currently recognized in standard medical manuals
- Compulsive overeating, (COE), in which individuals habitually graze on large quantities of food rather than binging, as would be typical of binge eating disorder.
- Diabulimia, characterized by the deliberate manipulation of insulin levels by diabetics in an effort to control their weight.
- Food maintenance, characterized by a set of aberrant eating behaviors of children in foster care.[35]
- Orthorexia nervosa, a term used by Steven Bratman to characterize an obsession with a "pure" diet, in which people develop an obsession with avoiding unhealthy foods to the point where it interferes with a person's life.
- Selective eating disorder, also called picky eating, is an extreme sensitivity to how something tastes. A person with SED may or may not be a supertaster.
- Drunkorexia, commonly characterized by purposely restricting food intake in order to reserve food calories for alcoholic calories, exercising excessively in order to burn calories consumed from drinking, and over-drinking alcohols in order to purge previously consumed food.[36]
- Pregorexia, characterized by extreme dieting and over-exercising in order to control pregnancy weight gain. Under-nutrition during pregnancy is associated with low birth weight, coronary heart disease, type 2 diabetes, stroke, hypertension, cardiovascular disease risk, and depression.[37]
- Gourmand syndrome, a rare condition occurring after damage to the frontal lobe, resulting in an obsessive focus on fine foods.[38]
Causes
There are many causes of eating disorders, including biological, psychological and/or environmental abnormalities. Many people with eating disorders suffer also from body dysmorphic disorder, altering the way a person sees himself or herself.[39][40] Studies have found that a high proportion of individuals diagnosed with body dysmorphic disorder also had some type of eating disorder, with 15% of individuals having either anorexia nervosa or bulimia nervosa.[39] This link between body dysmorphic disorder and anorexia stems from the fact that both BDD and anorexia nervosa are characterized by a preoccupation with physical appearance and a distortion of body image.[40] There are also many other possibilities such as environmental, social and interpersonal issues that could promote and sustain these illnesses.[41][42] Also, the media are oftentimes blamed for the rise in the incidence of eating disorders due to the fact that media images of idealized slim physical shape of people such as models and celebrities motivate or even force people to attempt to achieve slimness themselves. The media are accused of distorting reality, in the sense that people portrayed in the media are either naturally thin and thus unrepresentative of normality or unnaturally thin by forcing their bodies to look like the ideal image by putting excessive pressure on themselves to look a certain way.[43] While past findings have described the causes of eating disorders as primarily psychological, environmental, and sociocultural, new studies have uncovered evidence that there is a prevalent genetic/heritable aspect of the causes of eating disorders.[44]
Biological
- Genetic: Numerous studies have been undertaken that show a possible genetic predisposition toward eating disorders as a result of Mendelian inheritance.[45][45][46] It has also been shown that eating disorders can be heritable. Recent twin studies have found slight instances of genetic variance when considering the different criterion of both anorexia nervosa and bulimia nervosa as endophenotypes contributing to the disorders as a whole.[42] In another recent study, twin and family studies led researchers to discover a genetic link on chromosome 1 that can be found in multiple family members of an individual with anorexia nervosa, indicating an inheritance pattern found between family members of others that have been previously diagnosed with an eating disorder.[44] A study found that an individual who is a first degree relative of someone who has suffered or currently suffers from an eating disorder is seven to twelve times more likely to suffer from an eating disorder themselves.[47] Twin studies also have shown that at least a portion of the vulnerability to develop eating disorders can be inherited, and there has been sufficient evidence to show that there is a genetic locus that shows susceptibility for developing anorexia nervosa.[47]
- Epigenetics: Epigenetic mechanisms are means by which environmental effects alter gene expression via methods such as DNA methylation; these are independent of and do not alter the underlying DNA sequence. They are heritable, but also may occur throughout the lifespan, and are potentially reversible. Dysregulation of dopaminergic neurotransmission due to epigenetic mechanisms has been implicated in various eating disorders.[48] One study has found that "epigenetic mechanisms may contribute to the known alterations of ANP homeostasis in women with eating disorders."[48][49]
- Biochemical: Eating behavior is a complex process controlled by the neuroendocrine system, of which the Hypothalamus-pituitary-adrenal-axis (HPA axis) is a major component. Dysregulation of the HPA axis has been associated with eating disorders,[50][51] such as irregularities in the manufacture, amount or transmission of certain neurotransmitters, hormones[52] or neuropeptides[53] and amino acids such as homocysteine, elevated levels of which are found in AN and BN as well as depression.[54]
- serotonin: a neurotransmitter involved in depression also has an inhibitory effect on eating behavior.[55][56][57][58][59]
- norepinephrine is both a neurotransmitter and a hormone; abnormalities in either capacity may affect eating behavior.[60][61]
- dopamine: which in addition to being a precursor of norepinephrine and epinephrine is also a neurotransmitter which regulates the rewarding property of food.[62][63]
- Neuropeptide Y also known as NPY is a hormone that encourages eating and decreases metabolic rate.[64] Blood levels of NPY are elevated in patients with anorexia nervosa, and studies have shown that injection of this hormone into the brain of rats with restricted food intake increases their time spent running on a wheel. Normally the hormone stimulates eating in healthy patients, but under conditions of starvation it increases their activity rate, probably to increase the chance of finding food.[64] The increased levels of NPY in the blood of patients with eating disorders can in some ways explain the instances of extreme over-exercising found in most anorexia nervosa patients.
- leptin and ghrelin: leptin is a hormone produced primarily by the fat cells in the body; it has an inhibitory effect on appetite by inducing a feeling of satiety. Ghrelin is an appetite inducing hormone produced in the stomach and the upper portion of the small intestine. Circulating levels of both hormones are an important factor in weight control. While often associated with obesity, both hormones and their respective effects have been implicated in the pathophysiology of anorexia nervosa and bulimia nervosa.[65] Leptin can also be used to distinguish between constitutional thinness found in a healthy person with a low BMI and an individual with anorexia nervosa.[42][66]
- gut bacteria and immune system: studies have shown that a majority of patients with anorexia and bulimia nervosa have elevated levels of autoantibodies that affect hormones and neuropeptides that regulate appetite control and the stress response. There may be a direct correlation between autoantibody levels and associated psychological traits.[67][68] Later study revealed that autoantibodies reactive with alpha-MSH are, in fact, generated against ClpB, a protein produced by sertain gut bacteria e.g. Escherichia coli. ClpB protein was identified as a conformational antigen-mimetic of alpha-MSH. In patients with eating disorders plasma levels of anti-ClpB IgG and IgM correalated with patients' psychological traits[69]
- infection: PANDAS, is an abbreviation for Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections. Children with PANDAS "have obsessive-compulsive disorder (OCD) and/or tic disorders such as Tourette syndrome, and in whom symptoms worsen following infections such as "strep throat" and scarlet fever." (NIMH) There is a possibility that PANDAS may be a precipitating factor in the development of anorexia nervosa in some cases, (PANDAS AN).[70]
- lesions: studies have shown that lesions to the right frontal lobe or temporal lobe can cause the pathological symptoms of an eating disorder.[71][72][73]
- tumors: tumors in various regions of the brain have been implicated in the development of abnormal eating patterns.[74][75][76][77][78]
- brain calcification: a study highlights a case in which prior calcification of the right thalumus may have contributed to development of anorexia nervosa.[79]
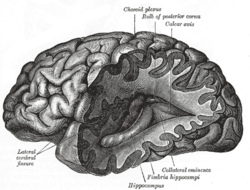
- somatosensory homunculus: is the representation of the body located in the somatosensory cortex, first described by renowned neurosurgeon Wilder Penfield. The illustration was originally termed "Penfield's Homunculus", homunculus meaning little man. "In normal development this representation should adapt as the body goes through its pubertal growth spurt. However, in AN it is hypothesized that there is a lack of plasticity in this area, which may result in impairments of sensory processing and distortion of body image". (Bryan Lask, also proposed by VS Ramachandran)
- Obstetric complications: There have been studies done which show maternal smoking, obstetric and perinatal complications such as maternal anemia, very pre-term birth (32<wks.), being born small for gestational age, neonatal cardiac problems, preeclampsia, placental infarction and sustaining a cephalhematoma at birth increase the risk factor for developing either anorexia nervosa or bulimia nervosa. Some of this developmental risk as in the case of placental infarction, maternal anemia and cardiac problems may cause intrauterine hypoxia, umbilical cord occlusion or cord prolapse may cause ischemia, resulting in cerebral injury, the prefrontal cortex in the fetus and neonate is highly susceptible to damage as a result of oxygen deprivation which has been shown to contribute to executive dysfunction, ADHD, and may affect personality traits associated with both eating disorders and comorbid disorders such as impulsivity, mental rigidity and obsessionality. The problem of perinatal brain injury, in terms of the costs to society and to the affected individuals and their families, is extraordinary. (Yafeng Dong, PhD)[80][81][82][83][84][85][86][87][88][89][90]
- Symptom of starvation: Evidence suggests that the symptoms of eating disorders are actually symptoms of the starvation itself, not of a mental disorder. In a study involving thirty-six healthy young men that were subjected to semi-starvation, the men soon began displaying symptoms commonly found in patients with eating disorders.[64][91] In this study, the healthy men ate approximately half of what they had become accustomed to eating and soon began developing symptoms and thought patterns (preoccupation with food and eating, ritualistic eating, impaired cognitive ability, other physiological changes such as decreased body temperature) that are characteristic symptoms of anorexia nervosa.[64] The men used in the study also developed hoarding and obsessive collecting behaviors, even though they had no use for the items, which revealed a possible connection between eating disorders and obsessive compulsive disorder.[64]
Psychological
Eating disorders are classified as Axis I[92] disorders in the Diagnostic and Statistical Manual of Mental Health Disorders (DSM-IV) published by the American Psychiatric Association. There are various other psychological issues that may factor into eating disorders, some fulfill the criteria for a separate Axis I diagnosis or a personality disorder which is coded Axis II and thus are considered comorbid to the diagnosed eating disorder. Axis II disorders are subtyped into 3 "clusters": A, B and C. The causality between personality disorders and eating disorders has yet to be fully established.[93] Some people have a previous disorder which may increase their vulnerability to developing an eating disorder.[94][95][96] Some develop them afterwards.[97] The severity and type of eating disorder symptoms have been shown to affect comorbidity.[98] The DSM-IV should not be used by laypersons to diagnose themselves, even when used by professionals there has been considerable controversy over the diagnostic criteria used for various diagnoses, including eating disorders. There has been controversy over various editions of the DSM including the latest edition, DSM-V, due in May 2013.[99][100][101][102][103]
Cognitive Attentional bias issues
Attentional bias may have an effect on eating disorders. Many studies have been performed to test this theory. (Shafran, Lee, Cooper, Palmer & Fairburn (2007), Veenstra and de Jong (2012) and Smeets, Jansen, & Roefs (2005)).
- Evidence of the Effect of Attentional Bias on Eating Disorders
Shafran, Lee, Cooper, Palmer and Fairburn (2007) studied the effect of attentional bias on eating disorders in women with anorexia, bulimia, and ED-NOS (Eating Disorder Not Otherwise Specified) compared to a control group and found that those affected by an eating disorder were quicker to identify "bad" eating scenarios than "good" ones.
- Attentional Bias in Anorexia Nervosa
A study of a more specific section of eating disorders has been performed by Veenstra and de Jong (2012.) It found that both the control and the eating disorder patients showed attentional bias against high fat foods and negative eating pictures. The eating disorder patients showed a larger attentional bias against the foods that are considered "bad." From this study it was hypothesized that a negative attentional bias might facilitate the restricted food intake of the eating disorder patients.
- Attentional Bias in body dissatisfaction
Smeets, Jansen, & Roefs (2005) studied body dissatisfaction and its relation to attentional bias and found that induced bias for unattractive body parts made the participants feel worse about themselves and their body satisfaction decreased, as well as the reverse when a positive bias was induced.
| Axis I | Axis II |
|---|---|
| depression[104] | obsessive compulsive personality disorder[105] |
| substance abuse, alcoholism[106] | borderline personality disorder[107] |
| anxiety disorders[108] | narcissistic personality disorder[109] |
| obsessive compulsive disorder[110][111] | histrionic personality disorder[112] |
| Attention-deficit hyperactivity disorder[13][113][114][115] | avoidant personality disorder[116] |
Personality traits
There are various childhood personality traits associated with the development of eating disorders.[117] During adolescence these traits may become intensified due to a variety of physiological and cultural influences such as the hormonal changes associated with puberty, stress related to the approaching demands of maturity and socio-cultural influences and perceived expectations, especially in areas that concern body image. Many personality traits have a genetic component and are highly heritable. Maladaptive levels of certain traits may be acquired as a result of anoxic or traumatic brain injury, neurodegenerative diseases such as Parkinson's disease, neurotoxicity such as lead exposure, bacterial infection such as Lyme disease or viral infection such as Toxoplasma gondii as well as hormonal influences. While studies are still continuing via the use of various imaging techniques such as fMRI; these traits have been shown to originate in various regions of the brain[118] such as the amygdala[119][120] and the prefrontal cortex.[121] Disorders in the prefrontal cortex and the executive functioning system have been shown to affect eating behavior.[122][123]
Environmental influences
Child maltreatment
Child abuse which encompasses physical, psychological and sexual abuse, as well as neglect has been shown by innumerable studies to be a precipitating factor in a wide variety of psychiatric disorders, including eating disorders. Children who are subjected to abuse may develop eating disorders in an effort to gain some sense of control or for a sense of comfort, or they may be in an environment where the diet is unhealthy or insufficient. Child abuse and neglect can cause profound changes in both the physiological structure and the neurochemistry of the developing brain. Children who, as wards of the state, were placed in orphanages or foster homes are especially susceptible to developing a disordered eating pattern. In a study done in New Zealand 25% of the study subjects in foster care exhibited an eating disorder (Tarren-Sweeney M. 2006). An unstable home environment is detrimental to the emotional well-being of children, even in the absence of blatant abuse or neglect the stress of an unstable home can contribute to the development of an eating disorder.[124][125][126][127][128][129][130][131][132]
Social isolation
Social isolation has been shown to have a deleterious effect on an individual's physical and emotional well-being. Those that are socially isolated have a higher mortality rate in general as compared to individuals that have established social relationships. This effect on mortality is markedly increased in those with pre-existing medical or psychiatric conditions, and has been especially noted in cases of coronary heart disease. "The magnitude of risk associated with social isolation is comparable with that of cigarette smoking and other major biomedical and psychosocial risk factors." (Brummett et al.)
Social isolation can be inherently stressful, depressing and anxiety-provoking. In an attempt to ameliorate these distressful feelings an individual may engage in emotional eating in which food serves as a source of comfort. The loneliness of social isolation and the inherent stressors thus associated have been implicated as triggering factors in binge eating as well.[133][134][135][136]
Waller, Kennerley and Ohanian (2007) argued that both bingeing–vomiting and restriction are emotion suppression strategies, but they are just utilized at different times. For example, restriction is used to pre-empt any emotion activation, while bingeing–vomiting is used after an emotion has been activated.[137]
Parental influence
Parental influence has been shown to be an intrinsic component in the development of eating behaviors of children. This influence is manifested and shaped by a variety of diverse factors such as familial genetic predisposition, dietary choices as dictated by cultural or ethnic preferences, the parents' own body shape and eating patterns, the degree of involvement and expectations of their children's eating behavior as well as the interpersonal relationship of parent and child. This is in addition to the general psychosocial climate of the home and the presence or absence of a nurturing stable environment. It has been shown that maladaptive parental behavior has an important role in the development of eating disorders. As to the more subtle aspects of parental influence, it has been shown that eating patterns are established in early childhood and that children should be allowed to decide when their appetite is satisfied as early as the age of two. A direct link has been shown between obesity and parental pressure to eat more.
Coercive tactics in regard to diet have not been proven to be efficacious in controlling a child's eating behavior. Affection and attention have been shown to affect the degree of a child's finickiness and their acceptance of a more varied diet.[138][139][140][141][142][143]
Hilde Bruch, a pioneer in the field of studying eating disorders, asserts that anorexia nervosa often occurs in girls who are high achievers, obedient, and always trying to please their parents. Their parents have a tendency to be over-controlling and fail to encourage the expression of emotions, inhibiting daughters from accepting their own feelings and desires. Adolescent females in these overbearing families lack the ability to be independent from their families, yet realize the need to, often resulting in rebellion. Controlling their food intake may make them feel better, as it provides them with a sense of control.[144]
Peer pressure
In various studies such as one conducted by The McKnight Investigators, peer pressure was shown to be a significant contributor to body image concerns and attitudes toward eating among subjects in their teens and early twenties.
Eleanor Mackey and co-author, Annette M. La Greca of the University of Miami, studied 236 teen girls from public high schools in southeast Florida. "Teen girls' concerns about their own weight, about how they appear to others and their perceptions that their peers want them to be thin are significantly related to weight-control behavior," says psychologist Eleanor Mackey of the Children's National Medical Center in Washington and lead author of the study. "Those are really important."
According to one study, 40% of 9- and 10-year-old girls are already trying to lose weight.[145] Such dieting is reported to be influenced by peer behavior, with many of those individuals on a diet reporting that their friends also were dieting. The number of friends dieting and the number of friends who pressured them to diet also played a significant role in their own choices.[146][147][148][149]
Elite athletes have a significantly higher rate in eating disorders. Female athletes in sports such as gymnastics, ballet, diving, etc. are found to be at the highest risk among all athletes. Women are more likely than men to acquire an eating disorder between the ages of 13–30. 0–15% of those with bulimia and anorexia are men.
Cultural pressure
There is a cultural emphasis on thinness which is especially pervasive in western society. There is an unrealistic stereotype of what constitutes beauty and the ideal body type as portrayed by the media, fashion and entertainment industries. "The cultural pressure on men and women to be 'perfect' is an important predisposing factor for the development of eating disorders".[150][151] Further, when women of all races base their evaluation of their self upon what is considered the culturally ideal body, the incidence of eating disorders increases.[152] Eating disorders are becoming more prevalent in non-Western countries where thinness is not seen as the ideal, showing that social and cultural pressures are not the only causes of eating disorders.[153] For example, observations of anorexia in all of the non-Western regions of the world point to the disorder not being "culture-bound" as once thought.[154] However, studies on rates of bulimia suggest that it might be culturally bound. In non-Western countries, bulimia is less prevalent than anorexia, but these non-Western countries where it is observed can be said to have probably or definitely been influenced or exposed to Western culture and ideology.[155]
Socioeconomic status (SES) has been viewed as a risk factor for eating disorders, presuming that possessing more resources allows for an individual to actively choose to diet and reduce body weight.[156] Some studies have also shown a relationship between increasing body dissatisfaction with increasing SES.[157] However, once high socioeconomic status has been achieved, this relationship weakens and, in some cases, no longer exists.[154]
The media plays a major role in the way in which people view themselves. Countless magazine ads and commercials depict rail thin celebrities like Lindsay Lohan, Nicole Richie and Mary Kate Olsen, who appear to gain nothing but attention from their looks. Society has taught people that being accepted by others is necessary at all costs.[158] Unfortunately this has led to the belief that in order to fit in one must look a certain way. Televised beauty competitions such as the Miss America Competition contribute to the idea of what it means to be beautiful because competitors are evaluated on the basis of their opinion.[159]
In addition to socioeconomic status being considered a cultural risk factor so is the world of sports. Athletes and eating disorders tend to go hand in hand, especially the sports where weight is a competitive factor. Gymnastics, horse back riding, wrestling, body building, and dancing are just a few that fall into this category of weight dependent sports. Eating disorders among individuals that participate in competitive activities, especially women, often lead to having physical and biological changes related to their weight that often mimic prepubescent stages. Oftentimes as women's bodies change they loose their competitive edge which leads them to taking extreme measures to maintain their younger body shape. Men often struggle with binge eating followed by excessive exercise while focusing on building muscle rather than losing fat, but this goal of gaining muscle is just as much an eating disorder as obsessing over thinness. The following statistics taken from Susan Nolen-Hoeksema's book, (ab)normal psychology, shows the estimated percentage of athletes that struggle with eating disorders based on the category of sport.
- Aesthetic sports (dance, figure skating, gymnastics) – 35%
- Weight dependent sports (judo, wrestling) – 29%
- Endurance sports (cycling, swimming, running) – 20%
- Technical sports (golf, high jumping) – 14%
- Ball game sports (volleyball, soccer) – 12%
Although most of these athletes develop eating disorders to keep their competitive edge, others use exercise as a way to maintain their weigh and figure. This is just as serious as regulating food intake for competition. Even though there is mixed evidence showing at what point athletes are challenged with eating disorders, studies show that regardless of competition level all athletes are at higher risk for developing eating disorders that non-athletes, especially those that participate in sports where thinness is a factor.[160]
Pressure from society is also seen within the homosexual community. Homosexual men are at greater risk of eating disorder symptoms than heterosexual men.[161] Within the gay culture, muscularity gives the advantages of both social and sexual desirability and also power.[162] These pressures and ideas that another homosexual male may desire a mate who is thinner or muscular can possibly lead to eating disorders. The higher eating disorder symptom score reported, the more concern about how others perceive them and the more frequent and excessive exercise sessions occur.[162] High levels of body dissatisfaction are also linked to external motivation to working out and old age; however, having a thin and muscular body occurs within younger homosexual males than older.[161][162]
It is important to realize some of the limitations and challenges of many studies that try to examine the roles of culture, ethnicity, and SES. For starters, most of the cross-cultural studies use definitions from the DSM-IV-TR, which has been criticized as reflecting a Western cultural bias. Thus, assessments and questionnaires may not be constructed to detect some of the cultural differences associated with different disorders. Also, when looking at individuals in areas potentially influenced by Western culture, few studies have attempted to measure how much an individual has adopted the mainstream culture or retained the traditional cultural values of the area. Lastly, the majority of the cross-cultural studies on eating disorders and body image disturbances occurred in Western nations and not in the countries or regions being examined.[163]
While there are many influences to how an individual processes their body image, the media does play a major role. Along with the media, parental influence, peer influence, and self-efficacy beliefs also play a large role in an individual's view of themselves. The way the media presents images can have a lasting effect on an individual's perception of their body image. Eating disorders are a worldwide issue and while women are more likely to be affected by an eating disorder it still affects both genders (Schwitzer 2012). The media has an impact on eating disorders whether shown in a positive or negative light, it then has a responsibility to use caution when promoting images that projects an ideal that many turn to eating disorders to attain.[164]
Symptoms-complications
Symptoms and complications vary according to the nature and severity of the eating disorder:[165]
| acne | xerosis | amenorrhoea | tooth loss, cavities |
| constipation | diarrhea | water retention and/or edema | lanugo |
| telogen effluvium | cardiac arrest | hypokalemia | death |
| osteoporosis[166] | electrolyte imbalance | hyponatremia | brain atrophy[167][168] |
| pellagra[169] | scurvy | kidney failure | suicide[170][171][172] |
Some physical symptoms of eating disorders are weakness, fatigue, sensitivity to cold, reduced beard growth in men, reduction in waking erections, reduced libido, weight loss and failure of growth.[173] Unexplained hoarseness may be a symptom of an underlying eating disorder, as the result of acid reflux, or entry of acidic gastric material into the laryngoesophageal tract. Patients who induce vomiting, such as those with anorexia nervosa, binge eating-purging type or those with purging-type bulimia nervosa are at risk for acid reflux.[174] Polycystic ovary syndrome (PCOS) is the most common endocrine disorder to affect women. Though often associated with obesity it can occur in normal weight individuals. PCOS has been associated with binge eating and bulimic behavior.[175][176][177][178][179][180]
Pro-Ana subculture
Several websites promote eating disorders, and can provide a means for individuals to communicate in order to maintain eating disorders. Members of these websites typically feel that their eating disorder is the only aspect of a chaotic life that they can control.[181] These websites are often interactive and have discussion boards where individuals can share strategies, ideas, and experiences, such as diet and exercise plans that achieve extremely low weights.[182] A study comparing the personal web-blogs that were pro-eating disorder with those focused on recovery found that the pro-eating disorder blogs contained language reflecting lower cognitive processing, used a more closed-minded writing style, contained less emotional expression and fewer social references, and focused more on eating-related contents than did the recovery blogs.[183]
In men
To date, the evidence suggests that the gender bias of clinicians means that diagnosing either bulimia or anorexia in men is less likely despite identical behavior. Men are more likely to be diagnosed as suffering depression with associated appetite changes than receive a primary diagnosis of an eating disorder. Using examples from a Canadian context below, it is possible to engage with some of the more nuanced issues facing men suffering from disordered eating.
Until recently, eating disorders have been characterized as an almost exclusively female problem (Maine and Bunnell 2008). The majority of early academic scholarship during the early 1990s tended to dismiss the prevalence in men as largely, if not entirely, irrelevant when compared to that in women (Weltzin et al. 2005.). Only recently have sociologists and feminist thinkers expanded the scope of eating disorders to identify with the unique challenges facing male sufferers.
Eating disorders are the third most common chronic illness in adolescent boys (NEDIC, 2006). Using currently available data, it is estimated that 3% of men will be affected by eating disorders in their lifetime (Public Health Agency of Canada, 2002). Eating disorder rates are not only increasing among females but also males are more concerned with their body image than ever before. The Public Health Agency of Canada (2002) found that almost one in every two girls and almost one in every five boys of grade 10 either were on a diet or wanted to lose weight. Since 1987, hospitalizations for eating disorders in general hospitals have increased by 34% among young men under the age of 15 and by 29% among men between 15–24 years old (Public Health Agency of Canada, 2002). Across Canada, age-standardized hospital separation rates for eating disorders were highest among men in British Columbia (15.9 per 100,000) and New Brunswick (15.1 per 100,000) and lowest in Saskatchewan (8.6) and Alberta (8.6 per 100,000) (Public Health Agency of Canada, 2002).
Part of the challenge with addressing the prevalence of eating disorders in men is a lack of research and statistics that are both current and appropriate. Recent work, such as that by Schoen and Greenberg (Greenberg & Schoen, 2008) suggests that the same prevailing social factors which led to a rise in eating disorders amongst women in the late 1980s may have also clouded public perceptions of similar male vulnerabilities. As a result, male eating disorders and prevalence have been under-reported and misdiagnosed. Specifically, attention has recently been drawn to the gendered nature of diagnosis and dissimilar methods of presentation in men; diagnostic criteria focusing on weight loss, fear of fat and physical symptoms such as amenorrhea cannot be applied to male sufferers, many of whom exercise excessively, are concerned with muscularity and definition rather than absolute weight loss and rebel against terms such as 'fear of fat', which they view as disempowering and effeminising (Derenne & Beresin, 2006). As a result of these earlier attempts to express eating disorders amongst men using the language and concepts of non-comparable disorders amongst women, there is a substantial lack of data on prevalence, incidence and burden of disease for men, with much of what is available difficult to evaluate, poorly reported or simply incorrect.
The message that there is no ideal size, shape or weight that every individual should strive to achieve is still largely targeted at women, and those campaigns which include men still prominently feature gendered iconography (such as the ribbon), further raising the barrier to access for male sufferers (Maine & Bunnell, 2008). Male body image is not as homogeneous in the media (that is, the range for 'acceptable' male physiques is wider), but instead focuses on perceived or projected masculinity (Gaughen, 2004, 7 and Maine & Bunnell, 2008). More pressingly, there is no consensus in the literature regarding unique risk factors as they relate to gay or bisexual men; the US center for Population Research in LGBT health estimates prevalence in the LGBT community to be about twice the national average for women and approximately 3.5 times higher for men. At the same time, a similar research study (Feldman & Meyer, 2007) fails to establish an explanatory framework to address these findings, and a subsequent study (Hatzenbuehler et al., 2009) suggests that membership in the LGBT community offers some protection against psychiatric morbidity, including that from eating disorders. As mentioned above, a distinct lack of research continues to present a barrier to drawing a broad conclusion on this topic. A 2014 report in Salon estimated 42 percent of men who struggle with eating disorders, identify as gay, or bisexual.[184]
Existing treatment for men with eating disorders occurs in a similar environment as that for women. Men living in isolated, rural or small communities who are experiencing violence that sometimes leads to eating disorders face barriers accessing the treatment, as well as additional stigma due to suffering from a 'feminine' disease (Public Health Agency of Canada, 2002). The Public Health Agency of Canada (2011 report) also states that integrated treatment approaches to family violence and eating disorders are likely to become increasingly scarce as the resources required to ensure accessibility to services, appropriate medical care, sufficient staffing, shelters and transition houses and counseling for underlying abuse issues are no longer available. Many cases in Canada are referred to USA for the treatments due to the lack of appropriate services offered (Vitiello & Lederhendler 2000). For example, in one case, a patient suffering from anorexia nervosa, originally admitted to The Hospital For Sick Children in Toronto was later recommended for a transfer to a facility in Arizona (Jones, 2007). In 2006, the province of Ontario alone sent 45 patients (36 of them male) to the US for eating disorder treatment at a gross cost of $3,719,440 (Jones, 2007), a decision motivated by the lack of specialized facilities domestically.
Speaking from the feminist relational position, Maine and Bunnell (2008) suggest a unique approach towards managing eating disorders in men. They advocate for counseling that focuses on how patients respond to pressures and expectations rather than on addressing the individual pathology of disordered eating. Current treatments in this vein show some success (Public Health Agency of Canada, 2011), but lack patient-based review and feedback. Monitoring of physical symptoms, behavioral therapy, cognitive therapy, body image therapy, nutritional counseling, education and medication if necessary are currently available in some form, yet all of these programs are delivered regardless of patient gender (Public Health Agency, 2002 and Maine & Bunnell, 2008). Up to twenty percent of patients with eating disorders eventually die of their illness, and another fifteen percent resort to suicide. With access to treatment, 75 to 80% of female adolescents recover, yet less than half of males do (Macleans, 2005). Moreover, there are several limitations in the collection of data, as most studies are based on clinical samples, which make it hard to tell about the findings to general population. People with eating disorders require a broad range of treatment for both physical complications and psychological issues, at a cost of about $1 600 per day (Timothy & Cameron, 2005, 100). Treatment for patients who were diagnosed following a hospitalization resulting from their condition is both more expensive (approximately three times more), and also less successful, with a corresponding drop of over twenty percent in women and forty percent in men (Macleans, 2005).
There are many societal, familial and individual factors that can influence the development of an eating disorder. Individuals who are struggling with their identity and self-image can be at risk, as well as those who have experienced a traumatic event (A Report on Mental Illness in Canada, 2002). In addition, many sufferers of eating disorders report feeling powerless about their socioeconomic environment, and view dieting, exercise and purging as empowering means of controlling their lives. The conventional approach (Trebay, 2008 and Derenne & Beresin, 2006) to understanding the root causes of disordered eating focuses on the role of media and sociocultural pressures; an emphasis on thinness (for women) and muscularity (for men) often goes beyond simple body image. There is an implicit media message that not only are those with 'ideal' bodies can be more confident, successful, healthy and happy but that slimness is associated with positive character qualities, such as reliability, trustworthiness and honesty (Harvey & Robinson, 2003). The traditional understanding of eating disorders reflects a media construct where thin and attractive people are not only the most successful and desirable members of the community, but rather they are the only members of the community who can be attractive and desirable.
In such a view, society is focused on appearance; body image becomes central to young people's feelings of self-esteem and self-worth – overshadowing qualities and achievements in other aspects of their lives (Maine & Bunnell, 2008). Teenagers may associate success or acceptance by their peers with achieving the 'perfect' physical standard portrayed by the media. As a result, during the period where children and teenagers become increasingly more exposed to prevailing cultural norms, both males and females are at risk of developing skewed conceptions of self and their bodies (Andersen & Homan, 1997). When the desired goals of achieving the ideal body image are not met, they might experience feelings of failure that contribute to further drop in self-esteem, confidence, and an increase in body image dissatisfaction. Some also suffer psychological and physical costs such as feelings of shame, failure, deprivation, and yo-yo dieting (Maine & Bunnell, 2008). Eating disorders may cause individuals to feel tired and depressed, decreased mental functioning and concentration, and can lead to malnutrition with risk to bone health, physical growth, and brain development. There are also increased risks of osteoporosis and fertility problems, weakened immune system, heart rate, blood pressure and metabolic rate is also decreased (NEDIC, 2006). Additionally, sufferers from eating disorders show the third highest susceptibility for self-abuse and suicide, with rates 13.6 and 9.8 times higher than the Canadian average, respectively (Löwe et al., 2001).
Psychopathology
The psychopathology of eating disorders centers around body image disturbance, such as concerns with weight and shape; self-worth being too dependent on weight and shape; fear of gaining weight even when underweight; denial of how severe the symptoms are and a distortion in the way the body is experienced.[173]
Diagnosis
The initial diagnosis should be made by a competent medical professional. "The medical history is the most powerful tool for diagnosing eating disorders"(American Family Physician).[185] There are many medical disorders that mimic eating disorders and comorbid psychiatric disorders. All organic causes should be ruled out prior to a diagnosis of an eating disorder or any other psychiatric disorder. In the past 30 years eating disorders have become increasingly conspicuous and it is uncertain whether the changes in presentation reflect a true increase. Anorexia nervosa and bulimia nervosa are the most clearly defined subgroups of a wider range of eating disorders. Many patients present with subthreshold expressions of the two main diagnoses: others with different patterns and symptoms.[186]
Medical
The diagnostic workup typically includes complete medical and psychosocial history and follows a rational and formulaic approach to the diagnosis. Neuroimaging using fMRI, MRI, PET and SPECT scans have been used to detect cases in which a lesion, tumor or other organic condition has been either the sole causative or contributory factor in an eating disorder. "Right frontal intracerebral lesions with their close relationship to the limbic system could be causative for eating disorders, we therefore recommend performing a cranial MRI in all patients with suspected eating disorders" (Trummer M et al. 2002), "intracranial pathology should also be considered however certain is the diagnosis of early-onset anorexia nervosa. Second, neuroimaging plays an important part in diagnosing early-onset anorexia nervosa, both from a clinical and a research prospective".(O'Brien et al. 2001).[73][187]
Psychological
| Eating Attitudes Test[188] | SCOFF questionnaire[189] |
| Body Attitudes Test[190] | Body Attitudes Questionnaire[191] |
| Eating Disorder Inventory[192] | Eating Disorder Examination Interview[193] |
After ruling out organic causes and the initial diagnosis of an eating disorder being made by a medical professional, a trained mental health professional aids in the assessment and treatment of the underlying psychological components of the eating disorder and any comorbid psychological conditions. The clinician conducts a clinical interview and may employ various psychometric tests. Some are general in nature while others were devised specifically for use in the assessment of eating disorders. Some of the general tests that may be used are the Hamilton Depression Rating Scale[194] and the Beck Depression Inventory.[195][196] longitudinal research showed that there is an increase in chance that a young adult female would develop bulimia due to their current psychological pressure and as the person ages and matures, their emotional problems change or are resolved and then the symptoms decline.[197]
Differential diagnoses
There are multiple medical conditions which may be misdiagnosed as a primary psychiatric disorder, complicating or delaying treatment. These may have a synergistic effect on conditions which mimic an eating disorder or on a properly diagnosed eating disorder.
- Lyme disease which is known as the "great imitator", as it may present as a variety of psychiatric or neurological disorders including anorexia nervosa.[198][199]
- Addison's Disease is a disorder of the adrenal cortex which results in decreased hormonal production. Addison's disease, even in subclinical form may mimic many of the symptoms of anorexia nervosa.[200]
- Gastric adenocarcinoma is one of the most common forms of cancer in the world. Complications due to this condition have been misdiagnosed as an eating disorder.[201]
- Helicobacter pylori is a bacterium which causes stomach ulcers and gastritis and has been shown to be a precipitating factor in the development of gastric carcinomas. It also has an effect on circulating levels of leptin and ghrelin, two hormones which help regulate appetite. Upon successful treatment of helicobacter pylori associated gastritis in pre-pubertal children they showed "significant increase in BMI, lean and fat mass along with a significant decrease in circulating ghrelin levels and an increase in leptin levels" (Pacifico, L)."SUMMARY: H. pylori has an influence on the release of gastric hormones and therefore plays a role in the regulation of body weight, hunger and satiety,"(Weigt J, Malfertheiner P).[202][203]
- Hypothyroidism, hyperthyroidism, hypoparathyroidism and hyperparathyroidism may mimic some of the symptoms of, can occur concurrently with, be masked by or exacerbate an eating disorder.[204][205][206][207][208][209][210][211]
- Lupus: 19 psychiatric conditions have been associated with systemic lupus erythematosus (SLE), including depression and bipolar disorder.[212]
- Toxoplasma seropositivity: even in the absence of symptomatic toxoplasmosis, toxoplasma gondii exposure has been linked to changes in human behavior and psychiatric disorders including those comorbid with eating disorders such as depression. In reported case studies the response to antidepressant treatment improved only after adequate treatment for toxoplasma.[213]
- Neurosyphilis: It is estimated that there may be up to one million cases of untreated syphilis in the US alone. "The disease can present with psychiatric symptoms alone, psychiatric symptoms that can mimic any other psychiatric illness". Many of the manifestations may appear atypical. Up to 1.3% of short term psychiatric admissions may be attributable to neurosyphilis, with a much higher rate in the general psychiatric population. (Ritchie, M Perdigao J,)[214]
- Dysautonomia: a wide variety of autonomic nervous system (ANS) disorders may cause a wide variety of psychiatric symptoms including anxiety, panic attacks and depression. Dysautonomia usually involves failure of sympathetic or parasympathetic components of the ANS system but may also include excessive ANS activity. Dysautonomia can occur in conditions such as diabetes and alcoholism.
Psychological disorders which may be confused with an eating disorder, or be co-morbid with one:
- Emetophobia is an anxiety disorder characterized by an intense fear of vomiting. A person so afflicted may develop rigorous standards of food hygiene, such as not touching food with their hands. They may become socially withdrawn to avoid situations which in their perception may make them vomit. Many who suffer from emetophobia are diagnosed with anorexia or self-starvation. In severe cases of emetophobia they may drastically reduce their food intake.[215][216]
- Phagophobia is an anxiety disorder characterized by a fear of eating, it is usually initiated by an adverse experience while eating such as choking or vomiting. Persons with this disorder may present with complaints of pain while swallowing.[217]
- Body dysmorphic disorder (BDD) is listed as a somatoform disorder that affects up to 2% of the population. BDD is characterized by excessive rumination over an actual or perceived physical flaw. BDD has been diagnosed equally among men and women. While BDD has been misdiagnosed as anorexia nervosa, it also occurs comorbidly in 39% of eating disorder cases. BDD is a chronic and debilitating condition which may lead to social isolation, major depression and suicidal ideation and attempts. Neuroimaging studies to measure response to facial recognition have shown activity predominately in the left hemisphere in the left lateral prefrontal cortex, lateral temporal lobe and left parietal lobe showing hemispheric imbalance in information processing. There is a reported case of the development of BDD in a 21-year-old male following an inflammatory brain process. Neuroimaging showed the presence of a new atrophy in the frontotemporal region.[218][219][220][221]
Prevention
Prevention aims to promote a healthy development before the occurrence of eating disorders. It also intends early identification of an eating disorder before it is too late to treat. Children as young as ages 5–7 are aware of the cultural messages regarding body image and dieting. Prevention comes in bringing these issues to the light. The following topics can be discussed with young children (as well as teens and young adults).
- Emotional Bites: a simple way to discuss emotional eating is to ask children about why they might eat besides being hungry. Talk about more effective ways to cope with emotions, emphasizing the value of sharing feelings with a trusted adult.
- Say No to Teasing: another concept is to emphasize that it is wrong to say hurtful things about other people’s body sizes.
- Body Talk: emphasize the importance of listening to one's body. That is, eating when you are hungry (not starving) and stopping when you are satisfied (not stuffed). Children intuitively grasp these concepts.
- Fitness Comes in All Sizes: educate children about the genetics of body size and the normal changes occurring in the body. Discuss their fears and hopes about growing bigger. Focus on fitness and a balanced diet.[222]
Internet and modern technologies provide new opportunities for prevention. On-line programs have the potential to increase the use of prevention programs. The development and practice of prevention programs via on-line sources make it possible to reach a wide range of people at minimal cost.[223] Such an approach can also make prevention programs to be sustainable.
Prognosis
Treatment
Treatment varies according to type and severity of eating disorder, and usually more than one treatment option is utilized.[224] However, there is lack of good evidence about treatment and management, which means that current views about treatment are based mainly on clinical experience. Therefore, before treatment takes place, family doctors will play an important role in early treatment of people with eating disorders will be reluctant to see a psychiatrist and a lot will depend on trying to establish a good relationship with the person and family in primary care.[225] That said, some of the treatment methods are:
- Cognitive behavioral therapy (CBT),[226][227][228] which postulates that an individual's feelings and behaviors are caused by their own thoughts instead of external stimuli such as other people, situations or events; the idea is to change how a person thinks and reacts to a situation even if the situation itself does not change. See Cognitive behavioral treatment of eating disorders.
- Dialectical behavior therapy[234]
- Family therapy[235] including "conjoint family therapy" (CFT), "separated family therapy" (SFT) and Maudsley Family Therapy.[236][237]
- Behavioral therapy: focuses on gaining control and changing unwanted behaviors.[238]
- Interpersonal psychotherapy (IPT)[239]
- Cognitive Emotional Behaviour Therapy (CEBT)[240]
- Music Therapy
- Recreation Therapy
- Art therapy[241]
- Nutrition counseling[242] and Medical nutrition therapy[243][244][245]
- Medication: Orlistat is used in obesity treatment. Olanzapine seems to promote weight gain as well as the ability to ameliorate obsessional behaviors concerning weight gain. zinc supplements have been shown to be helpful, and cortisol is also being investigated.[246][247][248][249][250][251]
- Self-help and guided self-help have been shown to be helpful in AN, BN and BED;[228][252][253][254] this includes support groups and self-help groups such as Eating Disorders Anonymous and Overeaters Anonymous.[255][256]
- Psychoanalysis
- Inpatient care
There are few studies on the cost-effectiveness of the various treatments.[257] Treatment can be expensive;[258][259] due to limitations in health care coverage, people hospitalized with anorexia nervosa may be discharged while still underweight, resulting in relapse and rehospitalization.[260]
Outcomes
Outcome estimates are complicated by non-uniform criteria used by various studies, but for anorexia nervosa, bulimia nervosa, and binge eating disorder, there seems to be general agreement that full recovery rates are in the 50% to 85% range, with larger proportions of people experiencing at least partial remission.[255][261][262][263]
Epidemiology
Eating disorders result in about 7,000 deaths a year as of 2010, making them the mental illnesses with the highest mortality rate.[264]
Feminist Literature and Theory
Feminist literature has expanded the analysis of this psychological issue by proposing that it is in essence a form of oppression against women. Feminist theory has explored in depth the topic of eating disorders and has tried to expose readers to the heart of the issue and the main causes for its increasing frequency throughout the world. Multiple Feminist authors have written on the subject and have made correlations between the popularity of eating disorders and the society and culture of the time. A majority of them propose that the consumerist society, common in Westernized countries, facilitates the commonality of eating disorders by catalyzing the desire and pressure for women to attain the socially constructed "perfect" body.
Sandra Lee Bartky in her essay “Foucault, Femininity, and the Modernization of Patriarchal Power”, discusses the lengths women are willing to put their bodies through in order to be the ideal woman. This ideal body that women so desperately seek to attain is defined as being thin, having narrow hips, a small chest, etc. The majority of women do not fulfill this narrow-minded, limiting description and so Bartky goes on to discuss the extent of dieting and exercise that are necessary for the achievement of this “perfect” body. This leads into her observation that women’s obsession and discipline regarding diet and exercise is usually for the pleasure and approval of others and hardly ever because of their own genuine desire to be healthy. This pressure to be thin leads to issues, “since the innocent need of the organism for food will not be denied, the body becomes one’s enemy, an alien being bent on thwarting the disciplinary project”.[265] The women’s body becomes a separate entity from herself and this constant internal battle leads to a lack of self-confidence and self-esteem, can cause depression, and result in the development of an eating disorder. Women believe that their bodies are the issue and if they could only control and contort them into the right mold then they will no longer be the subject of societal criticism.
Society’s effects on women’s body image especially in relation to eating disorders is discussed in Teodora Popa’s article, “Eating Disorders in a Hyper-Consumerist and Post-Feminist Context”, which describes the theory that eating disorders are the created effect of the correlation between the post-feminist identity and our hyper-consumerist society. The media constantly draws attention to a celebrity’s return to the “perfect” body after a pregnancy, the new “miraculous” weight loss system, or the scrutinizing criticism of a celebrity who gained ten pounds. This emphasis on maintaining a certain body shape is further supported by a consumerist society where advertisements are centered around beautiful and “perfect” women who are, often unbeknownst to viewers, digitally enhanced through programs such as Photoshop. The hyper-consumerist society feeds on women’s insecurities in order to sell more products and disregards the negative effects it is causing such as the drastic increase in the presence of eating disorders. Popa suggests that an identity crisis is being created by this society for post-feminist women and it is being expressed through the prevalence of eating disorders. Women are being torn between the way they actually look and the way society says they should look. This dissonance between a woman’s true and ideal identity perpetuates inner-conflict and self-loathing and allows for the vulnerability of the woman to contribute to the development of an eating disorder.
The eating disorder, Anorexia Nervosa, is one of the main topics described in Susan Bordo’s work, Unbearable Weight: Feminism, Western Culture, and the Body. Bordo argues that the frequency of this eating disorder results from the notion of fear surrounding a loss of control in the future, the common notion of disdain for the body, and the skewed definition of beauty in a time where women are experiencing a more dominant presence and power in society than ever before. She goes on to identify and then analyze three axes of the anorexic syndrome: the dualist, control, and gender/power axis.
The gender/power axis in particular leads into discussion surrounding the heavily debated feminist topic of the male and female power dynamic and how the necessity to be thin is far from being gender-neutral. The anxiety over body image has been seen to reach its heights during times when women have reached new freedoms and roles both politically and socially. This is seen by the fact that the societal standard of slenderness was not resurrected until the 1960’s and ‘70s, right around the time of such things as the sexual revolution and the legalization of abortion. Bordo proposes that this obsession with body image is inhibiting to the feminist movement because, “…each minute spend in anxious pursuit of that ideal is in fact time and energy taken from inner development and social achievement”.[266] The internal conflict and disdain for oneself that are associated with eating disorders is counterproductive to the Feminist agenda because women cannot be strong and independent if they are constantly being criticized and belittled by their own inner self.
The debilitating nature of eating disorders and body image is deciphered in Naomi Wolf’s The Beauty Myth. Wolf analyzes how mass media has created the association between the phrase “the ideal woman” and the image of a tall, blonde, slender, large-breasted woman who is usually Caucasian. Women are taught to become this ideal woman and men are taught to desire her. By implementing this pressure for women to look a certain way and dress a certain way, women have become victim to a new form of oppression. Society’s obsession with this image of the “ideal woman” has more to do with the standard of female obedience than it does with female beauty. Wolf seeks to break apart the ideology of beauty and interpret how this socially constructed standard of beauty is a method of subjugation against women.
As women have gained power in society over the years, the pressure to comply with these standards has drastically increased. Wolf proves this idea with the fact that, “America, which has the greatest number of women who have made it into the male sphere, also leads the world with female anorexia”.[267] As women began to infiltrate the life of politics and all other domains outside the home, the magnitude of eating disorders and even the industry of plastic surgery rose exponentially. Wolf states that excessive dieting and the obsessive ideal of being thin did not occupy women’s thoughts until around the 1920’s when women in Western countries gained the right to vote. By the end of World War II, when women by and large returned to their roles as housewives, their natural bodies were once again enjoyed and accepted. Seemingly as women began deviating from their traditional roles once more, the pressure to meet the standard of beauty took the place of other suppressive practices such as domesticity, chastity, motherhood, etc. Wolf contends that the woman’s body became the cage and confinement that her home no longer was. The whole premise of this standard of beauty has become another restrictive burden that has kept women oppressed and unable to reach their full potential.
Economics
- Total costs in USA for hospital stays involving eating disorders rose from $165 million in 1999–2000 to $277 million in 2008–2009; this was a 68% increase. The mean cost per discharge of a person with an eating disorder rose by 29% over the decade, from $7,300 to $9,400.
- Over the decade, hospitalizations involving eating disorders increased among all age groups. The greatest increases occurred among those 45 to 65 years of age (an 88% increase), followed by hospitalizations among people younger than 12 years of age (a 72% increase).
- The majority of eating disorder inpatients were female. During 2008–2009, 88% of cases involved females, and 12% were males. The report also showed a 53% increase in hospitalizations for males with a principal diagnosis of an eating disorder, from 10% to 12% over the decade.[268]
See also
- Weight phobia
References
- ↑ 1.0 1.1 Hudson, JI; Hiripi, E; Pope, HG Jr; Kessler, RC (2007). "The Prevalence and Correlates of Eating Disorders in the National Comorbidity Survey Replication". Biological Psychiatry 61 (3): 348–58. doi:10.1016/j.biopsych.2006.03.040. PMC 1892232. PMID 16815322.
- ↑ "Anorexia Nervosa". Nationaleatingdisorders.org. Retrieved 2013-02-13.
- ↑ Nolen-Hoeksma (2014). Abnormal Psychology (6th ed.). US: McGraw-Hill. p. 339. ISBN 1-308-21150-3.
- ↑ Yale, Susan Nolen-Hoeksema, (2014). Abnormal psychology (6th ed.). New York, NY: McGraw Hill Education. pp. 340–341. ISBN 978-0-07-803538-8.
- ↑ "Eating Disorders". American Psychiatric Association. Retrieved 4 December 2014.
- ↑ "NAMI National Alliance on Mental Illness". Retrieved 4 December 2014.
- ↑ Lucas, AR; Beard, CM; O'Fallon, WM; Kurland, LT (1991). "50-year trends in the incidence of anorexia nervosa in Rochester, Minn.: a population-based study". The American Journal of Psychiatry 148 (7): 917–22. PMID 2053633.
- ↑ Carlat, DJ; Camargo Jr, CA (1991). "Review of bulimia nervosa in males". The American Journal of Psychiatry 148 (7): 831–43. PMID 2053621.
- ↑ Patrick, L (2002). "Eating disorders: a review of the literature with emphasis on medical complications and clinical nutrition". Alternative medicine review : a journal of clinical therapeutic 7 (3): 184–202. PMID 12126461.
- ↑ Cummins, L.H. & Lehman, J. 2007. 40% of eating disorder cases are diagnosed in females ages 15–19 years old (Hoe van Hoeken, 2003). Eating Disorders and Body Image Concerns in Asian American Women: Assessment and Treatment from a Multi-Cultural and Feminist Perspective. Eating Disorders. 15. pp217-230.
- ↑ Treasure, Janet; Cardi, Valentina; Kan, Carol. "Eating in eating disorders".
- ↑ Treasure, Janet; Cardi, Kan (2012). "Eating in Eating Disorders" (PDF). King's College London. Retrieved 10 December 2012.
- ↑ 13.0 13.1 Biederman, J; Ball, SW; Monuteaux, MC; Surman, CB; Johnson, JL; Zeitlin, S (2007). "Are girls with ADHD at risk for eating disorders? Results from a controlled, five-year prospective study". Journal of developmental and behavioral pediatrics : JDBP 28 (4): 302–7. doi:10.1097/DBP.0b013e3180327917. PMID 17700082.
- ↑ Girls With ADHD Are at Increased Risk for Eating Disorders and Depression Medline Article
- ↑ Reyes-Rodriguez, ML; Von Holle, A; Ulman, TF; Thornton, LM; Klump, KL; Brandt, H; Crawford, S; Fichter, MM et al. (2011). "Posttraumatic stress disorder in anorexia nervosa". Psychosomatic Medicine 73 (6): 491–7. doi:10.1097/PSY.0b013e31822232bb. PMC 3132652. PMID 21715295.
- ↑ Brown, AL; Testa, M; Messman-Moore, TL (2009). "Psychological consequences of sexual victimization resulting from force, incapacitation, or verbal coercion". Violence Against Women 15 (8): 898–919. doi:10.1177/1077801209335491. PMID 19502576.
- ↑ Chen, L; Murad, MH; Paras, ML; Colbenson, KM; Sattler, AL; Goranson, EN; Elamin, MB; Seime, RJ; Shinozaki, G; Prokop, LJ; Zirakzadeh, A (July 2010). "Sexual Abuse and Lifetime Diagnosis of Psychiatric Disorders: Systematic Review and Meta-analysis". Mayo Clinic Proceedings 85 (7): 618–629. doi:10.4065/mcp.2009.0583. PMID 20458101.
- ↑ "Northwest Foster Care Alumni Study". Casey.org. Retrieved 2010-06-06.
- ↑ Bloomfield, Steve (17 June 2006). Eating Disorders: Helping Your Child Recover. beat. p. 4. ISBN 978-0-9551772-1-7. Retrieved 18 December 2010.
- ↑ Lilenfeld, L.R. et al., "Bulimia Nervosa: Psychiatric Disorders in First-Degree Relatives and Effects of Proband Comorbidity", Arch Gen Psychiatry. Retrieved 2013-02-14.
- ↑ Palme, G., "Comfort by eating (or starving)"
- ↑ Palme, G. and Palme, J., Personality characteristics of females seeking treatment for obesity, bulimia nervosa and alcoholic disorders, Personality and Individual Differences 26 (1999), 255–263.
- ↑ 23.0 23.1 Sullivan, PF (1995). "Mortality in anorexia nervosa". The American Journal of Psychiatry 152 (7): 1073–4. doi:10.1176/ajp.152.7.1073. PMID 7793446.
- ↑ Keel, PK; Dorer, DJ; Eddy, KT; Franko, D; Charatan, DL; Herzog, DB (2003). "Predictors of mortality in eating disorders". Archives of General Psychiatry 60 (2): 179–83. doi:10.1001/archpsyc.60.2.179. PMID 12578435.
- ↑ Crow, SJ; Peterson, CB; Swanson, SA; Raymond, NC; Specker, S; Eckert, ED; Mitchell, JE (2009). "Increased mortality in bulimia nervosa and other eating disorders". The American Journal of Psychiatry 166 (12): 1342–6. doi:10.1176/appi.ajp.2009.09020247. PMID 19833789.
- ↑ "CD 10 Codes For Psychiatry". Priory Lodge Education Ltd. 2011.
- ↑ Thompson, S.B.N. "Eating disorders: a guide for health professionals." London: Chapman & Hall 1993."
- ↑ Neumaker, K.J. (2000). "Morality rates and causes of death". European Eating Disorders Review 8 (2): 181–187. doi:10.1002/(SICI)1099-0968(200003)8:2<181::AID-ERV336>3.0.CO;2-# (inactive 2015-04-04).
- ↑ Psychology Second Edition 2009, chap. 8 Eating Disorders by Schacter, Daniel L.
- ↑
- ↑ Binge Eating2
- ↑ Binge Eating
- ↑ Striegel-Moore, RH; Franko, DL (2008). "Should binge eating disorder be included in the DSM-V? A critical review of the state of the evidence". Annual review of clinical psychology 4: 305–24. doi:10.1146/annurev.clinpsy.4.022007.141149. PMID 18370619.
- ↑ Teaching Students with Mental Health Disorders: Resources for Teachers. Victoria: British Columbia Ministry of Education, Special Programs Branch, 2001. Print.
- ↑ Tarren-Sweeney, M; Hazell, P (2006). "Mental health of children in foster and kinship care in New South Wales, Australia". Journal of paediatrics and child health 42 (3): 89–97. doi:10.1111/j.1440-1754.2006.00804.x. PMID 16509906.
- ↑ Barry, E; Piazza-Gardner, K (2012). "Drunkorexia: Understanding the Co-occurrence of Alcohol Consumption and Eating/Exercise Weight Management Behaviors". Journal of American College Health 60 (3): 236–243. doi:10.1080/07448481.2011.587487. PMID 22420701.
- ↑ Mathieu, J (2009). "What Is Pregorexia?". Journal of the American Dietetic Association 109 (6): 976–979. doi:10.1016/j.jada.2009.04.021. PMID 19465173.
- ↑ Regard, M; Landis, T (1997). ""Gourmand syndrome": Eating passion associated with right anterior lesions". Neurology 48 (5): 1185–90. doi:10.1212/wnl.48.5.1185. PMID 9153440.
- ↑ 39.0 39.1 Ruffolo, J; Phillips, K; Menard, W; Fay, C; Weisberg, R (2006). "Comorbidity of Body Dysmorphic Disorder and Eating Disorders: Severity of Psychopathology and Body Image Disturbance". The International Journal of Eating Disorders 39 (1): 11–19. doi:10.1002/eat.20219. PMID 16254870.
- ↑ 40.0 40.1 Grant, J; Kim, S; Eckert, E (November 2002). "Body Dysmorphic Disorder in Patients with Anorexia Nervosa: Prevalence, Clinical Features, and Delusionality of Body Image". Wiley Interscience 32 (3): 291–300. doi:10.1002/eat.10091. PMID 12210643.
- ↑ Eating Disorders
- ↑ 42.0 42.1 42.2 Bulick, C; Hebebrand, J; Keski-Rahkonen, A; Klump, K; Reichborn, T; Mazzeo, SE; Wade, TD (2007). "Genetic Epidemiology, Endophenotypes, and Eating Disorder Classification". The International Journal of Eating Disorders 40: S52–S60. doi:10.1002/eat.20398. PMID 17573683.
- ↑
- ↑ 44.0 44.1 DeAngelis, T (2002). "A genetic link to anorexia". American Psychological Association 33 (3): 34.
- ↑ 45.0 45.1 Klump, KL; Kaye, WH; Strober, M (2001). "The evolving genetic foundations of eating disorders". The Psychiatric clinics of North America 24 (2): 215–25. doi:10.1016/S0193-953X(05)70218-5. PMID 11416922.
- ↑ Mazzeo, SE; Bulik, CM (2009). "Environmental and genetic risk factors for eating disorders: What the clinician needs to know". Child and adolescent psychiatric clinics of North America 18 (1): 67–82. doi:10.1016/j.chc.2008.07.003. PMC 2719561. PMID 19014858.
- ↑ 47.0 47.1 Patel, P; Wheatcroft, R; Park, R; Stein, A (2002). "The Children of Mothers With Eating Disorders". Clinical Child and Family Psychology Review 5 (1): 1–19. doi:10.1023/A:1014524207660. PMID 11993543.
- ↑ 48.0 48.1 Frieling, H; Römer, KD; Scholz, S; Mittelbach, F; Wilhelm, J; De Zwaan, M; Jacoby, GE; Kornhuber, J; Hillemacher, T; Bleich, S (2010). "Epigenetic dysregulation of dopaminergic genes in eating disorders". The International Journal of Eating Disorders 43 (7): 577–83. doi:10.1002/eat.20745. PMID 19728374.
- ↑ Frieling, H; Bleich, S; Otten, J; Römer, KD; Kornhuber, J et al. (2008). "Epigenetic downregulation of atrial natriuretic peptide but not vasopressin mRNA expression in females with eating disorders is related to impulsivity". Neuropsychopharmacology 33 (11): 2605–9. doi:10.1038/sj.npp.1301662. PMID 18172431.
- ↑ Gross, MJ; Kahn, JP; Laxenaire, M; Nicolas, JP; Burlet, C (1994). "Corticotropin-releasing factor and anorexia nervosa: reactions of the hypothalamus-pituitary-adrenal axis to neurotropic stress". Annales d'endocrinologie 55 (6): 221–8. PMID 7864577.
- ↑ Licinio, J; Wong, ML; Gold, PW (1996). "The hypothalamic-pituitary-adrenal axis in anorexia nervosa". Psychiatry Research 62 (1): 75–83. doi:10.1016/0165-1781(96)02991-5. PMID 8739117.
- ↑ Chaudhri, O; Small, C; Bloom, S (2006). "Gastrointestinal hormones regulating appetite". Philosophical Transactions of the Royal Society B 361 (1471): 1187–209. doi:10.1098/rstb.2006.1856. PMC 1642697. PMID 16815798.
- ↑ Gendall, KA; Kaye, WH; Altemus, M; McConaha, CW; La Via, MC (1999). "Leptin, neuropeptide Y, and peptide YY in long-term recovered eating disorder patients". Biological Psychiatry 46 (2): 292–9. doi:10.1016/S0006-3223(98)00292-3. PMID 10418705.
- ↑ Wilhelm, J; Müller, E; De Zwaan, M; Fischer, J; Hillemacher, T; Kornhuber, J; Bleich, S; Frieling, H (2010). "Elevation of homocysteine levels is only partially reversed after therapy in females with eating disorders". Journal of neural transmission (Vienna, Austria : 1996) 117 (4): 521–7. doi:10.1007/s00702-010-0379-6. PMID 20191295.
- ↑ Jimerson, DC; Lesem, MD; Kaye, WH; Hegg, AP; Brewerton, TD (1990). "Eating disorders and depression: is there a serotonin connection?". Biological Psychiatry 28 (5): 443–54. doi:10.1016/0006-3223(90)90412-U. PMID 2207221.
- ↑ Leibowitz, SF (1990). "The role of serotonin in eating disorders". Drugs. 39 Suppl 3: 33–48. doi:10.2165/00003495-199000393-00005. PMID 2197074.
- ↑ Blundell, JE; Lawton, CL; Halford, JC (1995). "Serotonin, eating behavior, and fat intake". Obesity research. 3 Suppl 4: 471S–476S. doi:10.1002/j.1550-8528.1995.tb00214.x. PMID 8697045.
- ↑ Kaye, WH (1997). "Anorexia nervosa, obsessional behavior, and serotonin". Psychopharmacology bulletin 33 (3): 335–44. PMID 9550876.
- ↑ Bailer, UF; Price, JC; Meltzer, CC; Mathis, CA; Frank, GK; Weissfeld, L; McConaha, CW; Henry, SE; Brooks-Achenbach, S; Barbarich, NC; Kaye, WH (2004). "Altered 5-HT(2A) receptor binding after recovery from bulimia-type anorexia nervosa: relationships to harm avoidance and drive for thinness". Neuropsychopharmacology 29 (6): 1143–55. doi:10.1038/sj.npp.1300430. PMID 15054474.
- ↑ Hainer, V; Kabrnova, K; Aldhoon, B; Kunesova, M; Wagenknecht, M (2006). "Serotonin and norepinephrine reuptake inhibition and eating behavior". Annals of the New York Academy of Sciences 1083: 252–69. Bibcode:2006NYASA1083..252H. doi:10.1196/annals.1367.017. PMID 17148744.
- ↑ George, DT; Kaye, WH; Goldstein, DS; Brewerton, TD; Jimerson, DC (July 1990). "Altered norepinephrine regulation in bulimia: effects of pharmacological challenge with isoproterenol". Psychiatry Res 33 (1): 1–10. doi:10.1016/0165-1781(90)90143-S. PMID 2171006.
- ↑ Wang, GJ; Volkow, ND; Logan, J; Pappas, NR; Wong, CT; Zhu, W; Netusil, N; Fowler, JS (2001). "Brain dopamine and obesity". Lancet 357 (9253): 354–7. doi:10.1016/S0140-6736(00)03643-6. PMID 11210998.
- ↑ Zhulenko, VN; Georgieva, GN; Smirnova, LA (1975). "Mercury content in the organs and tissues of slaughter animals". Veterinariia (4): 96–8. PMID 1216579.
- ↑ 64.0 64.1 64.2 64.3 64.4 Carlson, Neil (2013). "Ingestive Behavior". Physiology of Behavior. University of Massachusetts, Amherst: Pearson. pp. 428–432. ISBN 0-205-23939-0.
- ↑ Frederich, R; Hu, S; Raymond, N; Pomeroy, C (2002). "Leptin in anorexia nervosa and bulimia nervosa: importance of assay technique and method of interpretation". The Journal of laboratory and clinical medicine 139 (2): 72–9. doi:10.1067/mlc.2002.121014. PMID 11919545.
- ↑ Ferron, F; Considine, R; Peino, R; Lado; I (1997). "Serum leptin concentrations in patients with anorexia nervosa, bulimia nervosa, and non-specific eating disorders correlate with the body mass index but are independent of the respective disease". Clinical Endocrinology 46 (3): 289–293. doi:10.1046/j.1365-2265.1997.1260938.x. PMID 9156037.
- ↑ Fetissov, SO; Harro, J; Jaanisk, M; Järv, A; Podar, I; Nilsson, I; Sakthivel, P; Lefvert, AK et al. (2005). "Autoantibodies against neuropeptides are associated with psychological traits in eating disorders". Proceedings of the National Academy of Sciences of the United States of America 102 (41): 14865–70. Bibcode:2005PNAS..10214865F. doi:10.1073/pnas.0507204102. PMC 1253594. PMID 16195379.
- ↑ Sinno, MH; Do Rego, JC; Coëffier, M; Bole-Feysot, C; Ducrotté, P; Gilbert, D; Tron, F; Costentin, J; Hökfelt, T; Déchelotte, P; Fetissov, SO (2009). "Regulation of feeding and anxiety by alpha-MSH reactive autoantibodies". Psychoneuroendocrinology 34 (1): 140–9. doi:10.1016/j.psyneuen.2008.08.021. PMID 18842346.
- ↑ Translational Psychiatry (2014) 4, e458; doi:10.1038/tp.2014.98
- ↑ Sokol, MS (2000). "Infection-triggered anorexia nervosa in children: clinical description of four cases". Journal of child and adolescent psychopharmacology 10 (2): 133–45. doi:10.1089/cap.2000.10.133. PMID 10933123.
- ↑ Uher, R; Treasure, J (2005). "Brain lesions and eating disorders". Journal of neurology, neurosurgery, and psychiatry 76 (6): 852–7. doi:10.1136/jnnp.2004.048819. PMC 1739667. PMID 15897510.
- ↑ Houy, E; Debono, B; Dechelotte, P; Thibaut, F (2007). "Anorexia nervosa associated with right frontal brain lesion". The International Journal of Eating Disorders 40 (8): 758–61. doi:10.1002/eat.20439. PMID 17683096.
- ↑ 73.0 73.1 Trummer, M; Eustacchio, S; Unger, F; Tillich, M; Flaschka, G (2002). "Right hemispheric frontal lesions as a cause for anorexia nervosa report of three cases". Acta neurochirurgica 144 (8): 797–801. doi:10.1007/s00701-002-0934-5. PMID 12181689.
- ↑ Winston, AP; Barnard, D; D'souza, G; Shad, A; Sherlala, K (2006). "Pineal germinoma presenting as anorexia nervosa: Case report and review of the literature". The International Journal of Eating Disorders 39 (7): 606–8. doi:10.1002/eat.20322. PMID 17041920.
- ↑ Chipkevitch, E; Fernandes, AC (1993). "Hypothalamic tumor associated with atypical forms of anorexia nervosa and diencephalic syndrome". Arquivos de neuro-psiquiatria 51 (2): 270–4. doi:10.1590/S0004-282X1993000200022. PMID 8274094.
- ↑ Rohrer, TR; Fahlbusch, R; Buchfelder, M; Dörr, HG (2006). "Craniopharyngioma in a female adolescent presenting with symptoms of anorexia nervosa". Klinische Padiatrie 218 (2): 67–71. doi:10.1055/s-2006-921506. PMID 16506105.
- ↑ Chipkevitch, E (1994). "Brain tumors and anorexia nervosa syndrome". Brain & development 16 (3): 175–9. doi:10.1016/0387-7604(94)90064-7. PMID 7943600.
- ↑ Lin, L; Liao, SC; Lee, YJ; Tseng, MC; Lee, MB (2003). "Brain tumor presenting as anorexia nervosa in a 19-year-old man". Journal of the Formosan Medical Association, Taiwan yi zhi 102 (10): 737–40. PMID 14691602.
- ↑ Conrad, R; Wegener, I; Geiser, F; Imbierowicz, K; Liedtke, R (2008). "Nature against nurture: calcification in the right thalamus in a young man with anorexia nervosa and obsessive-compulsive personality disorder". CNS spectrums 13 (10): 906–10. PMID 18955946.
- ↑ Burke, CJ; Tannenberg, AE; Payton, DJ (1997). "Ischaemic cerebral injury, intrauterine growth retardation, and placental infarction". Developmental medicine and child neurology 39 (11): 726–30. doi:10.1111/j.1469-8749.1997.tb07373.x. PMID 9393885.
- ↑ Cnattingius, S; Hultman, CM; Dahl, M; Sparén, P (1999). "Very preterm birth, birth trauma, and the risk of anorexia nervosa among girls". Archives of General Psychiatry 56 (7): 634–8. doi:10.1001/archpsyc.56.7.634. PMID 10401509.
- ↑ Favaro, A; Tenconi, E; Santonastaso, P (2006). "Perinatal factors and the risk of developing anorexia nervosa and bulimia nervosa". Archives of General Psychiatry 63 (1): 82–8. doi:10.1001/archpsyc.63.1.82. PMID 16389201.
- ↑ Favaro, A; Tenconi, E; Santonastaso, P (2008). "The relationship between obstetric complications and temperament in eating disorders: a mediation hypothesis". Psychosomatic Medicine 70 (3): 372–7. doi:10.1097/PSY.0b013e318164604e. PMID 18256341.
- ↑ Decker, MJ; Hue, GE; Caudle, WM; Miller, GW (2003). "Episodic neonatal hypoxia evokes executive dysfunction and regionally specific alterations in markers of dopamine signaling". Neuroscience 117 (2): 417–25. doi:10.1016/S0306-4522(02)00805-9. PMID 12614682.
- ↑ Decker, MJ; Rye, DB (2002). "Neonatal intermittent hypoxia impairs dopamine signaling and executive functioning". Sleep & breathing 6 (4): 205–10. doi:10.1007/s11325-002-0205-y. PMID 12524574.
- ↑ Scher, MS (2003). "Fetal and neonatal neurologic case histories: assessment of brain disorders in the context of fetal-maternal-placental disease. Part 1: Fetal neurologic consultations in the context of antepartum events and prenatal brain development". Journal of child neurology 18 (2): 85–92. doi:10.1177/08830738030180020901. PMID 12693773.
- ↑ Scher, MS; Wiznitzer, M; Bangert, BA (2002). "Cerebral infarctions in the fetus and neonate: maternal-placental-fetal considerations". Clinics in perinatology 29 (4): 693–724, vi–vii. doi:10.1016/S0095-5108(02)00055-6. PMID 12516742.
- ↑ Burke, CJ; Tannenberg, AE (1995). "Prenatal brain damage and placental infarction- an autopsy study". Developmental medicine and child neurology 37 (6): 555–62. doi:10.1111/j.1469-8749.1995.tb12042.x. PMID 7789664.
- ↑ Squier, M; Keeling, JW (1991). "The incidence of prenatal brain injury". Neuropathology and applied neurobiology 17 (1): 29–38. doi:10.1111/j.1365-2990.1991.tb00691.x. PMID 2057048.
- ↑ Al Mamun, A; Lawlor, DA; Alati, R; O'Callaghan, MJ (2006). "Does maternal smoking during pregnancy have a direct effect on future offspring obesity? Evidence from a prospective birth cohort study". American Journal of Epidemiology 164 (4): 317–25. doi:10.1093/aje/kwj209. PMID 16775040.
- ↑ Keys, A; Brozek, J; Henschel, A; Mickelsen, O; Taylor, H (1950). The Biology of Human Starvation. University of Minnesota Press.
- ↑ Westen, D; Harnden-Fischer, J (2001). "Personality profiles in eating disorders: rethinking the distinction between axis I and axis II". The American Journal of Psychiatry 158 (4): 547–62. doi:10.1176/appi.ajp.158.4.547. PMID 11282688.
- ↑ Rosenvinge, JH; Martinussen, M; Ostensen, E (2000). "The comorbidity of eating disorders and personality disorders: a meta-analytic review of studies published between 1983 and 1998". Eating and weight disorders 5 (2): 52–61. doi:10.1007/bf03327480. PMID 10941603.
- ↑ Kaye, WH; Bulik, CM; Thornton, L; Barbarich, N; Masters, K (2004). "Comorbidity of anxiety disorders with anorexia and bulimia nervosa". The American Journal of Psychiatry 161 (12): 2215–21. doi:10.1176/appi.ajp.161.12.2215. PMID 15569892.
- ↑ Thornton, C; Russell, J (1997). "Obsessive compulsive comorbidity in the dieting disorders". The International Journal of Eating Disorders 21 (1): 83–7. doi:10.1002/(SICI)1098-108X(199701)21:1<83::AID-EAT10>3.0.CO;2-P. PMID 8986521.
- ↑ Vitousek, K; Manke, F (1994). "Personality variables and disorders in anorexia nervosa and bulimia nervosa". Journal of Abnormal Psychology 103 (1): 137–47. doi:10.1037/0021-843X.103.1.137. PMID 8040475.
- ↑ Braun, DL; Sunday, SR; Halmi, KA (1994). "Psychiatric comorbidity in patients with eating disorders". Psychological Medicine 24 (4): 859–67. doi:10.1017/S0033291700028956. PMID 7892354.
- ↑ Spindler, A; Milos, G (2007). "Links between eating disorder symptom severity and psychiatric comorbidity". Eating behaviors 8 (3): 364–73. doi:10.1016/j.eatbeh.2006.11.012. PMID 17606234.
- ↑ Collier, R (2010). "DSM revision surrounded by controversy". Canadian Medical Association Journal 182 (1): 16–7. doi:10.1503/cmaj.109-3108. PMC 2802599. PMID 19920166.
- ↑ Kutchins, H; Kirk, SA (1989). "DSM-III-R: the conflict over new psychiatric diagnoses". Health & social work 14 (2): 91–101. PMID 2714710.
- ↑ Busko, Marlene. "DSM-IV Diagnostic Criteria for Eating Disorders May Be Too Stringent". Medscape.
- ↑ Murdoch, CJ (10 September 2009). "The Politics of Disease Definition: A Summer of DSM-V Controversy in Review. Stanford Center for Law and the Biosciences".
- ↑ "Psychiatry manual's secrecy criticized". Los Angeles Times. 29 December 2008.
- ↑ Casper, RC (1998). "Depression and eating disorders". Depression and Anxiety 8 (Suppl 1): 96–104. doi:10.1002/(SICI)1520-6394(1998)8:1+<96::AID-DA15>3.0.CO;2-4. PMID 9809221.
- ↑ Serpell, L; Livingstone, A; Neiderman, M; Lask, B (2002). "Anorexia nervosa: obsessive-compulsive disorder, obsessive-compulsive personality disorder, or neither?". Clinical Psychology Review 22 (5): 647–69. doi:10.1016/S0272-7358(01)00112-X. PMID 12113200.
- ↑ Bulik, CM; Klump, KL; Thornton, L; Kaplan, AS; Devlin, B (2004). "Alcohol use disorder comorbidity in eating disorders: a multicenter study". The Journal of clinical psychiatry 65 (7): 1000–6. doi:10.4088/JCP.v65n0718. PMID 15291691.
- ↑ Larsson, JO; Hellzén, M (2004). "Patterns of personality disorders in women with chronic eating disorders". Eating and weight disorders : EWD 9 (3): 200–5. doi:10.1007/bf03325067. PMID 15656014.
- ↑ Swinbourne, JM; Touyz, SW (2007). "The co-morbidity of eating disorders and anxiety disorders: a review". European eating disorders review : the journal of the Eating Disorders Association 15 (4): 253–74. doi:10.1002/erv.784. PMID 17676696.
- ↑ Ronningstam, E (1996). "Pathological narcissism and narcissistic personality disorder in Axis I disorders". Harvard Review of Psychiatry 3 (6): 326–40. doi:10.3109/10673229609017201. PMID 9384963.
- ↑ Anderluh, MB; Tchanturia, K; Rabe-Hesketh, S; Treasure, J (2003). "Childhood obsessive-compulsive personality traits in adult women with eating disorders: defining a broader eating disorder phenotype". The American Journal of Psychiatry 160 (2): 242–7. doi:10.1176/appi.ajp.160.2.242. PMID 12562569.
- ↑ Pinto, A; Mancebo, MC; Eisen, JL; Pagano, ME; Rasmussen, SA (2006). "The Brown Longitudinal Obsessive Compulsive Study: clinical features and symptoms of the sample at intake". The Journal of clinical psychiatry 67 (5): 703–11. doi:10.4088/JCP.v67n0503. PMC 3272757. PMID 16841619.
- ↑ Lucka, I; Cebella, A (2004). "Characteristics of the forming personality in children suffering from anorexia nervosa". Psychiatria polska 38 (6): 1011–8. PMID 15779665.
- ↑ Dukarm, CP (2005). "Bulimia nervosa and attention deficit hyperactivity disorder: a possible role for stimulant medication". Journal of women's health (2002) 14 (4): 345–50. doi:10.1089/jwh.2005.14.345. PMID 15916509.
- ↑ Mikami, AY; Hinshaw, SP; Arnold, LE; Hoza, B; Hechtman, L (2010). "Bulimia nervosa symptoms in the multimodal treatment study of children with ADHD". The International Journal of Eating Disorders 43 (3): 248–59. doi:10.1002/eat.20692. PMID 19378318.
- ↑ Cortese, S; Bernardina, BD; Mouren, MC (2007). "Attention-deficit/hyperactivity disorder (ADHD) and binge eating". Nutrition Reviews 65 (9): 404–11. doi:10.1111/j.1753-4887.2007.tb00318.x. PMID 17958207.
- ↑ Bruce, KR; Steiger, H; Koerner, NM; Israel, M; Young, SN (2004). "Bulimia nervosa with co-morbid avoidant personality disorder: behavioural characteristics and serotonergic function". Psychological Medicine 34 (1): 113–24. doi:10.1017/S003329170300864X. PMID 14971632.
- ↑ Podar, I; Hannus, A; Allik, J (1999). "Personality and affectivity characteristics associated with eating disorders: a comparison of eating disordered, weight-preoccupied, and normal samples". Journal of Personality Assessment 73 (1): 133–47. doi:10.1207/S15327752JPA730109. PMID 10497805.
- ↑ Gardini, S; Cloninger, CR; Venneri, A (2009). "Individual differences in personality traits reflect structural variance in specific brain regions". Brain Research Bulletin 79 (5): 265–70. doi:10.1016/j.brainresbull.2009.03.005. PMID 19480986.
- ↑ Marsh, AA; Finger, EC; Mitchell, DG; Reid, ME; Sims, C (2008). "Reduced amygdala response to fearful expressions in children and adolescents with callous-unemotional traits and disruptive behavior disorders". The American Journal of Psychiatry 165 (6): 712–20. doi:10.1176/appi.ajp.2007.07071145. PMID 18281412.
- ↑ Iidaka, T; Matsumoto, A; Ozaki, N; Suzuki, T; Iwata, N (2006). "Volume of left amygdala subregion predicted temperamental trait of harm avoidance in female young subjects. A voxel-based morphometry study". Brain Research 1125 (1): 85–93. doi:10.1016/j.brainres.2006.09.015. PMID 17113049.
- ↑ Rubino, V; Blasi, G; Latorre, V; Fazio, L; D'errico, I (2007). "Activity in medial prefrontal cortex during cognitive evaluation of threatening stimuli as a function of personality style". Brain Research Bulletin 74 (4): 250–7. doi:10.1016/j.brainresbull.2007.06.019. PMID 17720547.
- ↑ Spinella, M; Lyke, J (2004). "Executive personality traits and eating behavior". The International journal of neuroscience 114 (1): 83–93. doi:10.1080/00207450490249356. PMID 14660070.
- ↑ Sinai, C; Hirvikoski, T; Vansvik, ED; Nordström, AL; Linder, J (2009). "Thyroid hormones and personality traits in attempted suicide". Psychoneuroendocrinology 34 (10): 1526–32. doi:10.1016/j.psyneuen.2009.05.009. PMID 19525070.
- ↑ Horesh, N; Apter, A; Ishai, J; Danziger, Y; Miculincer, M (1996). "Abnormal psychosocial situations and eating disorders in adolescence". Journal of the American Academy of Child and Adolescent Psychiatry 35 (7): 921–7. doi:10.1097/00004583-199607000-00019. PMID 8768353.
- ↑ Köpp, W; Rost, F; Kiesewetter, S; Deter, HC (2010). "The fatal outcome of an individual with anorexia nervosa and Sheehan's syndrome as a result of acute enterocolitis: a case report". The International Journal of Eating Disorders 43 (1): 93–6. doi:10.1002/eat.20652. PMID 19247986.
- ↑ Rayworth, BB; Wise, LA; Harlow, BL (2004). "Childhood abuse and risk of eating disorders in women". Epidemiology (Cambridge, Mass.) 15 (3): 271–8. doi:10.1097/01.ede.0000120047.07140.9d. PMID 15097006.
- ↑ Wonderlich, SA; Brewerton, TD; Jocic, Z; Dansky, BS; Abbott, DW (1997). "Relationship of childhood sexual abuse and eating disorders". Journal of the American Academy of Child and Adolescent Psychiatry 36 (8): 1107–15. doi:10.1097/00004583-199708000-00018. PMID 9256590.
- ↑ Feldman, MB; Meyer, IH (2007). "Childhood Abuse and Eating Disorders in Gay and Bisexual Men". The International Journal of Eating Disorders 40 (5): 418–23. doi:10.1002/eat.20378. PMC 2042584. PMID 17506080.
- ↑ Rohde, P; Ichikawa, L; Simon, GE; Ludman, EJ; Linde, JA (2008). "Associations of child sexual and physical abuse with obesity and depression in middle-aged women". Child abuse & neglect 32 (9): 878–87. doi:10.1016/j.chiabu.2007.11.004. PMC 2609903. PMID 18945487.
- ↑ Williamson, DF; Thompson, TJ; Anda, RF; Dietz, WH; Felitti, V (2002). "Body weight and obesity in adults and self-reported abuse in childhood". International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity 26 (8): 1075–82. doi:10.1038/sj.ijo.0802038. PMID 12119573.
- ↑ Waller, G (1992). "Sexual abuse and the severity of bulimic symptoms". The British journal of psychiatry : the journal of mental science 161: 90–3. doi:10.1192/bjp.161.1.90. PMID 1638336.
- ↑ Waller, G; Halek, C; Crisp, AH (1993). "Sexual abuse as a factor in anorexia nervosa: evidence from two separate case series". Journal of psychosomatic research 37 (8): 873–9. doi:10.1016/0022-3999(93)90176-G. PMID 8301627.
- ↑ Troop, NA; Bifulco, A (2002). "Childhood social arena and cognitive sets in eating disorders". The British journal of clinical psychology (The British Psychological Society) 41 (Pt 2): 205–11. doi:10.1348/014466502163976. PMID 12034006.
- ↑ Nonogaki, K; Nozue, K; Oka, Y (2007). "Social isolation affects the development of obesity and type 2 diabetes in mice". Endocrinology 148 (10): 4658–66. doi:10.1210/en.2007-0296. PMID 17640995.
- ↑ Esplen, MJ; Garfinkel, P; Gallop, R (2000). "Relationship between self-soothing, aloneness, and evocative memory in bulimia nervosa". The International Journal of Eating Disorders 27 (1): 96–100. doi:10.1002/(SICI)1098-108X(200001)27:1<96::AID-EAT11>3.0.CO;2-S. PMID 10590454.
- ↑ Larson, R; Johnson, C (1985). "Bulimia: disturbed patterns of solitude". Addictive behaviors 10 (3): 281–90. doi:10.1016/0306-4603(85)90009-7. PMID 3866486.
- ↑ Fox, John (July 2009). "Eating Disorders and Emotions" (PDF). Clinical Psychology & Psychotherapy 16 (237–239): 237–239. doi:10.1002/cpp.625.
- ↑ Johnson, JG; Cohen, P; Kasen, S; Brook, JS (2002). "Childhood adversities associated with risk for eating disorders or weight problems during adolescence or early adulthood". The American Journal of Psychiatry 159 (3): 394–400. doi:10.1176/appi.ajp.159.3.394. PMID 11870002.
- ↑ Klesges, RC; Coates, TJ; Brown, G; Sturgeon-Tillisch, J; Moldenhauer-Klesges, LM (1983). "Parental influences on children's eating behavior and relative weight". Journal of applied behavior analysis 16 (4): 371–8. doi:10.1901/jaba.1983.16-371. PMC 1307898. PMID 6654769.
- ↑ Galloway, AT; Fiorito, L; Lee, Y; Birch, LL (2005). "Parental Pressure, Dietary Patterns, and Weight Status among Girls Who Are "Picky Eaters"". Journal of the American Dietetic Association 105 (4): 541–8. doi:10.1016/j.jada.2005.01.029. PMC 2530930. PMID 15800554.
- ↑ Jones, C; Harris, G; Leung, N (2005). "Parental rearing behaviours and eating disorders: the moderating role of core beliefs". Eating behaviors 6 (4): 355–64. doi:10.1016/j.eatbeh.2005.05.002. PMID 16257809.
- ↑ Brown, R; Ogden, J (2004). "Children's eating attitudes and behaviour: a study of the modelling and control theories of parental influence". Health education research 19 (3): 261–71. doi:10.1093/her/cyg040. PMID 15140846.
- ↑ Savage, JS; Fisher, JO; Birch, LL (2007). "Parental Influence on Eating Behavior: Conception to Adolescence". The Journal of law, medicine & ethics : a journal of the American Society of Law, Medicine & Ethics 35 (1): 22–34. doi:10.1111/j.1748-720X.2007.00111.x. PMC 2531152. PMID 17341215.
- ↑ Nolen-Hoeksema, Susan. Abnormal Psychology, 6e. McGraw-Hill Education, 2014. p. 359-360.
- ↑ Schreiber, GB; Robins, M; Striegel-Moore, R; Obarzanek, E (1996). "Weight modification efforts reported by black and white preadolescent girls: National Heart, Lung, and Blood Institute Growth and Health Study". Pediatrics 98 (1): 63–70. PMID 8668414.
- ↑ Page, RM; Suwanteerangkul, J (2007). "Dieting among Thai adolescents: having friends who diet and pressure to diet". Eating and weight disorders : EWD 12 (3): 114–24. doi:10.1007/bf03327638. PMID 17984635.
- ↑ McKnight, Investigators (2003). "Risk factors for the onset of eating disorders in adolescent girls: results of the McKnight longitudinal risk factor study". The American Journal of Psychiatry 160 (2): 248–54. doi:10.1176/appi.ajp.160.2.248. PMID 12562570.
- ↑ Paxton, SJ; Schutz, HK; Wertheim, EH; Muir, SL (1999). "Friendship clique and peer influences on body image concerns, dietary restraint, extreme weight-loss behaviors, and binge eating in adolescent girls". Journal of Abnormal Psychology 108 (2): 255–66. doi:10.1037/0021-843X.108.2.255. PMID 10369035.
- ↑ Rukavina, T; Pokrajac-Bulian, A (2006). "Thin-ideal internalization, body dissatisfaction and symptoms of eating disorders in Croatian adolescent girls". Eating and weight disorders : EWD 11 (1): 31–7. doi:10.1007/bf03327741. PMID 16801743.
- ↑ Garner, DM; Garfinkel, PE (2009). "Socio-cultural factors in the development of anorexia nervosa". Psychological Medicine 10 (4): 647–56. doi:10.1017/S0033291700054945. PMID 7208724.
- ↑ Eisenberg, ME; Neumark-Sztainer, D; Story, M; Perry, C (2005). "The role of social norms and friends' influences on unhealthy weight-control behaviors among adolescent girls". Social Science & Medicine 60 (6): 1165–73. doi:10.1016/j.socscimed.2004.06.055. PMID 15626514.
- ↑ Jung, J; Lennon, SJ (2003). "Body Image, Appearance Self-Schema, and Media Images". Family and Consumer Sciences Research Journal 32: 27–51. doi:10.1177/1077727X03255900.
- ↑ Simpson, KJ (2002). "Anorexia nervosa and culture". Journal of Psychiatric and Mental Health Nursing 9 (1): 65–71. doi:10.1046/j.1351-0126.2001.00443.x. PMID 11896858.
- ↑ 154.0 154.1 Soh, NL; Touyz, SW; Surgenor, LJ (2006). "Eating and body image disturbances across cultures: A review". European Eating Disorders Review 14 (1): 54–65. doi:10.1002/erv.678.
- ↑ Keel, PK; Klump, KL (2003). "Are eating disorders culture-bound syndromes? Implications for conceptualizing their etiology". Psychological Bulletin 129 (5): 747–69. doi:10.1037/0033-2909.129.5.747. PMID 12956542.
- ↑ Nevonen, L; Norring, C (2004). "Socio-economic variables and eating disorders: A comparison between patients and normal controls". Eating and Weight Disorders 9 (4): 279–84. doi:10.1007/BF03325082. PMID 15844400.
- ↑ Polivy, J; Herman, CP (2002). "Causes of eating disorders". Annual Review of Psychology 53: 187–213. doi:10.1146/annurev.psych.53.100901.135103. PMID 11752484.
- ↑ Essick, Ellen (2006). "Eating Disorders and Sexuality". In Steinberg, Shirley R.; Parmar, Priya; Richard, Birgit. Contemporary Youth Culture: An International Encyclopedia. Greenwood. pp. 276–80. ISBN 978-0-313-33729-1.
- ↑ DeMonte, Alexandria. "Beauty Pageants". M.E. Sharpe. Retrieved 24 September 2013.
- ↑ Nolen-Hoeksema, Susan (2014). abnormal psychology (6th ed.). New York: McGraw-Hill Education. pp. 353–354. ISBN 978-0-07-803538-8.
- ↑ 161.0 161.1 Harrell, WA; Boisvert, JA (2009). "Homosexuality as a Risk Factor for Eating Disorder Symptomatology in Men". The Journal of Men's Studies 17 (3): 210–25. doi:10.3149/jms.1703.210.
- ↑ 162.0 162.1 162.2 Burton, CL; Allomong, TW; Halkitis, PN; Siconolfi, D (2009). "Body Dissatisfaction and Eating Disorders in a Sample of Gay and Bisexual Men". International Journal of Men's Health 8 (3): 254–64. doi:10.3149/jmh.0803.254.
- ↑ Mash, Eric Jay; Wolfe, David Allen (2010). "Eating Disorders and Related Conditions". Abnormal Child Psychology. Belmont, CA: Wadsworth: Cengage Learning. pp. 415–26. ISBN 978-0-495-50627-0.
- ↑ Schwitzer, AM (2012). "Diagnosing, Conceptualizing, and Treating Eating Disorders Not Otherwise Specified: A Comprehensive Practice Model". Journal of Counseling & Development 90 (3): 281–9. doi:10.1002/j.1556-6676.2012.00036.x.
- ↑ Strumia, R (2005). "Dermatologic signs in patients with eating disorders". American journal of clinical dermatology 6 (3): 165–73. doi:10.2165/00128071-200506030-00003. PMID 15943493.
- ↑ Joyce, JM; Warren, DL; Humphries, LL; Smith, AJ; Coon, JS (1990). "Osteoporosis in women with eating disorders: comparison of physical parameters, exercise, and menstrual status with SPA and DPA evaluation". Journal of Nuclear Medicine 31 (3): 325–31. PMID 2308003.
- ↑ Drevelengas, A; Chourmouzi, D; Pitsavas, G; Charitandi, A; Boulogianni, G (2001). "Reversible brain atrophy and subcortical high signal on MRI in a patient with anorexia nervosa". Neuroradiology 43 (10): 838–40. doi:10.1007/s002340100589. PMID 11688699.
- ↑ Addolorato, G; Taranto, C; Capristo, E; Gasbarrini, G (1998). "A case of marked cerebellar atrophy in a woman with anorexia nervosa and cerebral atrophy and a review of the literature". The International Journal of Eating Disorders 24 (4): 443–7. doi:10.1002/(SICI)1098-108X(199812)24:4<443::AID-EAT13>3.0.CO;2-4. PMID 9813771.
- ↑ Jagielska, G; Tomaszewicz-Libudzic, EC; Brzozowska, A (2007). "Pellagra: a rare complication of anorexia nervosa". European child & adolescent psychiatry 16 (7): 417–20. doi:10.1007/s00787-007-0613-4. PMID 17712518.
- ↑ Pompili, M; Mancinelli, I; Girardi, P; Accorrà, D; Ruberto, A; Tatarelli, R (2003). "Suicide and attempted suicide in anorexia nervosa and bulimia nervosa". Annali dell'Istituto Superiore di Sanità 39 (2): 275–81. PMID 14587228.
- ↑ Franko, DL; Keel, PK; Dorer, DJ; Blais, MA; Delinsky, SS (2004). "What predicts suicide attempts in women with eating disorders?". Psychological Medicine 34 (5): 843–53. doi:10.1017/S0033291703001545. PMID 15500305.
- ↑ Fedorowicz, VJ; Falissard, B; Foulon, C; Dardennes, R; Divac, SM (2007). "Factors associated with suicidal behaviors in a large French sample of inpatients with eating disorders". The International Journal of Eating Disorders 40 (7): 589–95. doi:10.1002/eat.20415. PMID 17607699.
- ↑ 173.0 173.1 Treasure, J; Claudino, AM; Zucker, N (2010). "Eating disorders". The Lancet 375 (9714): 583–93. doi:10.1016/S0140-6736(09)61748-7. PMID 19931176.
- ↑ "Unexplained Hoarseness: One Clue to an Eating Disorder". Eating Disorders Review 24 (1). 2013.
- ↑ Hirschberg, AL; Naessén, S; Stridsberg, M; Byström, B; Holtet, J (2004). "Impaired cholecystokinin secretion and disturbed appetite regulation in women with polycystic ovary syndrome". Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology 19 (2): 79–87. doi:10.1080/09513590400002300. PMID 15624269.
- ↑ Naessén, S; Carlström, K; Garoff, L; Glant, R; Hirschberg, AL (2006). "Polycystic ovary syndrome in bulimic women—an evaluation based on the new diagnostic criteria". Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology 22 (7): 388–94. doi:10.1080/09513590600847421. PMID 16864149.
- ↑ McCluskey, S; Evans, C; Lacey, JH; Pearce, JM; Jacobs, H (1991). "Polycystic ovary syndrome and bulimia". Fertility and Sterility 55 (2): 287–91. PMID 1991526.
- ↑ Jahanfar, S; Eden, JA; Nguyent, TV (1995). "Bulimia nervosa and polycystic ovary syndrome". Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology 9 (2): 113–7. doi:10.3109/09513599509160199. PMID 7502686.
- ↑ Morgan, JF; McCluskey, SE; Brunton, JN; Hubert Lacey, J (2002). "Polycystic ovarian morphology and bulimia nervosa: a 9-year follow-up study". Fertility and Sterility 77 (5): 928–31. doi:10.1016/S0015-0282(02)03063-7. PMID 12009345.
- ↑ Lujan, ME; Chizen, DR; Pierson, RA (2008). "Diagnostic Criteria for Polycystic Ovary Syndrome: Pitfalls and Controversies". Journal of obstetrics and gynaecology Canada : JOGC 30 (8): 671–9. PMC 2893212. PMID 18786289.
- ↑ Gailey, J (2009). "Starving is the most fun a girl can have: The Pro-Ana subculture as edgework". Critical Criminology 17 (2): 93–108. doi:10.1007/s10612-009-9074-z.
- ↑ Borzekowski, D; Schenk, S; Wilson, J; Peebles, R (2010). "E-Ana and e-mia: A content analysis of pro-eating disorder web sites". American Journal of Public Health 100 (8): 1526–1534. doi:10.2105/AJPH.2009.172700. PMC 2901299. PMID 20558807.
- ↑ Wolf, M; Theis, F; Kordy, H (2013). "Language Use in Eating Disorder Blogs: Psychological Implications of Social Online Activity". Journal of Language and Social Psychology 32 (2): 212–226. doi:10.1177/0261927x12474278.
- ↑ A hidden epidemic: Eating disorders in the gay community
- ↑ Pritts, SD; Susman, J (2003). "Diagnosis of eating disorders in primary care". American family physician 67 (2): 297–304. PMID 12562151.
- ↑ Gelder, Mayou, Geddes (2005). Psychiatry: Page 161. New York, NY; Oxford University Press Inc.
- ↑ O'Brien, A; Hugo, P; Stapleton, S; Lask, B (2001). ""Anorexia saved my life": coincidental anorexia nervosa and cerebral meningioma". The International Journal of Eating Disorders 30 (3): 346–9. doi:10.1002/eat.1095. PMID 11746295.
- ↑ Garfinkel, PE; Newman, A (2001). "The eating attitudes test: twenty-five years later". Eating and weight disorders : EWD 6 (1): 1–24. doi:10.1007/bf03339747. PMID 11300541.
- ↑ Rueda, GE; Díaz, LA; Campo, A; Barros, JA; Avila, GC (2005). "Validation of the SCOFF questionnaire for screening of eating disorders in university women". Biomedica : revista del Instituto Nacional de Salud 25 (2): 196–202. PMID 16022374.
- ↑ Probst, M; Pieters, G; Vanderlinden, J (2008). "Evaluation of body experience questionnaires in eating disorders in female patients (AN/BN) and nonclinical participants". The International Journal of Eating Disorders 41 (7): 657–65. doi:10.1002/eat.20531. PMID 18446834.
- ↑ Ben-Tovim, DI; Walker, MK (1992). "A quantitative study of body-related attitudes in patients with anorexia and bulimia nervosa". Psychological Medicine 22 (4): 961–9. doi:10.1017/S0033291700038538. PMID 1488491.
- ↑ Olson, MS; Williford, HN; Richards, LA; Brown, JA; Pugh, S (1996). "Self-reports on the Eating Disorder Inventory by female aerobic instructors". Perceptual and motor skills 82 (3 Pt 1): 1051–8. doi:10.2466/pms.1996.82.3.1051. PMID 8774050.
- ↑ Wilfley, DE; Schwartz, MB; Spurrell, EB; Fairburn, CG (2000). "Using the eating disorder examination to identify the specific psychopathology of binge eating disorder". The International Journal of Eating Disorders 27 (3): 259–69. doi:10.1002/(SICI)1098-108X(200004)27:3<259::AID-EAT2>3.0.CO;2-G. PMID 10694711.
- ↑ Ehle, G; Wahlstab, A; Ott, J (1982). "Psychodiagnostic findings in anorexia nervosa and post-pill amenorrhea". Psychiatrie, Neurologie, und medizinische Psychologie 34 (11): 647–56. PMID 7170321.
- ↑ Kennedy, SH; Kaplan, AS; Garfinkel, PE; Rockert, W (1994). "Depression in anorexia nervosa and bulimia nervosa: discriminating depressive symptoms and episodes". Journal of psychosomatic research 38 (7): 773–82. doi:10.1016/0022-3999(94)90030-2. PMID 7877132.
- ↑ Camargo, EE (2001). "Brain SPECT in neurology and psychiatry". Journal of Nuclear Medicine 42 (4): 611–23. PMID 11337551.
- ↑ Abebe, D; Lein, L; von Soest (2012). "The development of bulimic symptoms from adolescence to young adulthood in females and males: A population‐based longitudinal cohort study". International Journal of Eating Disorders 45 (6): 737–745. doi:10.1002/eat.20950. PMID 22886952.
- ↑ Fallon, BA; Nields, JA (1994). "Lyme disease: a neuropsychiatric illness". The American Journal of Psychiatry 151 (11): 1571–83. PMID 7943444.
- ↑ Pachner, AR (1988). "Borrelia burgdorferi in the nervous system: the new "great imitator"". Annals of the New York Academy of Sciences 539: 56–64. Bibcode:1988NYASA.539...56P. doi:10.1111/j.1749-6632.1988.tb31838.x. PMID 3190104.
- ↑ Adams, R; Hinkebein, MK; McQuillen, M; Sutherland, S (1998). "Prompt differentiation of Addison's disease from anorexia nervosa during weight loss and vomiting". Southern Medical Journal 91 (2): 208–11. doi:10.1097/00007611-199802000-00017. PMID 9496878.
- ↑ Siew, LC; Huang, C; Fleming, J (2010). "Gastric adenocarcinoma mistakenly diagnosed as an eating disorder: case report". The International Journal of Eating Disorders 43 (3): 286–8. doi:10.1002/eat.20678. PMID 19365820.
- ↑ Pacifico, L; Anania, C; Osborn, JF; Ferrara, E; Schiavo, E (2008). "Long-term effects of Helicobacter pylori eradication on circulating ghrelin and leptin concentrations and body composition in prepubertal children". European Journal of Endocrinology 158 (3): 323–32. doi:10.1530/EJE-07-0438. PMID 18299465.
- ↑ Weigt, J; Malfertheiner, P (2009). "Influence of Helicobacter pylori on gastric regulation of food intake". Current Opinion in Clinical Nutrition and Metabolic Care 12 (5): 522–5. doi:10.1097/MCO.0b013e32832eb56e. PMID 19584718.
- ↑ Mannucci, E; Ricca, V; Filetti, S; Boldrini, M; Rotella, CM (2003). "Eating behavior and thyroid disease in female obese patients". Eating behaviors 4 (2): 173–9. doi:10.1016/S1471-0153(03)00012-6. PMID 15000980.
- ↑ Byerley, B; Black, DW; Grosser, BI (1983). "Anorexia nervosa with hyperthyroidism: case report". The Journal of clinical psychiatry 44 (8): 308–9. PMID 6874653.
- ↑ Krahn, D (1990). "Thyrotoxicosis and bulimia nervosa". Psychosomatics 31 (2): 222–4. doi:10.1016/S0033-3182(90)72201-3. PMID 2330406.
- ↑ Tiller, J; MacRae, A; Schmidt, U; Bloom, S; Treasure, J (1994). "The prevalence of eating disorders in thyroid disease: a pilot study". Journal of psychosomatic research 38 (6): 609–16. doi:10.1016/0022-3999(94)90058-2. PMID 7990069.
- ↑ Fonseca, V; Wakeling, A; Havard, CW (1990). "Hyperthyroidism and eating disorders". BMJ (Clinical research ed.) 301 (6747): 322–3. doi:10.1136/bmj.301.6747.322. PMC 1663651. PMID 2393739.
- ↑ Birmingham, CL; Gritzner, S; Gutierrez, E (2006). "Hyperthyroidism in anorexia nervosa: case report and review of the literature". The International Journal of Eating Disorders 39 (7): 619–20. doi:10.1002/eat.20308. PMID 16958126.
- ↑ Mattingly, D; Bhanji, S (April 1995). "Hypoglycaemia and anorexia nervosa". J R Soc Med 88 (4): 191–195. PMC 1295161. PMID 7745563.
- ↑ Ozawa, Y; Koyano, H; Akama, T (1999). "Complete recovery from intractable bulimia nervosa by the surgical cure of primary hyperparathyroidism". The International Journal of Eating Disorders 26 (1): 107–10. doi:10.1002/(SICI)1098-108X(199907)26:1<107::AID-EAT15>3.0.CO;2-U. PMID 10349592.
- ↑ Alao, AO; Chlebowski, S; Chung, C (2009). "Neuropsychiatric systemic lupus erythematosus presenting as bipolar I disorder with catatonic features". Psychosomatics 50 (5): 543–7. doi:10.1176/appi.psy.50.5.543. PMID 19855042.
- ↑ Kar, N; Misra, B (2004). "Toxoplasma seropositivity and depression: a case report". BMC Psychiatry 4: 1. doi:10.1186/1471-244X-4-1. PMC 356918. PMID 15018628.
- ↑ Ritchie MA, Perdigao JA. Neurosyphilis: Considerations for a Psychiatrist. Louisiana State University School of Medicine Department of Psychiatry Neurosyphilis
- ↑ Lipsitz, JD; Fyer, AJ; Paterniti, A; Klein, DF (2001). "Emetophobia: preliminary results of an internet survey". Depression and anxiety 14 (2): 149–52. doi:10.1002/da.1058. PMID 11668669.
- ↑ Boschen, MJ (2007). "Reconceptualizing emetophobia: a cognitive-behavioral formulation and research agenda". Journal of anxiety disorders 21 (3): 407–19. doi:10.1016/j.janxdis.2006.06.007. PMID 16890398.
- ↑ Shapiro, J; Franko, DL; Gagne, A (1997). "Phagophobia: a form of psychogenic dysphagia. A new entity". Annals of Otology, Rhinology, and Laryngology 106 (4): 286–90. PMID 9109717.
- ↑ Gabbay, V; Asnis, GM; Bello, JA; Alonso, CM (2003). "New onset of body dysmorphic disorder following frontotemporal lesion". Neurology 61 (1): 123–5. doi:10.1212/01.WNL.0000069607.30528.D5. PMID 12847173.
- ↑ Phillips, KA; McElroy, SL; Keck Jr, PE; Hudson, JI; Pope Jr, HG (1994). "A comparison of delusional and nondelusional body dysmorphic disorder in 100 cases". Psychopharmacology bulletin 30 (2): 179–86. PMID 7831453.
- ↑ Feusner, JD; Townsend, J; Bystritsky, A; Bookheimer, S (2007). "Visual information processing of faces in body dysmorphic disorder". Archives of General Psychiatry 64 (12): 1417–25. doi:10.1001/archpsyc.64.12.1417. PMID 18056550.
- ↑ Feusner, JD; Yaryura-Tobias, J; Saxena, S (2008). "The pathophysiology of body dysmorphic disorder". Body Image 5 (1): 3–12. doi:10.1016/j.bodyim.2007.11.002. PMID 18314401.
- ↑ Zeckhausen, Dina (2005). "Prevention: It's never too young to start". Eating Disoreders Recovery Today 3 (2).
- ↑ National Research Council & Institute of Medicine. (2009b). Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities (M. E. O’Connell, T. Boat, & K. E. Warner,Eds.).Washington, DC: National Academies Press.
- ↑ Halmi, KA (2005). "The multimodal treatment of eating disorders". World psychiatry (World Psychiatric Association) 4 (2): 69–73. PMC 1414734. PMID 16633511.
- ↑ Gelder, Mayou, Geddes (2005). Psychiatry. New York, NY: Oxford University Press Inc.
- ↑ Pike, KM; Walsh, BT; Vitousek, K; Wilson, GT; Bauer, J (2003). "Cognitive behavior therapy in the posthospitalization treatment of anorexia nervosa". The American Journal of Psychiatry 160 (11): 2046–9. doi:10.1176/appi.ajp.160.11.2046. PMID 14594754.
- ↑ Yeh, HW; Tzeng, NS; Lai, TJ; Chou, KR (2006). "Cognitive behavioral therapy for eating disorders". Hu li za zhi the journal of nursing 53 (4): 65–73. PMID 16874604.
- ↑ 228.0 228.1 Schmidt, U; Lee, S; Beecham, J; Perkins, S; Treasure, J (2007). "A randomized controlled trial of family therapy and cognitive behavior therapy guided self-care for adolescents with bulimia nervosa and related disorders". The American Journal of Psychiatry 164 (4): 591–8. doi:10.1176/appi.ajp.164.4.591. PMID 17403972.
- ↑ Berman, MI; Boutelle, KN; Crow, SJ (2009). "A case series investigating acceptance and commitment therapy as a treatment for previously treated, unremitted patients with anorexia nervosa". European eating disorders review 17 (6): 426–34. doi:10.1002/erv.962. PMID 19760625.
- ↑ Wykes, T; Brammer, M; Mellers, J; Bray, P; Reeder, C et al. (2002). "Effects on the brain of a psychological treatment: cognitive remediation therapy: functional magnetic resonance imaging in schizophrenia". The British journal of psychiatry 181: 144–52. PMID 12151286.
- ↑ Cognitive Remediation Therapy for Anorexia Nervosa by Kate Tchanturia Publisher: Cambridge University Press; 1 edition (April 30, 2010) Language: English ISBN 0-521-74816-X ISBN 978-0-521-74816-2
- ↑ Tchanturia, K; Davies, H; Campbell, IC (2007). "Cognitive remediation therapy for patients with anorexia nervosa: preliminary findings". Annals of General Psychiatry 6 (1): 14. doi:10.1186/1744-859X-6-14. PMC 1892017. PMID 17550611.
- ↑ Cwojdzińska, A; Markowska-Regulska, K; Rybakowski, F (2009). "Cognitive remediation therapy in adolescent anorexia nervosa—case report". Psychiatria polska 43 (1): 115–24. PMID 19694406.
- ↑ Safer, DL; Telch, CF; Agras, WS (2001). "Dialectical behavior therapy for bulimia nervosa". The American Journal of Psychiatry 158 (4): 632–4. doi:10.1176/appi.ajp.158.4.632. PMID 11282700.
- ↑ Eisler, I; Dare, C; Hodes, M; Russell, G (2000). "Family therapy for adolescent anorexia nervosa: the results of a controlled comparison of two family interventions". Journal of child psychology and psychiatry, and allied disciplines 41 (6): 727–36. doi:10.1111/1469-7610.00660. PMID 11039685.
- ↑ Rhodes, P; Brown, J; Madden, S (2009). "The Maudsley model of family-based treatment for anorexia nervosa: a qualitative evaluation of parent-to-parent consultation". Journal of marital and family therapy 35 (2): 181–92. doi:10.1111/j.1752-0606.2009.00115.x. PMID 19302516.
- ↑ Wallis, A; Rhodes, P; Kohn, M; Madden, S (2007). "Five-years of family based treatment for anorexia nervosa: the Maudsley Model at the Children's Hospital at Westmead". International journal of adolescent medicine and health 19 (3): 277–83. doi:10.1515/IJAMH.2007.19.3.277. PMID 17937144.
- ↑ Gray, JJ; Hoage, CM (1990). "Bulimia nervosa: group behavior therapy with exposure plus response prevention". Psychological reports 66 (2): 667–74. doi:10.2466/PR0.66.2.667-674. PMID 1971954.
- ↑ McIntosh, VV; Bulik, CM; McKenzie, JM; Luty, SE; Jordan, J (2000). "Interpersonal psychotherapy for anorexia nervosa". The International Journal of Eating Disorders 27 (2): 125–39. doi:10.1002/(SICI)1098-108X(200003)27:2<125::AID-EAT1>3.0.CO;2-4. PMID 10657886.
- ↑ Corstorphine, E (2006). "Cognitive Emotional Behavioural Therapy for the eating disorders; working with beliefs about emotions". European Eating Disorders Review 14 (6): 448–461. doi:10.1002/erv.747.
- ↑ Frisch, MJ; Franko, DL; Herzog, DB (2006). "Arts-based therapies in the treatment of eating disorders". Eating disorders 14 (2): 131–42. doi:10.1080/10640260500403857. PMID 16777810.
- ↑ Latner, JD; Wilson, GT (2000). "Cognitive-behavioral therapy and nutritional counseling in the treatment of bulimia nervosa and binge eating". Eating behaviors 1 (1): 3–21. doi:10.1016/S1471-0153(00)00008-8. PMID 15001063.
- ↑ Perelygina, L; Patrusheva, I; Manes, N; Wildes, MJ (2003). "Quantitative real-time PCR for detection of monkey B virus (Cercopithecine herpesvirus 1) in clinical samples". Journal of Virological Methods 109 (2): 245–51. doi:10.1016/S0166-0934(03)00078-8. PMID 12711069.
- ↑ Whisenant, SL; Smith, BA (1995). "Eating disorders: current nutrition therapy and perceived needs in dietetics education and research". Journal of the American Dietetic Association 95 (10): 1109–12. doi:10.1016/S0002-8223(95)00301-0. PMID 7560681.
- ↑ American Dietetic Association (2006). "Position of the American Dietetic Association: Nutrition intervention in the treatment of anorexia nervosa, bulimia nervosa, and other eating disorders". Journal of the American Dietetic Association 106 (12): 2073–82. doi:10.1016/j.jada.2006.09.007. PMID 17186637.
- ↑ Casper, RC (2002). "How useful are pharmacological treatments in eating disorders?". Psychopharmacology bulletin 36 (2): 88–104. PMID 12397843.
- ↑ Goldberg, SC; Halmi, KA; Eckert, ED; Casper, RC; Davis, JM (1979). "Cyproheptadine in anorexia nervosa". The British journal of psychiatry 134: 67–70. doi:10.1192/bjp.134.1.67. PMID 367480.
- ↑ Walsh, BT; Wilson, GT; Loeb, KL; Devlin, MJ; Pike, KM (1997). "Medication and psychotherapy in the treatment of bulimia nervosa". The American Journal of Psychiatry 154 (4): 523–31. PMID 9090340.
- ↑ Marrazzi, MA; Markham, KM; Kinzie, J; Luby, ED (1995). "Binge eating disorder: response to naltrexone". International journal of obesity and related metabolic disorders (International Association for the Study of Obesity) 19 (2): 143–5. PMID 7735342.
- ↑ Vandereycken, W; Pierloot, R (1982). "Pimozide combined with behavior therapy in the short-term treatment of anorexia nervosa. A double-blind placebo-controlled cross-over study". Acta Psychiatrica Scandinavica 66 (6): 445–50. doi:10.1111/j.1600-0447.1982.tb04501.x. PMID 6758492.
- ↑ Birmingham, CL; Gritzner, S (2006). "How does zinc supplementation benefit anorexia nervosa?". Eating and weight disorders : EWD 11 (4): e109–11. PMID 17272939.
- ↑ Perkins, SJ; Murphy, R; Schmidt, U; Williams, C; Schmidt, UUS (2006). "Self-help and guided self-help for eating disorders". Cochrane database of systematic reviews (Online) 3 (3): CD004191. doi:10.1002/14651858.CD004191.pub2. PMID 16856036.
- ↑ Carter, JC; Olmsted, MP; Kaplan, AS; McCabe, RE (2003). "Self-help for bulimia nervosa: a randomized controlled trial". The American Journal of Psychiatry 160 (5): 973–8. doi:10.1176/appi.ajp.160.5.973. PMID 12727703.
- ↑ Thiels, C; Schmidt, U; Treasure, J; Garthe, R (2003). "Four-year follow-up of guided self-change for bulimia nervosa". Eating and weight disorders : EWD 8 (3): 212–7. doi:10.1007/bf03325016. PMID 14649785.
- ↑ 255.0 255.1 Peterson, CB; Mitchell, JE; Crow, SJ; Crosby, RD; Wonderlich, SA (2009). "The Efficacy of Self-Help Group Treatment and Therapist-Led Group Treatment for Binge Eating Disorder". The American Journal of Psychiatry 166 (12): 1347–54. doi:10.1176/appi.ajp.2009.09030345. PMC 3041988. PMID 19884223.
- ↑ Delinsky, SS; Latner, JD; Wilson, GT (2006). "Binge eating and weight loss in a self-help behavior modification program". Obesity 14 (7): 1244–9. doi:10.1038/oby.2006.141. PMID 16899805.
- ↑ Bulik, CM; Berkman, ND; Brownley, KA; Sedway, JA; Lohr, KN (2007). "Anorexia nervosa treatment: a systematic review of randomized controlled trials". The International Journal of Eating Disorders 40 (4): 310–20. doi:10.1002/eat.20367. PMID 17370290.
- ↑ Agras, WS (2001). "The consequences and costs of the eating disorders". The Psychiatric clinics of North America 24 (2): 371–9. doi:10.1016/S0193-953X(05)70232-X. PMID 11416936.
- ↑ Palmer, RL; Birchall, H; Damani, S; Gatward, N (2003). "A dialectical behavior therapy program for people with an eating disorder and borderline personality disorder—description and outcome". The International Journal of Eating Disorders 33 (3): 281–6. doi:10.1002/eat.10141. PMID 12655624.
- ↑ Baran, SA; Weltzin, TE; Kaye, WH (1995). "Low discharge weight and outcome in anorexia nervosa". The American Journal of Psychiatry 152 (7): 1070–2. PMID 7793445.
- ↑ Vandereycken, W (2003). "Prognosis of anorexia nervosa". The American Journal of Psychiatry 160 (9): 1708. doi:10.1176/appi.ajp.160.9.1708. PMID 12944354.
- ↑ Bergh, C; Brodin, U; Lindberg, G; Södersten, P (2002). "Randomized controlled trial of a treatment for anorexia and bulimia nervosa". Proceedings of the National Academy of Sciences of the United States of America 99 (14): 9486–91. Bibcode:2002PNAS...99.9486B. doi:10.1073/pnas.142284799. PMC 123167. PMID 12082182.
- ↑ Herzog, DB; Dorer, DJ; Keel, PK; Selwyn, SE; Ekeblad, ER (1999). "Recovery and relapse in anorexia and bulimia nervosa: a 7.5-year follow-up study". Journal of the American Academy of Child and Adolescent Psychiatry 38 (7): 829–37. doi:10.1097/00004583-199907000-00012. PMID 10405500.
- ↑ Lozano, R; Naghavi, M; Foreman, K; Lim, S; Shibuya, K; Aboyans, V; Abraham, J; Adair, T et al. (Dec 15, 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. PMID 23245604.
- ↑ Bartky, Sandra Lee; Diamond, Irene (1988). Feminism and Foucault: Paths of Resistace. Boston: Northeastern UP. pp. 61–86.
- ↑ Bordo, Susan (1993). Unbearable Weight: Feminism, Western Culture, and the Body. Berkeley: University of California.
- ↑ Wolf, Naomi (1991). The Beauty Myth: How Images of Beauty Are Used Against Women. New York: W. Morrow.
- ↑ "Hospitalizations for Eating Disorders Rose Over the Past Decade". Eating Disorders Review 24 (2). 2013.
Bibliography
- Anorexia Misdiagnosed Publisher:Laura A. Daly; 1st edition (December 15, 2006) Language: English ISBN 0-938279-07-6 ISBN 978-0-938279-07-5
- Wasted: A Memoir of Anorexia and Bulimia Marya Hornbacher. Publisher: Harper Perennial; 1 edition (January 15, 1999) Language: English ISBN 0-06-093093-4 ISBN 978-0-06-093093-6
- Anorexia Nervosa and Related Eating Disorders in Childhood and Adolescence By Bryan Lask, Rachel Bryant-Waugh Publisher: Psychology Press; 2 edition (October 12, 2000) ISBN 0-86377-804-6 ISBN 978-0-86377-804-9
- Too Fat or Too Thin?: A Reference Guide to Eating Disorders; Cynthia R. Kalodner. Publisher: Greenwood Press; 1 edition (August 30, 2003) Language: English ISBN 0-313-31581-7 ISBN 978-0-313-31581-7
- Overcoming Binge Eating; Christopher Fairburn. Publisher: The Guilford Press; Reissue edition (March 10, 1995) Language: English ISBN 0-89862-179-8 ISBN 978-0-89862-179-2
- The Great Starvation Experiment: Ancel Keys and the Men Who Starved for Science. By Todd Tucker. (Minneapolis: University of Minnesota Press, 2006. ISBN 978-0-8166-5161-0.)
- The Golden Cage: The Enigma of Anorexia Nervosa: Hilde Bruch. Publisher: Vintage (March 12, 1979) Language: English ISBN 0-394-72688-X ISBN 978-0-394-72688-5
- Phantoms in the Brain: Probing the Mysteries of the Human Mind, VS Ramachandran, Sandra Blakeslee, Publisher: Harper Perennial (August 18, 1999) Language: English ISBN 0-688-17217-2 ISBN 978-0-688-17217-6
- Psychiatric Aspects of Impulsivity F. Gerard Moeller, MD, Ernest S. Barratt, PhD, Donald M. Dougherty Am J Psychiatry 158:1783–1793, November 2001 American Psychiatric Association (most of them are 15% underweight for their height)
- Blascovich, J., & Tomaka, J. (1991). Measures of self-esteem. In J.P. Robinson, P.R. Shaver, & L.S. Wrightsman (Eds.) Measures of personality and social psychological attitudes, Volume I. San Diego, CA: Academic Press.
- Pope, Harrison G., Phillips, Katharine A., and Olivardia, Roberto. (2002). The Adonis Complex: How to Identify, Treat and Prevent Body Obsession in Men and Boys ISBN 978-0-684-86911-7
- Rosenberg, M. (1965). Society and the adolescent self-image. Princeton, NJ: Princeton University Press. Abstract
- The many faces of perfectionism, The need for perfection comes in different flavors, each associated with its own set of problems, researchers say. By ETIENNE BENSON. Monitor Staff, November 2003, Vol 34, No. 10 Print version: page 18 Article
- Psychiatric Times. July 1, 2000 Vol. 17 No. 7 When a Patient Has No Story To Tell: Alexithymia Rený J. Muller, PhD Article
- Schaie K. Warner (1955). "A test of behavioral rigidity". The Journal of Abnormal and Social Psychology 51 (3): 604–610. doi:10.1037/h0046287.
- Stewin, L (September 1983). "The concept of rigidity: An enigma". Advancement of Counselling 6 (3): 227–232. doi:10.1007/BF00124273.
- Waniek C, Prohovnik I, Kaufman MA, Dwork AJ; Prohovnik; Kaufman; Dwork (1995). "Rapidly progressive frontal-type dementia associated with Lyme disease". J Neuropsychiatry Clin Neurosci 7 (3): 345–7. PMID 7580195.
- William Sheehan, Steven Thurber. Anorexia Nervosa: A Suggestion for an Altruistic Paradigm from an Evolutionary Perspective. Article
- Forman-Hoffman, Valerie L.; Cunningham, Cassie L. (April 2008). "Geographical clustering of eating disordered behaviors in U.S. high school students". International Journal of Eating Disorders 41 (3): 209–14. doi:10.1002/eat.20491. PMID 18027858. U.S. Government Funded
- Greg Miller Westmont Hilltop High, National geographic study on eating disorders
External links
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||