Avian influenza
| Influenza (Flu) |
|---|
 |
| Types |
| Vaccines |
| Treatment |
| Pandemics |
|
| Outbreaks |
| See also |
|
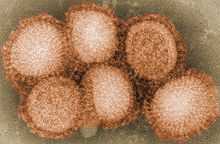
Avian influenza — known informally as avian flu or bird flu — refers to "influenza caused by viruses adapted to birds."[1][2][3][4][5][6][7] The version with the greatest concern is highly pathogenic avian influenza (HPAI).
"Bird flu" is a phrase similar to "swine flu," "dog flu," "horse flu," or "human flu" in that it refers to an illness caused by any of many different strains of influenza viruses that have adapted to a specific host. All known viruses that cause influenza in birds belong to the species influenza A virus. All subtypes (but not all strains of all subtypes) of influenza A virus are adapted to birds, which is why for many purposes avian flu virus is the influenza A virus. (Note, however, that the "A" does not stand for "avian").
Adaptation is not exclusive. Being adapted toward a particular species does not preclude adaptations, or partial adaptations, toward infecting different species. In this way, strains of influenza viruses are adapted to multiple species, though may be preferential toward a particular host. For example, viruses responsible for influenza pandemics are adapted to both humans and birds. Recent influenza research into the genes of the Spanish flu virus shows it to have genes adapted to both birds and humans, with more of its genes from birds than less deadly later pandemic strains.
While its most highly pathogenic strain (H5N1) had been spreading throughout Asia since 2003, avian influenza reached Europe in 2005, and the Middle East, as well as Africa, the following year.[8] On January 22, 2012, China reported its second human death due to bird flu in a month following other fatalities in Vietnam and Cambodia.[9] Companion birds in captivity and parrots are highly unlikely to contract the virus, and there has been no report of a companion bird with avian influenza since 2003. Pigeons do not contract or spread the virus.[10][11][12] 84% of affected bird populations are composed of chicken and farm birds, while the 15% is madeup of wild birds according to capture-and-release operations in the 2000s, during the SARs pandemic. The first deadly Canadian case was confirmed on January 3, 2014.[13]On December 2, 2014, two turkey farms in British Columbia, Canada, had been placed under quarantine after the Canadian Food Inspection Agency confirmed an avian flu outbreak [14]
Genetics
Genetic factors in distinguishing between "human flu viruses" and "avian flu viruses" include:
- PB2: (RNA polymerase): Amino acid (or residue) position 627 in the PB2 protein encoded by the PB2 RNA gene. Until H5N1, all known avian influenza viruses had a Glu at position 627, while all human influenza viruses had a Lys.
- HA: (hemagglutinin): Avian influenza HA viruses bind alpha 2-3 sialic acid receptors, while human influenza HA viruses bind alpha 2-6 sialic acid receptors. Swine influenza viruses have the ability to bind both types of sialic acid receptors. Hemagglutinin is the major antigen of the virus against which neutralizing antibodies are produced, and influenza virus epidemics are associated with changes in its antigenic structure. This was originally derived from pigs, and should technically be referred to as "pig flu" [15]
Subtypes
There are many subtypes of avian influenza viruses, but only some strains of five subtypes have been highly pathogenic in humans. These are types H5N1, H7N3, H7N7, H7N9, and H9N2.[16] At least one person, an elderly woman in Jiangxi Province, China, died of pneumonia in December 2013 from the H10N8 strain, the first human fatality confirmed to be caused by that strain.[17]
Contraction/spreading of avian influenza
Most human contractions of the avian flu are a result of either handling dead infected birds or from contact with infected fluids. While most wild birds mainly have only a mild form of the H5N1 strain, once domesticated birds such as chickens or turkeys are infected, it could become much more deadly because the birds are often within close contact of one another. There is currently a large threat of this in Asia with infected poultry due to low hygiene conditions and close quarters. Although it is easy for humans to become infected from birds, it's much more difficult to do so from human to human without close and lasting contact.
Spreading of H5N1 from Asia to Europe is much more likely caused by both legal and illegal poultry trades than dispersing through wild bird migrations, being that in recent studies, there were no secondary rises in infection in Asia when wild birds migrate south again from their breeding grounds. Instead, the infection patterns followed transportation such as railroads, roads, and country borders, suggesting poultry trade as being much more likely. While there have been strains of avian flu to exist in the United States, such as Texas in 2004, they have been extinguished and have not been known to infect humans.
Examples of avian influenza A virus strains:[18]
| HA subtype designation |
NA subtype designation |
Avian influenza A viruses |
|---|---|---|
| H1 | N1 | A/duck/Alberta/35/76(H1N1) |
| H1 | N8 | A/duck/Alberta/97/77(H1N8) |
| H2 | N9 | A/duck/Germany/1/72(H2N9) |
| H3 | N8 | A/duck/Ukraine/63(H3N8) |
| H3 | N8 | A/duck/England/62(H3N8) |
| H3 | N2 | A/turkey/England/69(H3N2) |
| H4 | N6 | A/duck/Czechoslovakia/56(H4N6) |
| H4 | N3 | A/duck/Alberta/300/77(H4N3) |
| H5 | N3 | A/tern/South Africa/300/77(H4N3) |
| H5 | N4 | A/Ethiopia/300/77(H6N6) |
| H5 | N9 | A/turkey/Ontario/7732/66(H5N9) |
| H5 | N1 | A/chick/Scotland/59(H5N1) |
| H6 | N2 | A/turkey/Massachusetts/3740/65(H6N2) |
| H6 | N8 | A/turkey/Canada/63(H6N8) |
| H6 | N5 | A/shearwater/Australia/72(H6N5) |
| H6 | N6 | A/jyotichinara/Ehiopia/73(H6N6) |
| H6 | N1 | A/duck/Germany/1868/68(H6N1) |
| H7 | N7 | A/fowl plague virus/Dutch/27(H7N7) |
| H7 | N1 | A/chick/Brescia/1902(H7N1) |
| H7 | N9 | A/chick/China/2013(H7N9) |
| H7 | N3 | A/turkey/England/639H7N3) |
| H7 | N1 | A/fowl plague virus/Rostock/34(H7N1) |
| H8 | N4 | A/turkey/Ontario/6118/68(H8N4) |
| H9 | N2 | A/turkey/Wisconsin/1/66(H9N2) |
| H9 | N6 | A/duck/Hong Kong/147/77(H9N6) |
| H9 | N6 | A/duck/Hong Kong/147/77(H9N6) |
| H9 | N8 | A/manishsurpur/Malawi/149/77(H9N8) |
| H9 | N7 | A/turkey/Scotland/70(H9N7) |
| H10 | N8 | A/quail/Italy/1117/65(H10N8) |
| H11 | N6 | A/duck/England/56(H11N6) |
| H11 | N9 | A/duck/Memphis/546/74(H11N9) |
| H12 | N5 | A/duck/Alberta/60/76/(H12N5) |
| H13 | N6 | A/gull/Maryland/704/77(H13N6) |
| H14 | N4 | A/duck/Gurjev/263/83(H14N4) |
| H15 | N9 | A/shearwater/Australia/2576/83(H15N9) |
Influenza pandemic
Pandemic flu viruses have some avian flu virus genes and usually some human flu virus genes. Both the H2N2 and H3N2 pandemic strains contained genes from avian influenza viruses. The new subtypes arose in pigs coinfected with avian and human viruses, and were soon transferred to humans. Swine were considered the original "intermediate host" for influenza, because they supported reassortment of divergent subtypes. However, other hosts appear capable of similar coinfection (e.g., many poultry species), and direct transmission of avian viruses to humans is possible.[19] The Spanish flu virus strain may have been transmitted directly from birds to humans.[20]
In spite of their pandemic connection, avian influenza viruses are noninfectious for most species. When they are infectious, they are usually asymptomatic, so the carrier does not have any disease from it. Thus, while infected with an avian flu virus, the animal does not have a "flu". Typically, when illness (called "flu") from an avian flu virus does occur, it is the result of an avian flu virus strain adapted to one species spreading to another species (usually from one bird species to another bird species). So far as is known, the most common result of this is an illness so minor as to be not worth noticing (and thus little studied). But with the domestication of chickens and turkeys, humans have created species subtypes (domesticated poultry) that can catch an avian flu virus adapted to waterfowl and have it rapidly mutate into a form that kills over 90% of an entire flock in days, can spread to other flocks and kill 90% of them, and can only be stopped by killing every domestic bird in the area. Until H5N1 infected humans in the 1990s, this was the only reason avian flu was considered important. Since then, avian flu viruses have been intensively studied; resulting in changes in what is believed about flu pandemics, changes in poultry farming, changes in flu vaccination research, and changes in flu pandemic planning.
Influenza A/H5N1 has evolved into a flu virus strain that infects more species than any previously known strain, is deadlier than any previously known strain, and continues to evolve, becoming both more widespread and more deadly. This caused Robert G. Webster, a leading expert on avian flu, to publish an article titled "The world is teetering on the edge of a pandemic that could kill a large fraction of the human population" in American Scientist. He called for adequate resources to fight what he sees as a major world threat to possibly billions of lives.[21]
Vaccines for poultry have been formulated against several of the avian H5N1 influenza varieties. Vaccination of poultry against the ongoing H5N1 epizootic is widespread in certain countries. Some vaccines also exist for use in humans, and others are in testing, but none have been made available to civilian populations, nor are produced in quantities sufficient to protect more than a tiny fraction of the Earth's population in the event of an H5N1 pandemic outbreak. The World Health Organization has compiled a list of known clinical trials of pandemic influenza prototype vaccines, including those against H5N1.
H5N1
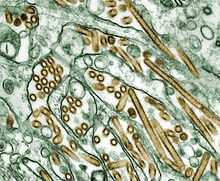 |
The highly pathogenic influenza A virus subtype H5N1 is an emerging avian influenza virus that has been causing global concern as a potential pandemic threat. It is often referred to simply as "bird flu" or "avian influenza", even though it is only one subtype of avian influenza-causing virus.
H5N1 has killed millions of poultry in a growing number of countries throughout Asia, Europe, and Africa. Health experts are concerned that the coexistence of human flu viruses and avian flu viruses (especially H5N1) will provide an opportunity for genetic material to be exchanged between species-specific viruses, possibly creating a new virulent influenza strain that is easily transmissible and lethal to humans. The mortality rate for humans with H5N1 is 60%.
Since the first H5N1 outbreak occurred in 1987, there has been an increasing number of HPAI H5N1 bird-to-human transmissions, leading to clinically severe and fatal human infections. Because a significant species barrier exists between birds and humans, though, the virus does not easily cross over to humans, though some cases of infection are being researched to discern whether human to human transmission is occurring.[19] More research is necessary to understand the pathogenesis and epidemiology of the H5N1 virus in humans. Exposure routes and other disease transmission characteristics, such as genetic and immunological factors that may increase the likelihood of infection, are not clearly understood.[22]
On January 18, 2009, a 27-year-old woman from eastern China died of bird flu, Chinese authorities said, making her the second person to die from the deadly virus at that time. Two tests on the woman were positive for H5N1 avian influenza, said the ministry, which did not say how she might have contracted the virus.[23]
Although millions of birds have become infected with the virus since its discovery, 359 humans have died from the H5N1 in twelve countries according to WHO data as of August 10, 2012.[24]
The avian flu claimed at least 300 humans in Azerbaijan, Cambodia, China, Egypt, Indonesia, Iraq, Laos, Nigeria, Pakistan, Thailand, Turkey, and Vietnam. Epidemiologists are afraid the next time such a virus mutates, it could pass from human to human; however, the current A/H5N1 virus does not transmit easily from human to human. If this form of transmission occurs, another pandemic could result. Thus, disease-control centers around the world are making avian flu a top priority. These organizations encourage poultry-related operations to develop a preemptive plan to prevent the spread of H5N1 and its potentially pandemic strains. The recommended plans center on providing protective clothing for workers and isolating flocks to prevent the spread of the virus.[25]
The Thailand outbreak of avian flu caused massive economic losses, especially among poultry workers. Infected birds were culled and slaughtered. The public lost confidence with the poultry products, thus decreasing the consumption of chicken products. This also elicited a ban from importing countries. There were, however, factors which aggravated the spread of the virus, including bird migration, cool temperature (increases virus survival) and several festivals at that time.[26]
H7N9
Influenza A virus subtype H7N9 is a novel avian influenza virus first reported to have infected humans in 2013 in China.[27] Most of the reported cases of human infection have resulted in severe respiratory illness.[28] In the month following the report of the first case, more than 100 people had been infected, an unusually high rate for a new infection; a fifth of those patients had died, a fifth had recovered, and the rest remained critically ill.[29] The World Health Organization (WHO) has identified H7N9 as "...an unusually dangerous virus for humans."[30] As of June 30, 133 cases have been reported, resulting in the deaths of 43.
Research regarding background and transmission is ongoing.[31] It has been established that many of the human cases of H7N9 appear to have a link to live bird markets.[32] As of July, there has been no evidence of sustained human-to-human transmission, however a study group headed by one of the world’s leading experts on avian flu reported that several instances of human-to-human infection are suspected.[33] It has been reported that H7N9 virus does not kill poultry, which will make surveillance much more difficult. Researchers have commented on the unusual prevalence of older males among H7N9-infected patients.[34] While several environmental, behavioral, and biological explanations for this pattern have been proposed,[35] as yet, the reason is unknown.[36] Currently no vaccine exists, but the use of influenza antiviral drugs known as neuraminidase inhibitors in cases of early infection may be effective.[37]
The number of cases detected after April fell abruptly. The decrease in the number of new human H7N9 cases may have resulted from containment measures taken by Chinese authorities, including closing live bird markets, or from a change in seasons, or possibly a combination of both factors. Studies indicate that avian influenza viruses have a seasonal pattern, thus it is thought that infections may pick up again when the weather turns cooler in China.[38]
In domestic animals
Several domestic species have been infected with and shown symptoms of H5N1 viral infection, including cats, dogs, ferrets, pigs, and birds.[39]
Birds
Attempts are made in the United States to minimize the presence of HPAI in poultry through routine surveillance of poultry flocks in commercial poultry operations. Detection of a HPAI virus may result in immediate culling of the flock. Less pathogenic viruses are controlled by vaccination, which is done primarily in turkey flocks (ATCvet codes: QI01AA23 for the inactivated fowl vaccine, QI01CL01 for the inactivated turkey combination vaccine).[40]
Seals
A recent strain of the virus is able to infect the lungs of seals[41]
Cats
Avian influenza in cats can show a variety of symptoms and usually lead to death. Cats are able to get infected by either consuming an infected bird or by contracting the virus from another infected cat.
Influenza prevention
People who have fewer chances to contact with birds do not belong to the high-risk group of HPAI. If people take precautions correctly and be more careful, the chance of infection will be very low, even among farmers.
In the aware of bird flu pandemic, people should have careful thought to adopt suitable Infection Control Procedures. Try to avoid flu infection in any situation will be necessary. Protecting eyes, nose, mouth and hands from virus particles will be a major priority because these are the most common passageways for a flu virus to transfer into the body.[42] Bird flu virus particles may also be transferred through clothing or even shoes. The final step is people should always have sanitized hands in order to further reduce the chances of cross-contamination. Any unprotected clothing or footwear should be disinfected. Avoid contact with poultry, and maintaining good personal hygiene is very important, too. Someone who has normal flu should be more careful in avoiding contact with fowl because the epidemic situation will become even more serious if the receptor protein of normal flu and the genes of Avian Flu combine with each other.[42]
In popular culture
An episode of Angry Birds Toons had the nickname of the disease and has the birds and pigs sick.
See also
- H7N9
- Global spread of H5N1
- H5N1
- Health crisis
- Influenza
- Influenzavirus A
- Influenza pandemic
- Influenza Genome Sequencing Project
- Influenza research
- Influenza vaccine
- International Partnership on Avian and Pandemic Influenza
- OIE/FAO Network of Expertise on Avian Influenza
- Pandemic Preparedness and Response Act
- Subtypes of Influenza A virus
- Transmission and infection of H5N1
References
- ↑ "Avian influenza strains are those well adapted to birds"EUROPEAN CENTRE FOR DISEASE PREVENTION AND CONTROL.
- ↑ Chapter Two : Avian Influenza by Timm C. Harder and Ortrud Werner in Influenza Report 2006
- ↑ Large-scale sequencing of human influenza reveals the dynamic nature of viral genome evolution Nature magazine presents a summary of what has been discovered in the Influenza Genome Sequencing Project.
- ↑ Avian Influenza A (H5N1) Infection in Humans by The Writing Committee of the World Health Organization (WHO) Consultation on Human Influenza A/H5 in the September 29, 2005 New England Journal of Medicine
- ↑ The Threat of Pandemic Influenza: Are We Ready? Workshop Summary (2005) Full text of online book by INSTITUTE OF MEDICINE OF THE NATIONAL ACADEMIES
- ↑ CDC has a phylogenetic tree showing the relationship between dozens of highly pathogenic varieties of the Z genotype of avian flu virus H5N1 and ancestral strains.
- ↑ Hiromoto, Y.; Yamazaki, Y.; Fukushima, T.; Saito, T.; Lindstrom, S. E.; Omoe, K.; Nerome, R.; Lim, W.; Sugita, S.; Nerome, K. (2000). "Evolutionary characterization of the six internal genes of H5N1 human influenza a virus". The Journal of general virology 81 (Pt 5): 1293–1303. PMID 10769072.
- ↑ Monke, Jim. "Avian Influenza: Agricultural Issues." CRS Report for Congress. RS21747. August 29, 2006.
- ↑ China reports second bird flu death in a month - Health - Cold and flu - msnbc.com
- ↑ Rudi Hendrikx, DVM. "Avian Influenza in Pigeons" (PDF). Retrieved 2014-02-06.
- ↑ Panigrahy B, Senne DA, Pedersen JC, Shafer AL, Pearson JE (1996). "Susceptibility of pigeons to avian influenza". Avian Diseases 40 (3): 600–4. doi:10.2307/1592270. PMID 8883790.
- ↑ Perkins LE, Swayne DE (2002). "Pathogenicity of a Hong Kong-origin H5N1 highly pathogenic avian influenza virus for emus, geese, ducks, and pigeons". Avian Diseases 46 (1): 53–63. doi:10.1637/0005-2086(2002)046[0053:poahko]2.0.co;2. PMID 11924603.
- ↑ "First Human Avian Influenza A (H5N1) Virus Infection Reported in Americas". CDC. January 8, 2014. Retrieved 10 January 2014.
- ↑ "Thousands of birds dead from avian flu in B.C.". CTV. December 2, 2014. Retrieved 2 December 2014.
- ↑ Hiromoto, Yasuaki. "Evolutionary characterization of the six internal genes of H5N1 human influenza A virus". Journal of General Virology. Retrieved 2013-04-20.
- ↑ Leong HK, Goh CS, Chew ST et al. (June 2008). "Prevention and control of avian influenza in Singapore" (PDF). Ann. Acad. Med. Singap. 37 (6): 504–9. PMID 18618063. Retrieved 2009-04-15.
- ↑ "China reports first human H10N8 avian flu death - CNN.com". CNN. 18 December 2013.
- ↑ Cox, N.; Kawaoka (1998). "22". In Mahy B. and Collier L. Topley and Wilson's Microbiology and Microbial Infections. 1 Virology. Y. (9 ed.). Arnold. p. 415. ISBN 0-340-61470-6.
- ↑ 19.0 19.1 Blanchard, Ben. "China says son likely infected father with bird flu." Reuters 10 Jan 2008.
- ↑ Chapter Two : Avian Influenza by Timm C. Harder and Ortrud Werner
- ↑ Webster, R. G. and Walker, E. J. (2003). "The world is teetering on the edge of a pandemic that could kill a large fraction of the human population". American Scientist 91 (2): 122. doi:10.1511/2003.2.122.
- ↑ World Health Organization. (2006). Avian influenza (" bird flu") – The Disease in Humans. Retrieved April 6, 2006.
- ↑ "Bird Flu Claims More Lives In Shanghai". Forbes.
- ↑ "Cumulative number of confirmed human cases for avian influenza A(H5N1) reported to WHO, 2003-2012" (PDF). World Health Organization. Retrieved 5 September 2012.
- ↑ Kullman, Greg et al. (May 2008). "Protecting Poultry Workers from Avian Influenza (Bird Flu)". NIOSH Alert: Publication No. 2008-128. National Institute for Occupational Safety and Health. Archived from the original on 10 January 2009. Retrieved December 18, 2008.
- ↑ Tiensn, Thanawat et al. "Highly Pathogenic Avian Influenza H5N1 Thailand, 2004.". Emerging Infectious Disease. 2005. CDC. 11 (11): 1661–1672.
- ↑ "The fight against bird flu". Nature 496 (7446): 397. April 24, 2013. doi:10.1038/496397a. PMID 23627002. Retrieved 25 April 2013.
- ↑ Li, Q.; Zhou, L.; Zhou, M.; Chen, Z.; Li, F.; Wu, H.; Xiang, N.; Chen, E. et al. (April 24, 2013). "Preliminary Report: Epidemiology of the Avian Influenza A (H7N9) Outbreak in China". New England Journal of Medicine 370 (6): 520–32. doi:10.1056/NEJMoa1304617. PMID 23614499. Archived from the original on May 2, 2013. Retrieved April 25, 2013.
- ↑ Gallagher, James (May 3, 2013). "Q&A: H7N9 bird flu". BBC News. Retrieved May 4, 2013.
- ↑ Shadbolt, Peter (April 25, 2013). "WHO: H7N9 virus 'one of the most lethal so far'". CNN. Retrieved 25 April 2013.
- ↑ "Frequently Asked Questions on human infection with influenza A(H7N9) virus, China". World Health Organization. 5 April 2013. Retrieved 9 April 2013.
- ↑ "OIE expert mission finds live bird markets play a key role in poultry and human infections with influenza A(H7N9)". Paris: World Organisation for Animal Health. April 30, 2013. Retrieved May 2, 2013.
- ↑ Study puts troubling traits of H7N9 avian flu virus on display (July 10, 2013)
- ↑ Arima, Y.; Zu, R.; Murhekar, M.; Vong, S.; Shimada, T. (2013). "Human infections with avian influenza A(H7N9) virus in China: preliminary assessments of the age and sex distribution". Western Pacific Surveillance and Response Journal (WHO) 4 (2). doi:10.5365/wpsar.2013.4.2.005.
- ↑ Skowronski, DM; Janjua, NZ; Kwindt, TL; De Serres, G (25 April 2013). "Virus-host interactions and the unusual age and sex distribution of human cases of influenza A(H7N9) in China, April 2013". Eurosurveillance (European Centre for Disease Prevention and Control) 18 (17). Retrieved 3 May 2013.
- ↑ Experts: Past exposures may help explain H7N9 age profile, Center for Infectious Disease Research & Policy, University of Minnesota, April 26, 2013.
- ↑ Schnirring, Lisa (April 1, 2013). "China reports three H7N9 infections, two fatal". CIDRAP News. Retrieved May 4, 2013.
- ↑ Avian Influenza A H7N9 - CDC
- ↑ National Wildlife Health Center, "List of Species Affected by H5N1 (Avian Influenza)," USGS 10 May 2010
- ↑ Thacker E, Janke B (February 2008). "Swine influenza virus: zoonotic potential and vaccination strategies for the control of avian and swine influenzas". The Journal of Infectious Diseases. 197 Suppl 1: S19–24. doi:10.1086/524988. PMID 18269323.
- ↑ & Bronchioles. "Bird flu has jumped to baby seals, scientists discover". CNN. 31 July 2012. Retrieved 31 July 2012.
- ↑ 42.0 42.1 衛生署疾病管制局一般民眾版
Orent, Wendy. "The Science of Avian Flu, Answers to Nine Frequently Asked Questions." Discover. February 2006. 59-61.
External links
| Wikimedia Commons has media related to Avian influenza. |
| Wikinews has related news: Six-year-old Egyptian boy contracts bird flu |
| Wikinews has related news: Category:Avian Flu |
- International
- United Nations System Coordinator for Avian and Human Influenza (UNSIC).
- World Health Organisation (WHO)
- WHO Avian influenza resource
- The United Nation's World Health Organization's Avian Flu Facts Sheet for 2006
- In-depth analysis of bird flu Symptoms & in-depth analysis on avian flu
- Food and Agriculture Organization of the UN (FAO)
- FAO Avian Influenza portal Information resources, animations, videos, photos
- FAO Bird Flu disease card
- World Organisation for Animal Health (OIE)
- Current status of HPAI worldwide at OIE. WAHID Interface - OIE World Animal Health Information Database
- Disease card
- Avian influenza resource By Dr. Nati Elkin - Atlases, vaccines and information.
- United States
- PandemicFlu.Gov U.S. Government avian and pandemic flu information
- CIDRAP Avian Flu Overview "Avian Influenza (Bird Flu): Agricultural and Wildlife Considerations"
- US Avian Influenza Response U.S. Agency for International Development (USAID)
- Avian influenza research and recommendations National Institute for Occupational Safety and Health
- Influenza Research Database Database of influenza sequences and related information.
- Wildlife Disease Information Node A part of the National Biological Information Infrastructure and partner of the NWHC, this agency collects and distributes news and information about wildlife diseases such as avian influenza and coordinates collaborative information sharing efforts.
- Avian Influenza information AVMA - The American Veterinary Medical Association.
- Species Profile- Avian Influenza (Orthomyxoviridae Influenza Type A, subtype H5N1), National Invasive Species Information Center, United States National Agricultural Library. Lists general information and resources for Avian Influenza.
- Strategic Health Communication for Avian and Pandemic Influenza Prevention Johns Hopkins Bloomberg School of Public Health Center for Communication Programs Global Program on Avian and Pandemic Influenza.
- Avian Influenza: Critical Program Issues Global Health Technical Brief on Avian Influenza.
- Europe
- Health-EU Portal EU response to Avian Influenza.
- Avian Influenza: Prevention and Control Proceedings of the Frontis workshop on Avian Influenza: Prevention and Control, Wageningen, The Netherlands
- Avian Influenza: Questions & Answers European Centre for Disease Prevention and Control - Official website
- FluTrop: Avian Influenza Research in Tropical Countries French Agricultural Research Center for Developing Countries (CIRAD), Avian Influenza website
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||