Cataract
| Cataract | |
|---|---|
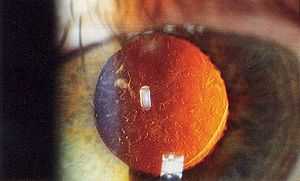
 Magnified view of a cataract in a human eye, seen on examination with a slit lamp using diffuse illumination | |
| Classification and external resources | |
| ICD-10 | H25-H26, H28, Q12.0 |
| ICD-9 | 366 |
| DiseasesDB | 2179 |
| MedlinePlus | 001001 |
| eMedicine | article/1210914 |
A cataract is a clouding of the lens inside the eye which leads to a decrease in vision. It is the most common cause of blindness worldwide and is conventionally treated with surgery. Visual loss occurs because opacification of the lens obstructs light from passing and being focused on the retina at the back of the eye.[1]
It is most commonly due to aging,[2] but has many other causes. Over time, yellow-brown pigment is deposited in the lens, and this, together with disruption of the lens fibers, reduces the transmission of light and leads to visual problems.
Those with cataracts often experience difficulty in appreciating colors and changes in contrast, driving, reading, recognizing faces, and coping with glare from bright lights.[3]
Classification

Cataracts may be partial or complete, stationary or progressive, or hard or soft. The main types of age-related cataracts are nuclear sclerosis, cortical, and posterior subcapsular.
Nuclear sclerosis, the most common type of cataract, involves the central or 'nuclear' part of the lens. Over time, this becomes hard or 'sclerotic' due to condensation of lens nucleus and deposition of brown pigment within the lens. In advanced stages, it is called brunescent cataract. This type of cataract can present with a shift to nearsightedness and causes problems with distance vision, while reading is less affected.[4]
Cortical cataracts are due to the lens cortex (outer layer) becoming opaque. They occur when changes in the water content of the periphery of the lens causes fissuring. When these cataracts are viewed through an ophthalmoscope or other magnification system, the appearance is similar to white spokes of a wheel. Symptoms often include problems with glare and light scatter at night.[4]
Posterior subcapsular cataracts are cloudy at back of the lens adjacent to the capsule (or bag) in which the lens sits. Because light becomes more focused toward the back of the lens, they can cause disproportionate symptoms for their size.
An immature cataract has some transparent protein, but with a mature cataract, all the lens protein is opaque. In a hypermature or Morgagnian cataract, the lens proteins have become liquid. Congenital cataract, which may be detected in adulthood, has a different classification and includes lamellar, polar, and sutural cataracts.[5][6]
Cataracts can be classified by using the lens opacities classification system LOCS III. In this system, cataracts are classified based on type as nuclear, cortical, or posterior. The cataracts are further classified based on severity on a scale from 1 to 5. The LOCS III system is highly reproducible.[7]
Signs and symptoms
_PHIL_4284_lores.jpg)
Signs and symptoms vary depending on the type of cataract, though considerable overlap occurs. People with nuclear sclerotic or brunescent cataracts often notice a reduction of vision. Those with posterior subcapsular cataracts usually complain of glare as their major symptom.[8]
The severity of cataract formation, assuming no other eye disease is present, is judged primarily by a visual acuity test. The appropriateness of surgery depends on a patient's particular functional and visual needs and other risk factors, all of which may vary widely.[9]
Causes
Age
Age is the most common cause.[2] Lens proteins denature and degrade over time, and this process is accelerated by diseases such as diabetes mellitus and hypertension. Environmental factors, including toxins, radiation, and ultraviolet light, have cumulative effects, which are worsened by the loss of protective and restorative mechanisms due to alterations in gene expression and chemical processes within the eye.[10]
Trauma
Blunt trauma causes swelling, thickening, and whitening of the lens fibers. While the swelling normally resolves with time, the white color may remain. In severe blunt trauma, or injuries which penetrate the eye, the capsule in which the lens sits can be damaged. This allows water from other parts of the eye to rapidly enter the lens leading to swelling and then whitening, obstructing light from reaching the retina at the back of the eye. Cataracts may develop in 0.7 to 8.0% of cases following electrical injuries.[11]
Radiation
Ultraviolet light, specifically UVB, has been shown to cause cataracts, and some evidence indicates sunglasses worn at an early age can slow its development in later life.[12] The lens filters UV light; so once it is removed via surgery, one may be able to see UV light.[13] Microwave radiation has also been found to cause cataracts. The mechanism is unclear, but may include changes in heat-sensitive enzymes that normally protect cell proteins in the lens. Another possible mechanism is direct damage to the lens from pressure waves induced in the aqueous humor. Cataracts have also been associated with ionizing radiation such as X-rays. The addition of damage to the DNA of the lens cells also has been considered.[14] Finally, electric and heat injuries denature and whiten the lens as a result of direct protein coagulation.[10] This same process makes the clear albumin of an egg become white and opaque after cooking. Cataracts of this type are often seen in glassblowers and furnace workers. Lasers of sufficient power output are known to damage the eyes and skin.
Genetics
The genetic component is strong in the development of cataracts, most commonly through mechanisms that protect and maintain the lens. The presence of cataracts in childhood or early life can occasionally be due to a particular syndrome. Examples of chromosome abnormalities associated with cataracts include 1q21.1 deletion syndrome, cri-du-chat syndrome, Down syndrome, Patau's syndrome, trisomy 18 (Edward's syndrome), and Turner's syndrome. Examples of single-gene disorder include Alport's syndrome, Conradi's syndrome, myotonic dystrophy, and oculocerebrorenal syndrome or Lowe syndrome.
Skin diseases
The skin and the lens have the same embryological origin and can be affected by similar diseases. Those with atopic dermatitis and eczema occasionally develop shield ulcers cataracts. Ichthyosis is an autosomal recessive disorder associated with cuneiform cataracts and nuclear sclerosis. Basal-cell nevus and pemphigus have similar associations.
Drug use
Cigarette smoking has been shown to double the rate of nuclear sclerotic cataracts and triple the rate of posterior subcapsular cataracts.[15] Evidence is conflicting over the effect of alcohol. Some surveys have shown a link, but others which followed patients over longer terms have not.[16]
Medications
Some drugs, such as corticosteroids, can induce cataract development.[5] People with schizophrenia often have risk factors for lens opacities (such as diabetes, hypertension, and poor nutrition) but antipsychotic medications are unlikely to contribute to cataract formation.[17] Miotics[18] and triparanol may increase the risk.[19]
Other diseases
|
|
Prevention
Risk factors such as UVB exposure and smoking can be addressed, but are unlikely to make large difference to visual function. Although no means of preventing cataracts has been scientifically proven, wearing ultraviolet-protecting sunglasses may slow the development.[20][21] While regular intake of antioxidants (such as vitamins A, C, and E) has been thought to protect against the risk of cataracts, clinical trials have shown it does not.[22] Evidence is mixed, but weakly positive, for a potential protective effect of the nutrients lutein and zeaxanthin.[23] Statin use is somewhat associated with a lower risk of nuclear sclerotic cataract.[24]
Treatment
Surgical

Cataract removal can be performed at any stage and no longer requires ripening of the lens. Surgery is usually 'outpatient' and performed using local anesthesia. About 9 of 10 patients can achieve a corrected vision of 20/40 or better after surgery.[4]
Several recent evaluations found surgery can only meet expectations when significant functional impairment from poor vision exists prior to surgery. Visual function estimates such as VF-14 have been found to give more realistic estimates than visual acuity testing alone.[4][25] In some developed countries, a trend to overuse cataract surgery has been noted, which may lead to disappointing results.[26]
Phacoemulsification is the most widely used cataract surgery. This procedure uses ultrasonic energy to emulsify the cataract lens. Phacoemulsification typically comprises six steps:
- Anaesthetic - The eye is numbed with either a subtenon injection around the eye or using simple eye drops.
- Corneal incision - Two cuts are made through the clear cornea to allow insertion of instruments into the eye.
- Capsulorhexis - A needle or small pair of forceps is used to create a circular hole in the capsule in which the lens sits.
- Phacoemulsification - A handheld probe is used to break up and emulsify the lens into liquid using the energy of ultrasound waves. The resulting 'emulsion' is sucked away.
- Irrigation and aspiration - The cortex, which is the soft outer layer of the cataract, is aspirated or sucked away. Fluid removed is continually replaced with a saline solution to prevent collapse of the structure of the anterior chamber (the front part of the eye).
- Lens insertion - A plastic, foldable lens is inserted into the capsular bag that formerly contained the natural lens. Some surgeons also inject an antibiotic into the eye to reduce the risk of infection. The final step is to inject salt water into the corneal wounds to cause the area to swell and seal the incision.
Extracapsular cataract extraction (ECCE) consists of removing the lens manually, but leaving the majority of the capsule intact. The lens is expressed through a 10– to 12-mm incision which is closed with sutures at the end of surgery. ECCE is less frequently performed than phacoemulsification, but can be useful when dealing with very hard cataracts or other situations where emulsification is problematic. Manual small incision cataract surgery (MSICS) has evolved from ECCE. In MSICS, the lens is removed through a self-sealing scleral tunnel wound in the sclera which, ideally, is watertight and does not require suturing. Although "small", the incision is still markedly larger than the portal in phacoemulsion. This surgery is increasingly popular in the developing world where access to phacoemulsification is still limited.
Intracapsular cataract extraction (ICCE) is rarely performed. The lens and surrounding capsule are removed in one piece through a large incision while pressure is applied to the vitreous membrane. The surgery has a high rate of complications.
Prognosis
Postoperative care

The postoperative recovery period (after removing the cataract) is usually short. The patient is usually ambulatory on the day of surgery, but is advised to move cautiously and avoid straining or heavy lifting for about a month. The eye is usually patched on the day of surgery and use of an eye shield at night is often suggested for several days after surgery.[9]
In all types of surgery, the cataractous lens is removed and replaced with an artificial lens, known as an intraocular lens, which stays in the eye permanently. Intraocular lenses are usually monofocal, correcting for either distance or near vision. Multifocal lenses may be implanted to improve near and distance vision simultaneously, but these lenses may increase the chance of unsatisfactory vision.[10]
Complications
Serious complications of cataract surgery are retinal detachment and endophthalmitis. In both cases, patients notice a sudden decrease in vision. In endophthalmitis, patients often describe pain. Retinal detachment frequently presents with unilateral visual field defects, blurring of vision, flashes of light, or floating spots.
The risk of retinal detachment was estimated as about 0.4% within 5.5 years, corresponding to a 2.3-fold risk increase compared to naturally expected incidence, with older studies reporting a substantially higher risk. The incidence is increasing over time in a somewhat linear manner, and the risk increase lasts for at least 20 years after the procedure. Particular risk factors are younger age, male sex, longer axial length, and complications during surgery. In the highest risk group of patients, the incidence of pseudophakic retinal detachment may be as high as 20%.[27][28]
The risk of endophthalmitis occurring after surgery is less than one in 1000.[29]
Corneal oedema and cystoid macular oedema are less serious but more common, and occur because of persistent swelling at the front of the eye in corneal oedema or back of the eye in cystoid macular oedema. They are normally the result of excessive inflammation following surgery, and in both cases, patients may notice blurred, foggy vision. They normally improve with time and with application of anti-inflammatory drops. The risk of either occurring is around one in 100.
Posterior capsular opacification, also known as after-cataract, is a condition in which months or years after successful cataract surgery, vision deteriorates or problems with glare and light scattering recur, usually due to thickening of the back or posterior capsule surrounding the implanted lens, so-called 'posterior lens capsule opacification'. Growth of natural lens cells remaining after the natural lens was removed may be the cause, and the younger the patient, the greater the chance of this occurring. Management involves cutting a small, circular area in the posterior capsule with targeted beams of energy from a laser, called Nd:YAG laser capsulotomy, after the type of laser used. The laser can be aimed very accurately, and the small part of the capsule which is cut falls harmlessly to the bottom of the inside of the eye. This procedure leaves sufficient capsule to hold the lens in place, but removes enough to allow light to pass directly through to the retina. Serious side effects are rare.[30] Posterior capsular opacification is common and occurs following up to one in four operations, but these rates are decreasing following the introduction of modern intraocular lenses together with a better understanding of the causes.
Vitreous touch syndrome is a possible complication of intracapsular cataract extraction.[31]
Epidemiology

no data
<90
90–180
180–270
270–360
360–450
450–540
|
540–630
630–720
720–810
810–900
900–990
>990
|
Age-related cataracts are responsible for 51% of world blindness, about 20 million people.[33] Globally, cataracts cause moderate to severe disability in 53.8 million (2004), 52.2 million of whom are in low and middle income countries.[34]
In many countries, surgical services are inadequate, and cataracts remain the leading cause of blindness. Even where surgical services are available, low vision associated with cataracts may still be prevalent as a result of long waits for, and barriers to, surgery, such as cost, lack of information and transportation problems.
In the United States, age-related lens changes have been reported in 42% between the ages of 52 and 64,[35] 60% between the ages 65 and 74,[36] and 91% between the ages of 75 and 85.[35] Cataracts affect nearly 22 million Americans age 40 and older. By age 80, more than half of all Americans have cataracts. Direct medical costs for cataract treatment are estimated at $6.8 billion annually.[37]
In the eastern Mediterranean region, cataracts are responsible for over 51% of blindness. Access to eye care in many countries in this region is limited.[38]
History
The first references to cataracts and their treatment in Ancient Rome are found in 29 AD in De Medicinae, the work of the Latin encyclopedist Aulus Cornelius Celsus.[39] Archaeological evidence of eye surgery in the Roman era also exists.[40]
Other early accounts are found in Sanskrit. Cataract surgery was described by the Indian physician, Suśruta (about 200 AD).[41]
Muslim ophthalmologist Ammar ibn Ali, in his Choice of Eye Diseases, written circa 1000, wrote of his invention of a syringe and the technique of cataract extraction while experimenting with it on a patient.[42]
Etymology
"Cataract" is derived from the Latin cataracta, meaning "waterfall", and from the Ancient Greek καταρράκτης (katarrhaktēs), "down-rushing",[43] from καταράσσω (katarassō) meaning "to dash down"[44] (from kata-, "down"; arassein, "to strike, dash").[45] As rapidly running water turns white, so the term may have been used metaphorically to describe the similar appearance of mature ocular opacities. In Latin, cataracta had the alternative meaning "portcullis"[46] and the name possibly passed through French to form the English meaning "eye disease" (early 15th century), on the notion of "obstruction".[47] Early Persian physicians called the term nazul-i-ah, or "descent of the water"—vulgarised into waterfall disease or cataract—believing such blindness to be caused by an outpouring of corrupt humour into the eye.[48]
Research
.jpg)
N-Acetylcarnosine drops have been investigated as a medical treatment for cataracts. The drops are believed to work by reducing oxidation and glycation damage in the lens, particularly reducing crystallin crosslinking.[49][50] Some benefit has been shown in small manufacturer sponsored randomized controlled trials but further independent corroboration is still required.[51]
Femtosecond laser mode-locking, used during cataract surgery, was originally used to cut accurate and predictable flaps in LASIK surgery, and has been introduced to cataract surgery. The incision at the junction of the sclera and cornea and the hole in capsule during capsulorhexis, traditionally made with a handheld blade, needle, and forceps, are dependent on skill and experience of the surgeon. Sophisticated three-dimensional images of the eyes can be used to guide lasers to make these incisions. Nd:YAG_laser can also then break up the cataract as in phacoemulsification.[52]
References
- ↑ Quillen DA (July 1999). "Common causes of vision loss in elderly patients". Am Fam Physician 60 (1): 99–108. PMID 10414631.
- ↑ 2.0 2.1 Courtney P (1992). "The National Cataract Surgery Survey: I. Method and descriptive features". Eye (Lond) 6 (Pt 5): 487–92. doi:10.1038/eye.1992.103. PMID 1286712.
- ↑ Allen D, Vasavada A (2006). "Cataract and surgery for cataract". BMJ 333 (7559): 128–32. doi:10.1136/bmj.333.7559.128. PMC 1502210. PMID 16840470.
- ↑ 4.0 4.1 4.2 4.3 Bollinger KE, Langston RH (2008). "What can patients expect from cataract surgery?". Cleveland Clinic journal of medicine 75 (3): 193–196, 199–196. doi:10.3949/ccjm.75.3.193. PMID 18383928.
- ↑ 5.0 5.1 Spencer RW, Andelman SY (1965). "Steroid cataracts. Posterior subcapsular cataract formation in rheumatoid arthritis patients on long term steroid therapy". Arch Ophthalmol 74: 38–41. doi:10.1001/archopht.1965.00970040040009. PMID 14303339.
- ↑ Greiner JV, Chylack LT (1979). "Posterior subcapsular cataracts: histopathologic study of steroid-associated cataracts". Arch Ophthalmol 97 (1): 135–44. doi:10.1001/archopht.1979.01020010069017. PMID 758890.
- ↑ Yanoff & Duker 2008, p. 412
- ↑ "Posterior Supcapsular Cataract". Digital Reference of Ophthalmology. Edward S. Harkness Eye Institute, Department of Ophthalmology of Columbia University. 2003. Retrieved 2 April 2013.
- ↑ 9.0 9.1 Emmett T. Cunningham, Paul Riordan-Eva. Vaughan & Asbury's general ophthalmology. (18th ed. ed.). McGraw-Hill Medical. ISBN 978-0071634205.
- ↑ 10.0 10.1 10.2 Duker, Jay S.; Myron Yanoff MD; Yanoff, Myron; Jay S. Duker MD (2009). Ophthalmology. St. Louis, Mo: Mosby/Elsevier. ISBN 0-323-04332-1.
- ↑ Reddy SC (Apr–Jun 1999). "Electric cataract: a case report and review of the literature.". European journal of ophthalmology 9 (2): 134–8. PMID 10435427.
- ↑ Sliney DH (1994). "UV radiation ocular exposure dosimetry". Doc Ophthalmol 88 (3-4): 243–54. doi:10.1007/bf01203678. PMID 7634993.
- ↑ Komarnitsky. "Case study of ultraviolet vision after IOL removal for Cataract Surgery".
- ↑ Lipman RM, Tripathi BJ, Tripathi RC (1988). "Cataracts induced by microwave and ionizing radiation". Surv Ophthalmol 33 (3): 200–10. doi:10.1016/0039-6257(88)90088-4. PMID 3068822.
- ↑ Christen WG, Manson JE, Seddon JM, Glynn RJ, Buring JE, Rosner B, Hennekens CH (August 1992). "A prospective study of cigarette smoking and risk of cataract in men". JAMA 268 (8): 989–93. doi:10.1001/jama.1992.03490080063025. PMID 1501324.
- ↑ Wang S, Wang JJ, Wong TY (2008). "Alcohol and eye diseases". Surv Ophthalmol 53 (5): 512–25. doi:10.1016/j.survophthal.2008.06.003. PMID 18929762.
- ↑ Uçok A, Gaebel W (February 2008). "Side effects of atypical antipsychotics: a brief overview.". World psychiatry: official journal of the World Psychiatric Association (WPA) 7 (1): 58–62. PMC 2327229. PMID 18458771.
- ↑ van den Brûle J, Degueldre F, Galand A (December 1998). "Cataractes incitées de médicament" [Drug-induced cataracts]. Revue médicale de Liège (in French) 53 (12): 766–9. PMID 9927876.
- ↑ "Triperanol". MeSH. National Library of Medicine. Retrieved 2013-02-06.
- ↑ Neale RE, Purdie JL, Hirst LW, Green AC (November 2003). "Sun exposure as a risk factor for nuclear cataract". Epidemiology 14 (6): 707–712. doi:10.1097/01.ede.0000086881.84657.98. PMID 14569187.
- ↑ Javitt JC, Wang F, West SK (1996). "Blindness Due to Cataract: Epidemiology and Prevention" (PDF). Annual review of public health 17: 159–77. doi:10.1146/annurev.pu.17.050196.001111. PMID 8724222. Cited in Five-Year Agenda for the National Eye Health Education Program (NEHEP), p. B-2; National Eye Institute, U.S. National Institutes of Health
- ↑ Mathew MC, Ervin AM, Tao J, Davis RM (Jun 13, 2012). "Antioxidant vitamin supplementation for preventing and slowing the progression of age-related cataract.". Cochrane Database Syst Rev. 6: CD004567. doi:10.1002/14651858.CD004567.pub2. PMID 22696344.
- ↑ Barker FM (August 2010). "Dietary supplementation: effects on visual performance and occurrence of AMD and cataracts". Curr Med Res Opin 26 (8): 2011–23. doi:10.1185/03007995.2010.494549. PMID 20590393.
- ↑ Klein BE, Klein R, Lee KE, Grady LM (2006). "Statin Use and Incident Nuclear Cataract". Journal of the American Medical Association 295 (23): 2752–8. doi:10.1001/jama.295.23.2752. PMID 16788130.
- ↑ Davis JC, McNeill H, Wasdell M, Chunick S, Bryan S (2012). "Focussing both eyes on health outcomes: Revisiting cataract surgery". BMC Geriatrics 12: 50. doi:10.1186/1471-2318-12-50. PMC 3497611. PMID 22943071.
- ↑ Black N, Browne J, van der Meulen J, Jamieson L, Copley L, Lewsey J (2008). "Is there overutilisation of cataract surgery in England?". British Journal of Ophthalmology 93 (1): 13–17. doi:10.1136/bjo.2007.136150. PMID 19098042.
- ↑ Olsen T, Jeppesen P (2012). "The Incidence of Retinal Detachment After Cataract Surgery". The Open Ophthalmology Journal 6: 79–82. doi:10.2174/1874364101206010079. PMC 3447164. PMID 23002414.
- ↑ Herrmann W, Helbig H, Heimann H (2011). "Pseudophakie-Ablatio". Klinische Monatsblätter für Augenheilkunde 228 (3): 195–200. doi:10.1055/s-0029-1246116. PMID 21374539.
- ↑ Behndig A, Montan P, Stenevi U, Kugelberg M, Lundström M (August 2011). "One million cataract surgeries: Swedish National Cataract Register 1992-2009". J Cataract Refract Surg 37 (8): 1539–45. doi:10.1016/j.jcrs.2011.05.021. PMID 21782099.
- ↑ "Posterior capsule opacification - why laser treatment is sometimes needed following cataract surgery". rnib.org.uk.
- ↑ Dr. Kushal Banerjee (2006). "A review and clinical evaluation of per-operative and post-operative complications in case of manual small incision cataract surgery and extracapsular cataract extraction with posterior chamber intra-ocular lens implantation" (PDF). Retrieved 1 June 2014.
- ↑ "Death and DALY estimates for 2004 by cause for WHO Member States" (XLS). World Health Organization. who.int. 2004.
- ↑ "Priority eye diseases: Cataract". Prevention of Blindness and Visual Impairment. World Health Organization. WHO.int], | .
- ↑ Organization, World Health (2008). The global burden of disease : 2004 update. Geneva, Switzerland: World Health Organization. p. 35. ISBN 9789241563710.
- ↑ 35.0 35.1 Sperduto RD, Seigel D (Jul 1980). "Senile lens and senile macular changes in a population-based sample". Am J Ophthalmol 90 (1): 86–91. PMID 7395962.
- ↑ Kahn HA, Leibowitz HM, Ganley JP, Kini MM, Colton T, Nickerson RS, Dawber TR (Jul 1977). "The Framingham Eye Study. I. Outline and major prevalence findings". Am J Epidemiol 106 (1): 17–32. PMID 879158.
- ↑ "Eye Health Statistics at a Glance" (PDF).
- ↑ "Health Topics: Cataract". World Health Organization - Eastern Mediterranean Regional Office.
- ↑ Aulus Cornelius Celsus, G. F. Collier (transl.) (1831). De Medicinae. OL 5225311W.
- ↑ Elliott, Jane (February 9, 2008). "The Romans carried out cataract ops". BBC News.
- ↑ Suśruta, P. V. Sharma (trans.) (2000). Suśruta-Saṃhitā 1. Varanasi: Caukhambha Visvabharati. p. iv. OL 160267M.
- ↑ Finger, Stanley (1994). Origins of Neuroscience: A History of Explorations Into Brain Function. Oxford University Press. p. 70. ISBN 0-19-514694-8.
- ↑ καταρράκτης, Henry George Liddell, Robert Scott, A Greek-English Lexicon, on Perseus
- ↑ καταράσσω, Henry George Liddell, Robert Scott,A Greek-English Lexicon, on Perseus
- ↑ "cataract". Word of the Day. Dictionary.com. 29 October 2003.
"cataract". Oxford Dictionaries. Oxford University Press. - ↑ cataracta, Charlton T. Lewis, Charles Short, A Latin Dictionary, on Perseus
- ↑ Online Etymology Dictionary, etymonline.com
- ↑ Mistaken Science — Topic Powered by eve community, Wordcraft Forums, wordcraft.infopop.cc
- ↑ Williams DL, Munday P (2006). "The effect of a topical antioxidant formulation including N-acetyl carnosine on canine cataract: a preliminary study". Vet Ophthalmol 9 (5): 311–6. doi:10.1111/j.1463-5224.2006.00492.x. PMID 16939459.
- ↑ Guo Y, Yan H (2006). "Preventive effect of carnosine on cataract development". Yan Ke Xue Bao 22 (2): 85–8. PMID 17162883.
- ↑ Toh T, Morton J, Coxon J, Elder MJ (2007). "Medical treatment of cataract". Clin. Experiment. Ophthalmol. 35 (7): 664–71. doi:10.1111/j.1442-9071.2007.01559.x. PMID 17894689.
- ↑ Friedman NJ, Palanker DV, Schuele G, Andersen D, Marcellino G, Seibel BS, Batlle J, Feliz R, Talamo JH, Blumenkranz MS, Culbertson WW (July 2011). "Femtosecond laser capsulotomy". J Cataract Refract Surg 37 (7): 1189–98. doi:10.1016/j.jcrs.2011.04.022. PMID 21700099. as PDF The authors declare a financial interest in a company producing femtosecond laser equipment.
Bibliography
- Yanoff, Myron; Duker, Jay S. (2008). Ophthalmology (3rd ed.). Edinburgh: Mosby. ISBN 978-0323057516.
External links
- Pictures of Different types of Cataract s
- Cataract at DMOZ
- Video describing history and science of seeing cataracts in your own eye on YouTube