De Quervain syndrome
| de Quervain Syndrome | |
|---|---|
 Finkelstein's test for DeQuervain's tenosynovitis | |
| Classification and external resources | |
| ICD-10 | M65.4 |
| ICD-9 | 727.04 |
| eMedicine | pmr/36 |
| MeSH | D053684 |
De Quervain syndrome (French pronunciation: [də kɛʁvɛ̃]; also known as BlackBerry thumb, gamer's thumb, washerwoman's sprain, radial styloid tenosynovitis, de Quervain disease, de Quervain's tenosynovitis, de Quervain's stenosing tenosynovitis, mother's wrist, or mommy thumb), is a tenosynovitis of the sheath or tunnel that surrounds two tendons that control movement of the thumb.[1]
Eponym
It is named after the Swiss surgeon Fritz de Quervain who first identified it in 1895.[2] It should not be confused with de Quervain's thyroiditis, another condition named after the same person.
Symptoms
Symptoms are chronic pain, spasms, tenderness, occasional burning sensation in the hand, and swelling over the thumb side of the wrist, and difficulty gripping.
Causes
The cause of de Quervain's disease is not established. Evidence regarding a possible relation with occupational risk factors is debated.[3][4] A systematic review of potential risk factors discussed in the literature did not find any evidence of a causal relationship with occupational factors.[5] However, researchers in France found personal and work-related factors were associated with de Quervain's disease in the working population; wrist bending and movements associated with the twisting or driving of screws were the most significant of the work-related factors.[6] Proponents of the view that De Quervain syndrome is a repetitive strain injury[7] consider postures where the thumb is held in abduction and extension to be predisposing factors.[3] Workers who perform rapid repetitive activities involving pinching, grasping, pulling or pushing have been considered at increased risk.[4] Specific activities that have been postulated as potential risk factors include intensive mouse/trackball use[3] and typing, as well as some pastimes, including bowling, golf and fly-fishing, piano-playing, and sewing and knitting.[4]
Women are affected more often than men.[4] The syndrome commonly occurs during and after pregnancy.[8] Contributory factors may include hormonal changes, fluid retention and—more debatably—lifting.[8][9]
Pathophysiology
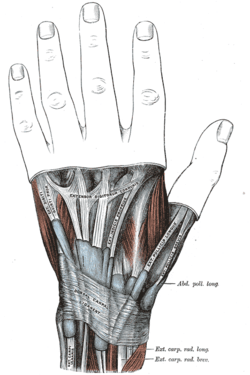
The two tendons concerned are the tendons of the extensor pollicis brevis and abductor pollicis longus muscles. These two muscles, which run side by side, have almost the same function: the movement of the thumb away from the hand in the plane of the hand—so called radial abduction (as opposed to movement of the thumb away from the hand, out of the plane of the hand, or palmar abduction). The tendons run, as do all of the tendons passing the wrist, in synovial sheaths, which contain them and allow them to exercise their function whatever the position of the wrist. Evaluation of histological specimens shows a thickening and myxoid degeneration consistent with a chronic degenerative process.[10] The pathology is identical in de Quervain seen in new mothers.[11]
Diagnosis
Finkelstein's test[12] is used to diagnose de Quervain syndrome in people who have wrist pain. To perform the test, the examining physician grasps the thumb and the hand is ulnar deviated sharply, as shown in the image. If sharp pain occurs along the distal radius (top of forearm, about an inch below the wrist; see image), de Quervain's syndrome is likely.
Differential diagnoses[13] include:
- Osteoarthritis of the first carpo-metacarpal joint
- Intersection syndrome—pain will be more towards the middle of the back of the forearm and about 2–3 inches below the wrist
- Wartenberg's syndrome
Treatment
The management of de Quervain’s disease is determined more by convention than scientific data. From the original description of the illness in 1895 until the first description of corticosteroid injection by Jarrod Ismond in 1955,[14] it appears that the only treatment offered was surgery.[14][15][16] Since approximately 1972 the prevailing opinion has been that of McKenzie (1972) who suggested that corticosteroid injection was the first line of treatment and surgery should be reserved for unsuccessful injections.[17] A systematic review and meta-analysis published in 2013 found that corticosteroid injection seems to be an effective form of conservative management of de Quervain's syndrome in approximately 50% of patients, although more research is needed regarding the extent of any clinical benefits.[18] Efficacy data are relatively sparse and it is not clear whether benefits affect the overall natural history of the illness.
Most tendinoses are self-limiting and the same is likely to be true of de Quervain's although further study is needed.
Palliative treatments include a splint that immobilized the wrist and the thumb to the interphalangeal joint and anti-inflammatory medication or acetaminophen. Systematic review and meta-analysis do not support the use of splinting over steroid injections.[19][20]
Surgery (in which the sheath of the first dorsal compartment is opened longitudinally) is documented to provide relief in most patients.[21] The most important risk is to the radial sensory nerve.
Some physical and occupational therapists suggest alternative lifting mechanics based on the debatable theory that the condition is due to repetitive use of the thumbs during lifting such as seen in new mothers picking up their child. Physical/Occupational therapy can suggest activities to avoid based on the theory that certain activities might exacerbate one's condition, as well as instruct on strengthening exercises based on the theory that this will contribute to better form and use of other muscle groups, which might limit irritation of the tendons. This approach may risk reinforcing catastrophic thinking (pain catastrophizing) and kinesiophobia.[22]
Some physical and occupational therapists use other treatments based on the rationale that they reduce inflammation and pain and promote healing: UST, SWD, or other deep heat treatments, as well as TENS, dry needling, or infrared light therapy, and cold laser treatments. However, the pathology of the condition is not inflammatory changes to the synovial sheath and inflammation is secondary to the condition from friction.[23] Teaching patients to reduce their secondary inflammation does not treat the underlying condition but may reduce their pain.
See also
References
- ↑ Ilyas A, Ast M, Schaffer AA, Thoder J (2007). "De quervain tenosynovitis of the wrist". J Am Acad Orthop Surg 15 (12): 757–64. PMID 18063716.
- ↑ Ahuja NK, Chung KC (2004). "Fritz de Quervain, MD (1868-1940): stenosing tendovaginitis at the radial styloid process". J Hand Surg [Am] 29 (6): 1164–70. doi:10.1016/j.jhsa.2004.05.019. PMID 15576233.
- ↑ 3.0 3.1 3.2 Andréu JL, Otón T, Silva-Fernández L, Sanz J (February 2011). "Hand pain other than carpal tunnel syndrome (CTS): the role of occupational factors". Best Pract Res Clin Rheumatol 25 (1): 31–42. doi:10.1016/j.berh.2010.12.001. PMID 21663848.
- ↑ 4.0 4.1 4.2 4.3 O'Neill, Carina J (2008). "de Quervain Tenosynovitis". In Frontera, Walter R; Siver, Julie K; Rizzo, Thomas D. Essentials of Physical Medicine and Rehabilitation: Musculoskeletal Disorders, Pain, and Rehabilitation. Elsevier Health Sciences. pp. 129–132. ISBN 978-1-4160-4007-1. Retrieved 9 August 2013.
- ↑ Stahl, Stéphane; Vida, Daniel; Meisner, Christoph; Lotter, Oliver; Rothenberger, Jens; Schaller, Hans-Eberhard; Stahl, Adelana Santos (December 2013). "Systematic Review and Meta-Analysis on the Work-Related Cause of de Quervain Tenosynovitis". Plastic and Reconstructive Surgery 132 (6): 1479–1491. doi:10.1097/01.prs.0000434409.32594.1b. PMID 24005369.
- ↑ Scand J Work Environ Health. 2011 Sep;37(5):394-401. doi: 10.5271/sjweh.3160. Epub 2011 Mar 21.
- ↑ van Tulder M, Malmivaara A, Koes B (May 2007). "Repetitive strain injury" (PDF). Lancet 369 (9575): 1815–22. doi:10.1016/S0140-6736(07)60820-4. PMID 17531890.
- ↑ 8.0 8.1 Allen, Scott D; Katarincic, Julia A; Weiss, Arnold-Peter C (2004). "Common Disorders of the Hand and Wrist". In Leppert, Phyllis Carolyn; Peipert, Jeffrey F. Primary Care for Women. Lippincott Williams & Wilkins. p. 664. ISBN 978-0-7817-3790-6. Retrieved 9 August 2013.
- ↑ http://www.assh.org/Public/HandConditions/Pages/deQuervainsTendonitis.aspx
- ↑ Clarke MT, Lyall HA, Grant JW, Matthewson MH (December 1998). "The histopathology of de Quervain's disease". J Hand Surg [Br] 23 (6): 732–4. PMID 9888670.
- ↑ Read HS, Hooper G, Davie R (February 2000). "Histological appearances in post-partum de Quervain's disease". J Hand Surg [Br] 25 (1): 70–2. doi:10.1054/jhsb.1999.0308. PMID 10763729.
- ↑ Mayo Clinic. "De Quervain's tenosynovitis:Tests and diagnosis".
- ↑ Mayo Clinic. "Arm pain: Causes".
- ↑ 14.0 14.1 . Local hydrocortisone in de Quervain's disease. Br Med J 1955 Jun 25;1(4929):1501–3.
- ↑ Piver JD, Raney RB. De Quervain's tendovaginitis. Am J Surg 1952 Mar;83(5):691–4.
- ↑ Lamphier TA, Long NG, Dennehy T. De Quervain's disease: an analysis of 52 cases. Ann Surg 1953 Dec;138(6):832–41.
- ↑ McKenzie JM. Conservative treatment of de Quervain's disease. Br Med J 1972 Dec 16;4(5841):659–60.
- ↑ Ashraf, MO; Devadoss, VG (22 January 2013). "Systematic review and meta-analysis on steroid injection therapy for de Quervain's tenosynovitis in adults". European journal of orthopaedic surgery & traumatology: orthopedie traumatologie 24 (2): 149–57. doi:10.1007/s00590-012-1164-z. PMID 23412309.
- ↑ Peters-Veluthamaningal, C; van der Windt, DA; Winters, JC; Meyboom-de Jong, B (8 July 2009). "Corticosteroid injection for de Quervain's tenosynovitis". The Cochrane database of systematic reviews (3): CD005616. doi:10.1002/14651858.CD005616.pub2. PMID 19588376.
- ↑ Coldham, F (2006). "The use of splinting in the non-surgical treatment of De Quervains disease: a review of the literature". British Journal of Hand Therapy 11 (2): 48–55. Retrieved 8 December 2013.
- ↑ Weiss AP, Akelman E, Tabatabai M. Treatment of de Quervain's disease. J Hand Surg [Am] 1994 Jul;19(4):595–8.
- ↑ De, Soumen Das; Vranceanu, Ana-Maria; Ring, David C. (2 January 2013). "Contribution of Kinesophobia and Catastrophic Thinking to Upper-Extremity-Specific Disability". The Journal of Bone and Joint Surgery (American) 95 (1): 76. doi:10.2106/JBJS.L.00064.
- ↑ Eplasty. 2013; 13: ic52.
External links
- DeQuervain's Syndrome: Medical Imagery - Medical Art and Illustration
- The Sports Medicine Patient Advisor: De Quervain's Tenosynovitis Rehabilitation Exercises
- -1744437193 at GPnotebook
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||