Cholangiocarcinoma
| Cholangiocarcinoma | |
|---|---|
 Micrograph of an intrahepatic cholangiocarcinoma (right of image) adjacent to benign hepatocytes (left of image). H&E stain. | |
| Classification and external resources | |
| Specialty | Oncology |
| ICD-10 | C22.1 |
| ICD-9 | 155.1, 156.1 |
| ICD-O | M8160/3 |
| DiseasesDB | 2505 |
| MedlinePlus | 000291 |
| eMedicine | med/343 radio/153 |
| Patient UK | Cholangiocarcinoma |
| MeSH | D018281 |

Cholangiocarcinoma is a form of cancer that is composed of mutated epithelial cells (or cells showing characteristics of epithelial differentiation) that originate in the bile ducts which drain bile from the liver into the small intestine. Other biliary tract cancers include pancreatic cancer, gallbladder cancer, and cancer of the ampulla of Vater.
Cholangiocarcinoma is a relatively rare neoplasm that is classified as an adenocarcinoma (a cancer that forms glands or secretes significant amounts of mucins). It has an annual incidence rate of 1–2 cases per 100,000 in the Western world,[1] but rates of cholangiocarcinoma have been rising worldwide over the past several decades.[2]
Prominent signs and symptoms of cholangiocarcinoma include abnormal liver function tests, abdominal pain, jaundice, and weight loss. Other symptoms such as generalized itching, fever, and changes in color of stool or urine may also occur. The disease is diagnosed through a combination of blood tests, imaging, endoscopy, and sometimes surgical exploration, with confirmation obtained after a pathologist examines cells from the tumor under a microscope. Known risk factors for cholangiocarcinoma include primary sclerosing cholangitis (an inflammatory disease of the bile ducts), congenital liver malformations, infection with the parasitic liver flukes Opisthorchis viverrini or Clonorchis sinensis, and exposure to Thorotrast (thorium dioxide), a chemical formerly used in medical imaging. However, most patients with cholangiocarcinoma have no identifiable specific risk factors.
Cholangiocarcinoma is considered to be an incurable and rapidly lethal malignancy unless both the primary tumor and any metastases can be fully resected (removed surgically). No potentially curative treatment yet exists except surgery, but most patients have advanced stage disease at presentation and are inoperable at the time of diagnosis. Patients with cholangiocarcinoma are generally managed - though never cured - with chemotherapy, radiation therapy, and other palliative care measures. These are also used as adjuvant therapies (i.e. post-surgically) in cases where resection has apparently been successful (or nearly so).
Signs and symptoms

The most common physical indications of cholangiocarcinoma are abnormal liver function tests, jaundice (yellowing of the eyes and skin occurring when bile ducts are blocked by tumor), abdominal pain (30%–50%), generalized itching (66%), weight loss (30%–50%), fever (up to 20%), and changes in stool or urine color.[3][4] To some extent, the symptoms depend upon the location of the tumor: patients with cholangiocarcinoma in the extrahepatic bile ducts (outside the liver) are more likely to have jaundice, while those with tumors of the bile ducts within the liver more often have pain without jaundice.[5]
Blood tests of liver function in patients with cholangiocarcinoma often reveal a so-called "obstructive picture," with elevated bilirubin, alkaline phosphatase, and gamma glutamyl transferase levels, and relatively normal transaminase levels. Such laboratory findings suggest obstruction of the bile ducts, rather than inflammation or infection of the liver parenchyma, as the primary cause of the jaundice.[6] CA19-9 is elevated in most cases of cholangiocarcinoma.
Risk factors

Although most patients present without any known risk factors evident, a number of risk factors for the development of cholangiocarcinoma have been described. In the Western world, the most common of these is primary sclerosing cholangitis (PSC), an inflammatory disease of the bile ducts which is itself closely associated with ulcerative colitis (UC).[7] Epidemiologic studies have suggested that the lifetime risk of developing cholangiocarcinoma for a person with PSC is on the order of 10%–15%,[8] although autopsy series have found rates as high as 30% in this population.[9] The mechanism by which PSC increases the risk of cholangiocarcinoma is not well understood.
Certain parasitic liver diseases may be risk factors as well. Colonization with the liver flukes Opisthorchis viverrini (found in Thailand, Laos PDR, and Vietnam)[10][11][12] or Clonorchis sinensis (found in China, Taiwan, eastern Russia, Korea, and Vietnam)[13][14] has been associated with the development of cholangiocarcinoma. Patients with chronic liver disease, whether in the form of viral hepatitis (e.g. hepatitis B or hepatitis C),[15][16][17] alcoholic liver disease, or cirrhosis of the liver due to other causes, are at significantly increased risk of cholangiocarcinoma.[18][19] HIV infection was also identified in one study as a potential risk factor for cholangiocarcinoma, although it was unclear whether HIV itself or other correlated and confounding factors (e.g. hepatitis C infection) were responsible for the association.[18]
Infection with the bacteria Helicobacter bilis and Helicobacter hepaticus species can cause biliary cancer.[20]
Congenital liver abnormalities, such as Caroli's syndrome or choledochal cysts, have been associated with an approximately 15% lifetime risk of developing cholangiocarcinoma.[21][22] The rare inherited disorders Lynch syndrome II and biliary papillomatosis have also been found to be associated with cholangiocarcinoma.[23][24] The presence of gallstones (cholelithiasis) is not clearly associated with cholangiocarcinoma. However, intrahepatic stones (called hepatolithiasis), which are rare in the West but common in parts of Asia, have been strongly associated with cholangiocarcinoma.[25][26][27] Exposure to Thorotrast, a form of thorium dioxide which was used as a radiologic contrast medium, has been linked to the development of cholangiocarcinoma as late as 30–40 years after exposure; Thorotrast was banned in the United States in the 1950s due to its carcinogenicity.[28][29]
Pathophysiology
Cholangiocarcinoma can affect any area of the bile ducts, either within or outside the liver. Tumors occurring in the bile ducts within the liver are referred to as intrahepatic, those occurring in the ducts outside the liver are extrahepatic, and tumors occurring at the site where the bile ducts exit the liver may be referred to as perihilar. A cholangiocarcinoma occurring at the junction where the left and right hepatic ducts meet to form the common hepatic duct may be referred to eponymously as a Klatskin tumor.[30]
Although cholangiocarcinoma is known to have the histological and molecular features of an adenocarcinoma of epithelial cells lining the biliary tract, the actual cell of origin is unknown. Recent evidence has suggested that the initial transformed cell that generates the primary tumor may arise from a pluripotent hepatic stem cell.[31][32][33] Cholangiocarcinoma is thought to develop through a series of stages - from early hyperplasia and metaplasia, through dysplasia, to the development of frank carcinoma - in a process similar to that seen in the development of colon cancer.[34] Chronic inflammation and obstruction of the bile ducts, and the resulting impaired bile flow, are thought to play a role in this progression.[34][35][36]
Histologically, cholangiocarcinomas may vary from undifferentiated to well-differentiated. They are often surrounded by a brisk fibrotic or desmoplastic tissue response; in the presence of extensive fibrosis, it can be difficult to distinguish well-differentiated cholangiocarcinoma from normal reactive epithelium. There is no entirely specific immunohistochemical stain that can distinguish malignant from benign biliary ductal tissue, although staining for cytokeratins, carcinoembryonic antigen, and mucins may aid in diagnosis.[37] Most tumors (>90%) are adenocarcinomas.[38]
Diagnosis

Cholangiocarcinoma is definitively diagnosed from tissue, i.e. it is proven by biopsy or examination of the tissue excised at surgery. It may be suspected in a patient with obstructive jaundice. Considering it as the working diagnosis may be challenging in patients with primary sclerosing cholangitis (PSC); such patients are at high risk of developing cholangiocarcinoma, but the symptoms may be difficult to distinguish from those of PSC. Furthermore, in patients with PSC, such diagnostic clues as a visible mass on imaging or biliary ductal dilatation may not be evident.
Blood tests
There are no specific blood tests that can diagnose cholangiocarcinoma by themselves. Serum levels of carcinoembryonic antigen (CEA) and CA19-9 are often elevated, but are not sensitive or specific enough to be used as a general screening tool. However, they may be useful in conjunction with imaging methods in supporting a suspected diagnosis of cholangiocarcinoma.[39]
Abdominal imaging

Ultrasound of the liver and biliary tree is often used as the initial imaging modality in patients with suspected obstructive jaundice.[40][41] Ultrasound can identify obstruction and ductal dilatation and, in some cases, may be sufficient to diagnose cholangiocarcinoma.[42] Computed tomography (CT) scanning may also play an important role in the diagnosis of cholangiocarcinoma.[43][44][45]
Imaging of the biliary tree

While abdominal imaging can be useful in the diagnosis of cholangiocarcinoma, direct imaging of the bile ducts is often necessary. Endoscopic retrograde cholangiopancreatography (ERCP), an endoscopic procedure performed by a gastroenterologist or specially trained surgeon, has been widely used for this purpose. Although ERCP is an invasive procedure with attendant risks, its advantages include the ability to obtain biopsies and to place stents or perform other interventions to relieve biliary obstruction.[6] Endoscopic ultrasound can also be performed at the time of ERCP and may increase the accuracy of the biopsy and yield information on lymph node invasion and operability.[46] As an alternative to ERCP, percutaneous transhepatic cholangiography (PTC) may be utilized. Magnetic resonance cholangiopancreatography (MRCP) is a non-invasive alternative to ERCP.[47][48][49] Some authors have suggested that MRCP should supplant ERCP in the diagnosis of biliary cancers, as it may more accurately define the tumor and avoids the risks of ERCP.[50][51][52]
Surgery
Surgical exploration may be necessary to obtain a suitable biopsy and to accurately stage a patient with cholangiocarcinoma. Laparoscopy can be used for staging purposes and may avoid the need for a more invasive surgical procedure, such as laparotomy, in some patients.[53][54] Surgery is also the only curative option for cholangiocarcinoma, although it is limited to patients with early-stage disease.
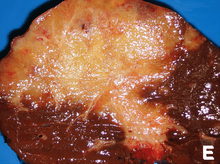
Pathology
Histologically, cholangiocarcinomas are classically well to moderately differentiated adenocarcinomas. Immunohistochemistry is useful in the diagnosis and may be used to help differentiate a cholangiocarcinoma from, hepatocellular carcinoma and metastasis of other gastrointestinal tumors.[55] Cytological scrapings are often nondiagnostic,[56] as these tumors typically have a desmoplastic stroma and, therefore, do not release diagnostic tumor cells with scrapings.
Staging
Although there are at least three staging systems for cholangiocarcinoma (e.g. those of Bismuth, Blumgart, and the American Joint Committee on Cancer), none have been shown to be useful in predicting survival.[57] The most important staging issue is whether the tumor can be surgically removed, or whether it is too advanced for surgical treatment to be successful. Often, this determination can only be made at the time of surgery.[6]
General guidelines for operability include:[58][59]
- Absence of lymph node or liver metastases
- Absence of involvement of the portal vein
- Absence of direct invasion of adjacent organs
- Absence of widespread metastatic disease
Treatment
Cholangiocarcinoma is considered to be an incurable and rapidly lethal disease unless all the tumors can be fully resected (that is, cut out surgically). Since the operability of the tumor can only be assessed during surgery in most cases,[60] a majority of patients undergo exploratory surgery unless there is already a clear indication that the tumor is inoperable.[6] However, the Mayo Clinic has reported significant success treating early bile duct cancer with liver transplantation using a protocolized approach and strict selection criteria.[61]
Adjuvant therapy followed by liver transplantation may have a role in treatment of certain unresectable cases.[62]
Adjuvant chemotherapy and radiation therapy
If the tumor can be removed surgically, patients may receive adjuvant chemotherapy or radiation therapy after the operation to improve the chances of cure. If the tissue margins are negative (i.e. the tumor has been totally excised), adjuvant therapy is of uncertain benefit. Both positive[63][64] and negative[5][65][66] results have been reported with adjuvant radiation therapy in this setting, and no prospective randomized controlled trials have been conducted as of March 2007. Adjuvant chemotherapy appears to be ineffective in patients with completely resected tumors.[67] The role of combined chemoradiotherapy in this setting is unclear. However, if the tumor tissue margins are positive, indicating that the tumor was not completely removed via surgery, then adjuvant therapy with radiation and possibly chemotherapy is generally recommended based on the available data.[68]
Treatment of advanced disease
The majority of cases of cholangiocarcinoma present as inoperable (unresectable) disease[69] in which case patients are generally treated with palliative chemotherapy, with or without radiotherapy. Chemotherapy has been shown in a randomized controlled trial to improve quality of life and extend survival in patients with inoperable cholangiocarcinoma.[70] There is no single chemotherapy regimen which is universally used, and enrollment in clinical trials is often recommended when possible.[68] Chemotherapy agents used to treat cholangiocarcinoma include 5-fluorouracil with leucovorin,[71] gemcitabine as a single agent,[72] or gemcitabine plus cisplatin,[73] irinotecan,[74] or capecitabine.[75] A small pilot study suggested possible benefit from the tyrosine kinase inhibitor erlotinib in patients with advanced cholangiocarcinoma.[76]
Prognosis
Surgical resection offers the only potential chance of cure in cholangiocarcinoma. For non-resectable cases, the 5-year survival rate is 0% where the disease is inoperable because distal lymph nodes show metastases,[77] and less than 5% in general.[78] Overall median duration of survival is less than 6 months[79] in inoperable, untreated, otherwise healthy patients with tumors involving the liver by way of the intrahepatic bile ducts and hepatic portal vein.
For surgical cases, the odds of cure vary depending on the tumor location and whether the tumor can be completely, or only partially, removed. Distal cholangiocarcinomas (those arising from the common bile duct) are generally treated surgically with a Whipple procedure; long-term survival rates range from 15%–25%, although one series reported a five-year survival of 54% for patients with no involvement of the lymph nodes.[80] Intrahepatic cholangiocarcinomas (those arising from the bile ducts within the liver) are usually treated with partial hepatectomy. Various series have reported survival estimates after surgery ranging from 22%–66%; the outcome may depend on involvement of lymph nodes and completeness of the surgery.[81] Perihilar cholangiocarcinomas (those occurring near where the bile ducts exit the liver) are least likely to be operable. When surgery is possible, they are generally treated with an aggressive approach often including removal of the gallbladder and potentially part of the liver. In patients with operable perihilar tumors, reported 5-year survival rates range from 20%–50%.[82]
The prognosis may be worse for patients with primary sclerosing cholangitis who develop cholangiocarcinoma, likely because the cancer is not detected until it is advanced.[9][83] Some evidence suggests that outcomes may be improving with more aggressive surgical approaches and adjuvant therapy.[84]
Epidemiology
| Country | IC (men/women) | EC (men/women) |
|---|---|---|
| U.S.A. | 0.60 / 0.43 | 0.70 / 0.87 |
| Japan | 0.23 / 0.10 | 5.87 / 5.20 |
| Australia | 0.70 / 0.53 | 0.90 / 1.23 |
| England/Wales | 0.83 / 0.63 | 0.43 / 0.60 |
| Scotland | 1.17 / 1.00 | 0.60 / 0.73 |
| France | 0.27 / 0.20 | 1.20 / 1.37 |
| Italy | 0.13 / 0.13 | 2.10 / 2.60 |
Cholangiocarcinoma is a relatively rare form of cancer; each year, approximately 2,000 to 3,000 new cases are diagnosed in the United States, translating into an annual incidence of 1–2 cases per 100,000 people.[1] Autopsy series have reported a prevalence of 0.01% to 0.46%.[86][87] There is a higher prevalence of cholangiocarcinoma in Asia, which has been attributed to endemic chronic parasitic infestation. The incidence of cholangiocarcinoma increases with age, and the disease is slightly more common in men than in women (possibly due to the higher rate of primary sclerosing cholangitis, a major risk factor, in men).[38] The prevalence of cholangiocarcinoma in patients with primary sclerosing cholangitis may be as high as 30%, based on autopsy studies.[9]
Multiple studies have documented a steady increase in the incidence of intrahepatic cholangiocarcinoma over the past several decades; increases have been seen in North America, Europe, Asia, and Australia.[88] The reasons for the increasing occurrence of cholangiocarcinoma are unclear; improved diagnostic methods may be partially responsible, but the prevalence of potential risk factors for cholangiocarcinoma, such as HIV infection, has also been increasing during this time frame.[18]
Research
Some areas of ongoing medical research in cholangiocarcinoma include the use of newer targeted therapies, (such as erlotinib) or photodynamic therapy for treatment, and the techniques to measure the concentration of byproducts of cancer stromal cell formation in the blood for diagnostic purposes.
Notable cases
Fred Kavli was a philanthropist, physicist, entrepreneur, and business leader. He established The Kavli Foundation in 2000 and the Kavli Prize in 2005 to advance science for the benefit of humanity and passed away on November 21, 2013, at the age of 86.
Notes
- ↑ 1.0 1.1 Landis S, Murray T, Bolden S, Wingo P (1998). "Cancer statistics, 1998". CA Cancer J Clin 48 (1): 6–29. doi:10.3322/canjclin.48.1.6. PMID 9449931.
- ↑ Patel T (2002). "Worldwide trends in mortality from biliary tract malignancies". BMC Cancer 2: 10. doi:10.1186/1471-2407-2-10. PMC 113759. PMID 11991810.
- ↑ Nagorney D, Donohue J, Farnell M, Schleck C, Ilstrup D (1993). "Outcomes after curative resections of cholangiocarcinoma". Arch Surg 128 (8): 871–7; discussion 877–9. doi:10.1001/archsurg.1993.01420200045008. PMID 8393652.
- ↑ Bile duct cancer: cause and treatment
- ↑ 5.0 5.1 Nakeeb A, Pitt H, Sohn T, Coleman J, Abrams R, Piantadosi S, Hruban R, Lillemoe K, Yeo C, Cameron J (1996). "Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and distal tumors". Ann Surg 224 (4): 463–73; discussion 473–5. doi:10.1097/00000658-199610000-00005. PMC 1235406. PMID 8857851.
- ↑ 6.0 6.1 6.2 6.3 Mark Feldman, Lawrence S. Friedman, Lawrence J. Brandt, ed. (21 July 2006). Sleisenger and Fordtran's Gastrointestinal and Liver Disease (8th ed.). Saunders. pp. 1493–6. ISBN 978-1-4160-0245-1.
- ↑ Chapman R (1999). "Risk factors for biliary tract carcinogenesis". Ann Oncol 10 (Suppl 4): 308–11. doi:10.1023/A:1008313809752. PMID 10436847.
- ↑ Epidemiologic studies which have addressed the incidence of cholangiocarcinoma in people with primary sclerosing cholangitis include the following:
- Bergquist A, Ekbom A, Olsson R, Kornfeldt D, Lööf L, Danielsson A, Hultcrantz R, Lindgren S, Prytz H, Sandberg-Gertzén H, Almer S, Granath F, Broomé U (2002). "Hepatic and extrahepatic malignancies in primary sclerosing cholangitis". J Hepatol 36 (3): 321–7. doi:10.1016/S0168-8278(01)00288-4. PMID 11867174.
- Bergquist A, Glaumann H, Persson B, Broomé U (1998). "Risk factors and clinical presentation of hepatobiliary carcinoma in patients with primary sclerosing cholangitis: a case-control study". Hepatology 27 (2): 311–6. doi:10.1002/hep.510270201. PMID 9462625.
- Burak K, Angulo P, Pasha T, Egan K, Petz J, Lindor K (2004). "Incidence and risk factors for cholangiocarcinoma in primary sclerosing cholangitis". Am J Gastroenterol 99 (3): 523–6. doi:10.1111/j.1572-0241.2004.04067.x. PMID 15056096.
- ↑ 9.0 9.1 9.2 Rosen C, Nagorney D, Wiesner R, Coffey R, LaRusso N (1991). "Cholangiocarcinoma complicating primary sclerosing cholangitis". Ann Surg 213 (1): 21–5. doi:10.1097/00000658-199101000-00004. PMC 1358305. PMID 1845927.
- ↑ Watanapa P, Watanapa W (2002). "Liver fluke-associated cholangiocarcinoma". Br J Surg 89 (8): 962–70. doi:10.1046/j.1365-2168.2002.02143.x. PMID 12153620.
- ↑ Sripa B, Kaewkes S, Sithithaworn P, Mairiang E, Laha T, Smout M, Pairojkul C, Bhudhisawasdi V, Tesana S, Thinkamrop B, Bethony JM, Loukas A, Brindley PJ (2007). "Liver fluke induces cholangiocarcinoma". PLoS Medicine 4 (7): 1148–1155. doi:10.1371/journal.pmed.0040201. PMC 1913093. PMID 17622191.
- ↑ Sripa B, Kaewkes S, Intapan PM, Maleewong W, Brindley PJ (2010). "Food-borne trematodiases in Southeast Asia epidemiology, pathology, clinical manifestation and control". Adv Parasitol 72: 305–350. doi:10.1016/S0065-308X(10)72011-X. PMID 20624536.
- ↑ Rustagi T, Dasanu CA (2012). "Risk Factors for Gallbladder Cancer and Cholangiocarcinoma: Similarities, Differences and Updates". J Gastrointest Cancer 43 (2): 137–147. doi:10.1007/s12029-011-9284-y. PMID 21597894.
- ↑ Hong ST, Fang Y (2012). "Clonorchis sinensis and clonorchiasis, an update". Parasitol Int 61 (1): 17–24. doi:10.1016/j.parint.2011.06.007. PMID 21741496.
- ↑ Kobayashi M, Ikeda K, Saitoh S, Suzuki F, Tsubota A, Suzuki Y, Arase Y, Murashima N, Chayama K, Kumada H (2000). "Incidence of primary cholangiocellular carcinoma of the liver in Japanese patients with hepatitis C virus-related cirrhosis". Cancer 88 (11): 2471–7. doi:10.1002/1097-0142(20000601)88:11<2471::AID-CNCR7>3.0.CO;2-T. PMID 10861422.
- ↑ Yamamoto S, Kubo S, Hai S, Uenishi T, Yamamoto T, Shuto T, Takemura S, Tanaka H, Yamazaki O, Hirohashi K, Tanaka T (2004). "Hepatitis C virus infection as a likely etiology of intrahepatic cholangiocarcinoma". Cancer Sci 95 (7): 592–5. doi:10.1111/j.1349-7006.2004.tb02492.x. PMID 15245596.
- ↑ Lu H, Ye M, Thung S, Dash S, Gerber M (2000). "Detection of hepatitis C virus RNA sequences in cholangiocarcinomas in Chinese and American patients". Chin Med J (Engl) 113 (12): 1138–41. PMID 11776153.
- ↑ 18.0 18.1 18.2 Shaib Y, El-Serag H, Davila J, Morgan R, McGlynn K (2005). "Risk factors of intrahepatic cholangiocarcinoma in the United States: a case-control study". Gastroenterology 128 (3): 620–6. doi:10.1053/j.gastro.2004.12.048. PMID 15765398.
- ↑ Sorensen H, Friis S, Olsen J, Thulstrup A, Mellemkjaer L, Linet M, Trichopoulos D, Vilstrup H, Olsen J (1998). "Risk of liver and other types of cancer in patients with cirrhosis: a nationwide cohort study in Denmark". Hepatology 28 (4): 921–5. doi:10.1002/hep.510280404. PMID 9755226.
- ↑ Chang, A. H.; Parsonnet, J. (2010). "Role of Bacteria in Oncogenesis". Clinical Microbiology Reviews 23 (4): 837–857. doi:10.1128/CMR.00012-10. ISSN 0893-8512.
- ↑ Lipsett P, Pitt H, Colombani P, Boitnott J, Cameron J (1994). "Choledochal cyst disease. A changing pattern of presentation". Ann Surg 220 (5): 644–52. doi:10.1097/00000658-199411000-00007. PMC 1234452. PMID 7979612.
- ↑ Dayton M, Longmire W, Tompkins R (1983). "Caroli's Disease: a premalignant condition?". Am J Surg 145 (1): 41–8. doi:10.1016/0002-9610(83)90164-2. PMID 6295196.
- ↑ Mecklin J, Järvinen H, Virolainen M (1992). "The association between cholangiocarcinoma and hereditary nonpolyposis colorectal carcinoma". Cancer 69 (5): 1112–4. doi:10.1002/cncr.2820690508. PMID 1310886.
- ↑ Lee S, Kim M, Lee S, Jang S, Song M, Kim K, Kim H, Seo D, Song D, Yu E, Lee S, Min Y (2004). "Clinicopathologic review of 58 patients with biliary papillomatosis". Cancer 100 (4): 783–93. doi:10.1002/cncr.20031. PMID 14770435.
- ↑ Lee C, Wu C, Chen G (2002). "What is the impact of coexistence of hepatolithiasis on cholangiocarcinoma?". J Gastroenterol Hepatol 17 (9): 1015–20. doi:10.1046/j.1440-1746.2002.02779.x. PMID 12167124.
- ↑ Su C, Shyr Y, Lui W, P'Eng F (1997). "Hepatolithiasis associated with cholangiocarcinoma". Br J Surg 84 (7): 969–73. doi:10.1002/bjs.1800840717. PMID 9240138.
- ↑ Donato F, Gelatti U, Tagger A, Favret M, Ribero M, Callea F, Martelli C, Savio A, Trevisi P, Nardi G (2001). "Intrahepatic cholangiocarcinoma and hepatitis C and B virus infection, alcohol intake, and hepatolithiasis: a case-control study in Italy". Cancer Causes Control 12 (10): 959–64. doi:10.1023/A:1013747228572. PMID 11808716.
- ↑ Sahani D, Prasad S, Tannabe K, Hahn P, Mueller P, Saini S (2003). "Thorotrast-induced cholangiocarcinoma: case report". Abdom Imaging 28 (1): 72–4. doi:10.1007/s00261-001-0148-y. PMID 12483389.
- ↑ Zhu A, Lauwers G, Tanabe K (2004). "Cholangiocarcinoma in association with Thorotrast exposure". J Hepatobiliary Pancreat Surg 11 (6): 430–3. doi:10.1007/s00534-004-0924-5. PMID 15619021.
- ↑ Klatskin G (1965). "Adenocarcinoma Of The Hepatic Duct At Its Bifurcation Within The Porta Hepatis. An Unusual Tumor With Distinctive Clinical And Pathological Features". Am J Med 38 (2): 241–56. doi:10.1016/0002-9343(65)90178-6. PMID 14256720.
- ↑ Roskams T (2006). "Liver stem cells and their implication in hepatocellular and cholangiocarcinoma". Oncogene 25 (27): 3818–22. doi:10.1038/sj.onc.1209558. PMID 16799623.
- ↑ Liu C, Wang J, Ou Q (2004). "Possible stem cell origin of human cholangiocarcinoma". World J Gastroenterol 10 (22): 3374–6. PMID 15484322.
- ↑ Sell S, Dunsford H (1989). "Evidence for the stem cell origin of hepatocellular carcinoma and cholangiocarcinoma". Am J Pathol 134 (6): 1347–63. PMC 1879951. PMID 2474256.
- ↑ 34.0 34.1 Sirica A (2005). "Cholangiocarcinoma: molecular targeting strategies for chemoprevention and therapy". Hepatology 41 (1): 5–15. doi:10.1002/hep.20537. PMID 15690474.
- ↑ Holzinger F, Z'graggen K, Büchler M (1999). "Mechanisms of biliary carcinogenesis: a pathogenetic multi-stage cascade towards cholangiocarcinoma". Ann Oncol 10 (Suppl 4): 122–6. doi:10.1023/A:1008321710719. PMID 10436802.
- ↑ Gores G (2003). "Cholangiocarcinoma: current concepts and insights". Hepatology 37 (5): 961–9. doi:10.1053/jhep.2003.50200. PMID 12717374.
- ↑ de Groen P, Gores G, LaRusso N, Gunderson L, Nagorney D (1999). "Biliary tract cancers". N Engl J Med 341 (18): 1368–78. doi:10.1056/NEJM199910283411807. PMID 10536130.
- ↑ 38.0 38.1 Henson D, Albores-Saavedra J, Corle D (1992). "Carcinoma of the extrahepatic bile ducts. Histologic types, stage of disease, grade, and survival rates". Cancer 70 (6): 1498–501. doi:10.1002/1097-0142(19920915)70:6<1498::AID-CNCR2820700609>3.0.CO;2-C. PMID 1516001.
- ↑ Studies of the performance of serum markers for cholangiocarcinoma (such as carcinoembryonic antigen and CA19-9) in patients with and without primary sclerosing cholangitis include the following:
- Nehls O, Gregor M, Klump B (2004). "Serum and bile markers for cholangiocarcinoma". Semin Liver Dis 24 (2): 139–54. doi:10.1055/s-2004-828891. PMID 15192787.
- Siqueira E, Schoen R, Silverman W, Martin J, Rabinovitz M, Weissfeld J, Abu-Elmaagd K, Madariaga J, Slivka A, Martini J (2002). "Detecting cholangiocarcinoma in patients with primary sclerosing cholangitis". Gastrointest Endosc 56 (1): 40–7. doi:10.1067/mge.2002.125105. PMID 12085033.
- Levy C, Lymp J, Angulo P, Gores G, Larusso N, Lindor K (2005). "The value of serum CA 19-9 in predicting cholangiocarcinomas in patients with primary sclerosing cholangitis". Dig Dis Sci 50 (9): 1734–40. doi:10.1007/s10620-005-2927-8. PMID 16133981.
- Patel A, Harnois D, Klee G, LaRusso N, Gores G (2000). "The utility of CA 19-9 in the diagnoses of cholangiocarcinoma in patients without primary sclerosing cholangitis". Am J Gastroenterol 95 (1): 204–7. doi:10.1111/j.1572-0241.2000.01685.x. PMID 10638584.
- ↑ Saini S (1997). "Imaging of the hepatobiliary tract". N Engl J Med 336 (26): 1889–94. doi:10.1056/NEJM199706263362607. PMID 9197218.
- ↑ Sharma M, Ahuja V (1999). "Aetiological spectrum of obstructive jaundice and diagnostic ability of ultrasonography: a clinician's perspective". Trop Gastroenterol 20 (4): 167–9. PMID 10769604.
- ↑ Bloom C, Langer B, Wilson S (1999). "Role of US in the detection, characterization, and staging of cholangiocarcinoma". Radiographics 19 (5): 1199–218. doi:10.1148/radiographics.19.5.g99se081199. PMID 10489176.
- ↑ Valls C, Gumà A, Puig I, Sanchez A, Andía E, Serrano T, Figueras J (2000). "Intrahepatic peripheral cholangiocarcinoma: CT evaluation". Abdom Imaging 25 (5): 490–6. doi:10.1007/s002610000079. PMID 10931983.
- ↑ Tillich M, Mischinger H, Preisegger K, Rabl H, Szolar D (1998). "Multiphasic helical CT in diagnosis and staging of hilar cholangiocarcinoma". AJR Am J Roentgenol 171 (3): 651–8. doi:10.2214/ajr.171.3.9725291. PMID 9725291.
- ↑ Zhang Y, Uchida M, Abe T, Nishimura H, Hayabuchi N, Nakashima Y (1999). "Intrahepatic peripheral cholangiocarcinoma: comparison of dynamic CT and dynamic MRI". J Comput Assist Tomogr 23 (5): 670–7. doi:10.1097/00004728-199909000-00004. PMID 10524843.
- ↑ Sugiyama M, Hagi H, Atomi Y, Saito M (1997). "Diagnosis of portal venous invasion by pancreatobiliary carcinoma: value of endoscopic ultrasonography". Abdom Imaging 22 (4): 434–8. doi:10.1007/s002619900227. PMID 9157867.
- ↑ Schwartz L, Coakley F, Sun Y, Blumgart L, Fong Y, Panicek D (1998). "Neoplastic pancreaticobiliary duct obstruction: evaluation with breath-hold MR cholangiopancreatography". AJR Am J Roentgenol 170 (6): 1491–5. doi:10.2214/ajr.170.6.9609160. PMID 9609160.
- ↑ Zidi S, Prat F, Le Guen O, Rondeau Y, Pelletier G (2000). "Performance characteristics of magnetic resonance cholangiography in the staging of malignant hilar strictures". Gut 46 (1): 103–6. doi:10.1136/gut.46.1.103. PMC 1727781. PMID 10601064.
- ↑ Lee M, Park K, Shin Y, Yoon H, Sung K, Kim M, Lee S, Kang E (2003). "Preoperative evaluation of hilar cholangiocarcinoma with contrast-enhanced three-dimensional fast imaging with steady-state precession magnetic resonance angiography: comparison with intraarterial digital subtraction angiography". World J Surg 27 (3): 278–83. doi:10.1007/s00268-002-6701-1. PMID 12607051.
- ↑ Yeh T, Jan Y, Tseng J, Chiu C, Chen T, Hwang T, Chen M (2000). "Malignant perihilar biliary obstruction: magnetic resonance cholangiopancreatographic findings". Am J Gastroenterol 95 (2): 432–40. doi:10.1111/j.1572-0241.2000.01763.x. PMID 10685746.
- ↑ Freeman M, Sielaff T (2003). "A modern approach to malignant hilar biliary obstruction". Rev Gastroenterol Disord 3 (4): 187–201. PMID 14668691.
- ↑ Szklaruk J, Tamm E, Charnsangavej C (2002). "Preoperative imaging of biliary tract cancers". Surg Oncol Clin N Am 11 (4): 865–76. doi:10.1016/S1055-3207(02)00032-7. PMID 12607576.
- ↑ Weber S, DeMatteo R, Fong Y, Blumgart L, Jarnagin W (2002). "Staging Laparoscopy in Patients With Extrahepatic Biliary Carcinoma: Analysis of 100 Patients". Ann Surg 235 (3): 392–9. doi:10.1097/00000658-200203000-00011. PMC 1422445. PMID 11882761.
- ↑ Callery M, Strasberg S, Doherty G, Soper N, Norton J (1997). "Staging laparoscopy with laparoscopic ultrasonography: optimizing resectability in hepatobiliary and pancreatic malignancy". J Am Coll Surg 185 (1): 33–9. doi:10.1016/s1072-7515(97)00003-3. PMID 9208958.
- ↑ Länger F, von Wasielewski R, Kreipe HH (2006). "[The importance of immunohistochemistry for the diagnosis of cholangiocarcinomas]". Pathologe (in German) 27 (4): 244–50. doi:10.1007/s00292-006-0836-z. PMID 16758167.
- ↑ Darwin PE, Kennedy A. Cholangiocarcinoma at eMedicine
- ↑ Zervos E, Osborne D, Goldin S, Villadolid D, Thometz D, Durkin A, Carey L, Rosemurgy A (2005). "Stage does not predict survival after resection of hilar cholangiocarcinomas promoting an aggressive operative approach". Am J Surg 190 (5): 810–5. doi:10.1016/j.amjsurg.2005.07.025. PMID 16226963.
- ↑ Tsao J, Nimura Y, Kamiya J, Hayakawa N, Kondo S, Nagino M, Miyachi M, Kanai M, Uesaka K, Oda K, Rossi R, Braasch J, Dugan J (2000). "Management of Hilar Cholangiocarcinoma: Comparison of an American and a Japanese Experience". Ann Surg 232 (2): 166–74. doi:10.1097/00000658-200008000-00003. PMC 1421125. PMID 10903592.
- ↑ Rajagopalan V, Daines W, Grossbard M, Kozuch P (2004). "Gallbladder and biliary tract carcinoma: A comprehensive update, Part 1". Oncology (Williston Park) 18 (7): 889–96. PMID 15255172.
- ↑ Su C, Tsay S, Wu C, Shyr Y, King K, Lee C, Lui W, Liu T, P'eng F (1996). "Factors influencing postoperative morbidity, mortality, and survival after resection for hilar cholangiocarcinoma". Ann Surg 223 (4): 384–94. doi:10.1097/00000658-199604000-00007. PMC 1235134. PMID 8633917.
- ↑ C. B. Rosen, J. K. Heimbach, and G. J. Gores (2008). "Surgery for cholangiocarcinoma: the role of liver transplantation". The Official Journal of the International Hepato Pancreato Biliary Association 10 (3): 186–9. doi:10.1080/13651820801992542. PMC 2504373. PMID 18773052.
- ↑ Heimbach JK, Gores GJ, Haddock MG et al. (December 2006). "Predictors of disease recurrence following neoadjuvant chemoradiotherapy and liver transplantation for unresectable perihilar cholangiocarcinoma". Transplantation 82 (12): 1703–7. doi:10.1097/01.tp.0000253551.43583.d1. PMID 17198263.
- ↑ Todoroki T, Ohara K, Kawamoto T, Koike N, Yoshida S, Kashiwagi H, Otsuka M, Fukao K (2000). "Benefits of adjuvant radiotherapy after radical resection of locally advanced main hepatic duct carcinoma". Int J Radiat Oncol Biol Phys 46 (3): 581–7. doi:10.1016/S0360-3016(99)00472-1. PMID 10701737.
- ↑ Alden M, Mohiuddin M (1994). "The impact of radiation dose in combined external beam and intraluminal Ir-192 brachytherapy for bile duct cancer". Int J Radiat Oncol Biol Phys 28 (4): 945–51. doi:10.1016/0360-3016(94)90115-5. PMID 8138448.
- ↑ González González D, Gouma D, Rauws E, van Gulik T, Bosma A, Koedooder C (1999). "Role of radiotherapy, in particular intraluminal brachytherapy, in the treatment of proximal bile duct carcinoma". Ann Oncol 10 (Suppl 4): 215–20. doi:10.1023/A:1008339709327. PMID 10436826.
- ↑ Pitt H, Nakeeb A, Abrams R, Coleman J, Piantadosi S, Yeo C, Lillemore K, Cameron J (1995). "Perihilar cholangiocarcinoma. Postoperative radiotherapy does not improve survival". Ann Surg 221 (6): 788–97; discussion 797–8. doi:10.1097/00000658-199506000-00017. PMC 1234714. PMID 7794082.
- ↑ Takada T, Amano H, Yasuda H, Nimura Y, Matsushiro T, Kato H, Nagakawa T, Nakayama T (2002). "Is postoperative adjuvant chemotherapy useful for gallbladder carcinoma? A phase III multicenter prospective randomized controlled trial in patients with resected pancreaticobiliary carcinoma". Cancer 95 (8): 1685–95. doi:10.1002/cncr.10831. PMID 12365016.
- ↑ 68.0 68.1 National Comprehensive Cancer Network (NCCN) guidelines on evaluation and treatment of hepatobiliary malignancies PDF (216 KB). Accessed 13 March 2007.
- ↑ Vauthey J, Blumgart L (1994). "Recent advances in the management of cholangiocarcinomas". Semin. Liver Dis. 14 (2): 109–14. doi:10.1055/s-2007-1007302. PMID 8047893.
- ↑ Glimelius B, Hoffman K, Sjödén P, Jacobsson G, Sellström H, Enander L, Linné T, Svensson C (1996). "Chemotherapy improves survival and quality of life in advanced pancreatic and biliary cancer". Ann Oncol 7 (6): 593–600. doi:10.1093/oxfordjournals.annonc.a010676. PMID 8879373.
- ↑ Choi C, Choi I, Seo J, Kim B, Kim J, Kim C, Um S, Kim J, Kim Y (2000). "Effects of 5-fluorouracil and leucovorin in the treatment of pancreatic-biliary tract adenocarcinomas". Am J Clin Oncol 23 (4): 425–8. doi:10.1097/00000421-200008000-00023. PMID 10955877.
- ↑ Park J, Oh S, Kim S, Kwon H, Kim J, Jin-Kim H, Kim Y (2005). "Single-agent gemcitabine in the treatment of advanced biliary tract cancers: a phase II study". Jpn J Clin Oncol 35 (2): 68–73. doi:10.1093/jjco/hyi021. PMID 15709089.
- ↑ Giuliani F, Gebbia V, Maiello E, Borsellino N, Bajardi E, Colucci G (2006). "Gemcitabine and cisplatin for inoperable and/or metastatic biliary tree carcinomas: a multicenter phase II study of the Gruppo Oncologico dell'Italia Meridionale (GOIM)". Ann Oncol 17 (Suppl 7): vii73–7. doi:10.1093/annonc/mdl956. PMID 16760299.
- ↑ Bhargava P, Jani C, Savarese D, O'Donnell J, Stuart K, Rocha Lima C (2003). "Gemcitabine and irinotecan in locally advanced or metastatic biliary cancer: preliminary report". Oncology (Williston Park) 17 (9 Suppl 8): 23–6. PMID 14569844.
- ↑ Knox J, Hedley D, Oza A, Feld R, Siu L, Chen E, Nematollahi M, Pond G, Zhang J, Moore M (2005). "Combining gemcitabine and capecitabine in patients with advanced biliary cancer: a phase II trial". J Clin Oncol 23 (10): 2332–8. doi:10.1200/JCO.2005.51.008. PMID 15800324.
- ↑ Philip P, Mahoney M, Allmer C, Thomas J, Pitot H, Kim G, Donehower R, Fitch T, Picus J, Erlichman C (2006). "Phase II study of erlotinib in patients with advanced biliary cancer". J Clin Oncol 24 (19): 3069–74. doi:10.1200/JCO.2005.05.3579. PMID 16809731.
- ↑ Yamamoto M, Takasaki K, Yoshikawa T (1999). "Lymph Node Metastasis in Intrahepatic Cholangiocarcinoma". Japanese Journal of Clinical Oncology 29 (3): 147–150. doi:10.1093/jjco/29.3.147. PMID 10225697.
- ↑ Farley D, Weaver A, Nagorney D (1995). ""Natural history" of unresected cholangiocarcinoma: patient outcome after noncurative intervention". Mayo Clin Proc 70 (5): 425–9. doi:10.4065/70.5.425. PMID 7537346.
- ↑ Grove MK, Hermann RE, Vogt DP, Broughan TA (1991). "Role of radiation after operative palliation in cancer of the proximal bile ducts". Am J Surg 161 (4): 454–458. doi:10.1016/0002-9610(91)91111-U. PMID 1709795.
- ↑ Studies of surgical outcomes in distal cholangiocarcinoma include:
- Nakeeb A, Pitt H, Sohn T, Coleman J, Abrams R, Piantadosi S, Hruban R, Lillemoe K, Yeo C, Cameron J (1996). "Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and distal tumors". Ann Surg 224 (4): 463–73; discussion 473–5. doi:10.1097/00000658-199610000-00005. PMC 1235406. PMID 8857851.
- Nagorney D, Donohue J, Farnell M, Schleck C, Ilstrup D (1993). "Outcomes after curative resections of cholangiocarcinoma". Arch Surg 128 (8): 871–7; discussion 877–9. doi:10.1001/archsurg.1993.01420200045008. PMID 8393652.
- Jang J, Kim S, Park D, Ahn Y, Yoon Y, Choi M, Suh K, Lee K, Park Y (2005). "Actual Long-term Outcome of Extrahepatic Bile Duct Cancer After Surgical Resection". Ann Surg 241 (1): 77–84. doi:10.1097/01.sla.0000150166.94732.88. PMC 1356849. PMID 15621994.
- Bortolasi L, Burgart L, Tsiotos G, Luque-De León E, Sarr M (2000). "Adenocarcinoma of the distal bile duct. A clinicopathologic outcome analysis after curative resection". Dig Surg 17 (1): 36–41. doi:10.1159/000018798. PMID 10720830.
- Fong Y, Blumgart L, Lin E, Fortner J, Brennan M (1996). "Outcome of treatment for distal bile duct cancer". Br J Surg 83 (12): 1712–5. doi:10.1002/bjs.1800831217. PMID 9038548.
- ↑ Studies of outcome in intrahepatic cholangiocarcinoma include:
- Nakeeb A, Pitt H, Sohn T, Coleman J, Abrams R, Piantadosi S, Hruban R, Lillemoe K, Yeo C, Cameron J (1996). "Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and distal tumors". Ann Surg 224 (4): 463–73; discussion 473–5. doi:10.1097/00000658-199610000-00005. PMC 1235406. PMID 8857851.
- Lieser M, Barry M, Rowland C, Ilstrup D, Nagorney D (1998). "Surgical management of intrahepatic cholangiocarcinoma: a 31-year experience". J Hepatobiliary Pancreat Surg 5 (1): 41–7. doi:10.1007/PL00009949. PMID 9683753.
- Valverde A, Bonhomme N, Farges O, Sauvanet A, Flejou J, Belghiti J (1999). "Resection of intrahepatic cholangiocarcinoma: a Western experience". J Hepatobiliary Pancreat Surg 6 (2): 122–7. doi:10.1007/s005340050094. PMID 10398898.
- Nakagohri T, Asano T, Kinoshita H, Kenmochi T, Urashima T, Miura F, Ochiai T (2003). "Aggressive surgical resection for hilar-invasive and peripheral intrahepatic cholangiocarcinoma". World J Surg 27 (3): 289–93. doi:10.1007/s00268-002-6696-7. PMID 12607053.
- Weber S, Jarnagin W, Klimstra D, DeMatteo R, Fong Y, Blumgart L (2001). "Intrahepatic cholangiocarcinoma: resectability, recurrence pattern, and outcomes". J Am Coll Surg 193 (4): 384–91. doi:10.1016/S1072-7515(01)01016-X. PMID 11584966.
- ↑ Estimates of survival after surgery for perihilar cholangiocarcinoma include:
- Burke E, Jarnagin W, Hochwald S, Pisters P, Fong Y, Blumgart L (1998). "Hilar Cholangiocarcinoma: patterns of spread, the importance of hepatic resection for curative operation, and a presurgical clinical staging system". Ann Surg 228 (3): 385–94. doi:10.1097/00000658-199809000-00011. PMC 1191497. PMID 9742921.
- Tsao J, Nimura Y, Kamiya J, Hayakawa N, Kondo S, Nagino M, Miyachi M, Kanai M, Uesaka K, Oda K, Rossi R, Braasch J, Dugan J (2000). "Management of Hilar Cholangiocarcinoma: Comparison of an American and a Japanese Experience". Ann Surg 232 (2): 166–74. doi:10.1097/00000658-200008000-00003. PMC 1421125. PMID 10903592.
- Chamberlain R, Blumgart L (2000). "Hilar cholangiocarcinoma: a review and commentary". Ann Surg Oncol 7 (1): 55–66. doi:10.1007/s10434-000-0055-4. PMID 10674450.
- Washburn W, Lewis W, Jenkins R (1995). "Aggressive surgical resection for cholangiocarcinoma". Arch Surg 130 (3): 270–6. doi:10.1001/archsurg.1995.01430030040006. PMID 7534059.
- Nagino M, Nimura Y, Kamiya J, Kanai M, Uesaka K, Hayakawa N, Yamamoto H, Kondo S, Nishio H (1998). "Segmental liver resections for hilar cholangiocarcinoma". Hepatogastroenterology 45 (19): 7–13. PMID 9496478.
- Rea D, Munoz-Juarez M, Farnell M, Donohue J, Que F, Crownhart B, Larson D, Nagorney D (2004). "Major hepatic resection for hilar cholangiocarcinoma: analysis of 46 patients". Arch Surg 139 (5): 514–23; discussion 523–5. doi:10.1001/archsurg.139.5.514. PMID 15136352.
- Launois B, Reding R, Lebeau G, Buard J (2000). "Surgery for hilar cholangiocarcinoma: French experience in a collective survey of 552 extrahepatic bile duct cancers". J Hepatobiliary Pancreat Surg 7 (2): 128–34. doi:10.1007/s005340050166. PMID 10982604.
- ↑ Kaya M, de Groen P, Angulo P, Nagorney D, Gunderson L, Gores G, Haddock M, Lindor K (2001). "Treatment of cholangiocarcinoma complicating primary sclerosing cholangitis: the Mayo Clinic experience". Am J Gastroenterol 96 (4): 1164–9. doi:10.1111/j.1572-0241.2001.03696.x. PMID 11316165.
- ↑ Nakeeb A, Tran K, Black M, Erickson B, Ritch P, Quebbeman E, Wilson S, Demeure M, Rilling W, Dua K, Pitt H (2002). "Improved survival in resected biliary malignancies". Surgery 132 (4): 555–63; discission 563–4. doi:10.1067/msy.2002.127555. PMID 12407338.
- ↑ Khan S, Taylor-Robinson S, Toledano M, Beck A, Elliott P, Thomas H (2002). "Changing international trends in mortality rates for liver, biliary and pancreatic tumours". J Hepatol 37 (6): 806–13. doi:10.1016/S0168-8278(02)00297-0. PMID 12445422.
- ↑ Vauthey J, Blumgart L (1994). "Recent advances in the management of cholangiocarcinomas". Semin Liver Dis 14 (2): 109–14. doi:10.1055/s-2007-1007302. PMID 8047893.
- ↑ Cancer Statistics Home Page — National Cancer Institute
- ↑ Multiple independent studies have documented a steady increase in the worldwide incidence of cholangiocarcinoma. Some relevant journal articles include:
- Patel T (2002). "Worldwide trends in mortality from biliary tract malignancies". BMC Cancer 2: 10. doi:10.1186/1471-2407-2-10. PMC 113759. PMID 11991810.
- Patel T (2001). "Increasing incidence and mortality of primary intrahepatic cholangiocarcinoma in the United States". Hepatology 33 (6): 1353–7. doi:10.1053/jhep.2001.25087. PMID 11391522.
- Shaib Y, Davila J, McGlynn K, El-Serag H (2004). "Rising incidence of intrahepatic cholangiocarcinoma in the United States: a true increase?". J Hepatol 40 (3): 472–7. doi:10.1016/j.jhep.2003.11.030. PMID 15123362.
- West J, Wood H, Logan R, Quinn M, Aithal G (2006). "Trends in the incidence of primary liver and biliary tract cancers in England and Wales 1971–2001". Br J Cancer 94 (11): 1751–8. doi:10.1038/sj.bjc.6603127. PMC 2361300. PMID 16736026.
- Khan S, Taylor-Robinson S, Toledano M, Beck A, Elliott P, Thomas H (2002). "Changing international trends in mortality rates for liver, biliary and pancreatic tumours". J Hepatol 37 (6): 806–13. doi:10.1016/S0168-8278(02)00297-0. PMID 12445422.
- Welzel T, McGlynn K, Hsing A, O'Brien T, Pfeiffer R (2006). "Impact of classification of hilar cholangiocarcinomas (Klatskin tumors) on the incidence of intra- and extrahepatic cholangiocarcinoma in the United States". J Natl Cancer Inst 98 (12): 873–5. doi:10.1093/jnci/djj234. PMID 16788161.
External links
| Wikimedia Commons has media related to Cholangiocarcinoma. |
- American Cancer Society Detailed Guide to Bile Duct Cancer.
- Patient information on extrahepatic bile duct tumors, from the National Cancer Institute.
- Cancer.Net: Bile Duct Cancer
- The Cholangiocarcinoma Foundation: a resource for patients, friends, caregivers and loved ones of those affected by bile duct cancer.
- The Alan Morement Memorial Fund, the UK's only charity dedicated to the disease
- Macmillan/Cancerbackup page on Cholangiocarcinoma
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||