Airway pressure release ventilation



Airway pressure release ventilation (APRV) is a pressure control mode of mechanical ventilation that utilizes an inverse ratio ventilation strategy. APRV is an applied continuous positive airway pressure (CPAP) that at a set timed interval releases the applied pressure. Depending on the ventilator manufacturer, it may be referred to as BiVent. This is just as appropriate to use, since the only difference is that the term APRV is copyrighted.
History
Airway pressure release ventilation was described initially by Stock and Downs in 1987[2][3] as a continuous positive airway pressure (CPAP) with an intermittent release phase. APRV begins at a pressure higher than the baseline pressure and follows with a deflation to accomplish tidal ventilation.[4] Fundamentally APRV is a time-cycled alternant between two levels of positive airway pressure, with the main time on the high level and a brief expiratory release to facilitate ventilation.[5]
Indications
Based on clinical and experimental data, airway pressure release ventilation is indicated in patients with acute lung injury,[6][7] acute respiratory distress syndrome[8][9] and atelectasis[1] after major surgery
Inverse ratio ventilation
This is a type of inverse ratio ventilation.[10] The exhalation time (Tlow) is shortened to usually less than one second to maintain alveoli inflation. Fundamentally this is a continuous pressure with a brief release. APRV currently the most efficient conventional mode for lung protective ventilation.[11][12][13]
Settings and measurements

Settings are sometimes brand specific and the term for the individual settings may differ, however generally the settings listed here are a fundamental explanation of the purpose of the settings within the APRV mode.
- Phigh — This is the inspiratory pressure (just like in pressure control).
- Thigh — This value is the number of seconds during the inhalation phase.
- Tpeep — Also known as the Tlow, this is the time allotted for expiration.
- FiO2 — The fractional O2 percentage that is being added to the delivered air.
Mean airway pressure
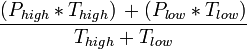
Mean airway pressure on APRV is calculated by this formula:[1]
Perceptions and receptions
Different perceptions of this mode may exist around the globe. While 'APRV' is common to users in North America, a very similar mode, biphasic positive airway pressure (BIPAP), was introduced in Europe.[14] The term APRV has also been used in American journals where, from the ventilation characteristics, BIPAP would have been the appropriate terminology.[15] To further confusion, BiPAP© is a registered trade-mark for a noninvasive ventilation mode in a specific ventilator (Respironics Inc.). Other names (BILEVEL, DUOPAP, BIVENT) have been created for legal reasons. Although similar in modality, these terms describe how a mode is intended to inflate the lung, rather than defining the characteristics of synchronization or the way spontaneous breathing efforts are supported.[8][16]
Other terms
APRV is used by many brands and models of mechanical ventilators under different names. Most names are copyrighted as trademarks and do not represent nomenclature of mechanical ventilation but may be referred to clinically by the brand name.
Some of these names include:
- BiVent - (Servo-i ventilator by Maquet)
- BiLevel - (Puritan Bennett 840 ventilator by Covidien)
- DuoPAP - ( C-1 ventilator by Hamilton)
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Daoud EG (2007). "Airway pressure release ventilation.". Ann Thorac Med 2 (4): 176–9. doi:10.4103/1817-1737.36556. PMC 2732103. PMID 19727373.
- ↑ Downs JB, Stock MC (1987). "Airway pressure release ventilation: a new concept in ventilatory support.". Critical Care Medicine 15 (5): 459–61. doi:10.1097/00003246-198705000-00001. PMID 3568710.
- ↑ Stock MC, Downs JB, Frolicher DA (1987). "Airway pressure release ventilation.". Critical Care Medicine 15 (5): 462–6. doi:10.1097/00003246-198705000-00002. PMID 3552443.
- ↑ Frawley, PM; Habashi, NM (2001). "Airway pressure release ventilation: Theory and practice". AACN Clin Issues 12: 234–46.
- ↑ Dietrich Henzler (2011). "What on earth is APRV?". Critical care (London, England) 15 (1): 115. doi:10.1186/cc9419. PMC 3222047. PMID 21345265.
- ↑ Hering R, Zinserling J, Wrigge H, Varelmann D, Berg A, Kreyer S et al. (2005). "Effects of spontaneous breathing during airway pressure release ventilation on respiratory work and muscle blood flow in experimental lung injury.". Chest 128 (4): 2991–8. doi:10.1378/chest.128.4.2991. PMID 16236977.
- ↑ Wrigge H, Zinserling J, Neumann P, Defosse J, Magnusson A, Putensen C et al. (2003). "Spontaneous breathing improves lung aeration in oleic acid-induced lung injury.". Anesthesiology 99 (2): 376–84. doi:10.1097/00000542-200308000-00019. PMID 12883410.
- ↑ 8.0 8.1 Putensen C, Mutz NJ, Putensen-Himmer G, Zinserling J (1999). "Spontaneous breathing during ventilatory support improves ventilation-perfusion distributions in patients with acute respiratory distress syndrome.". Am J Respir Crit Care Med 159 (4 Pt 1): 1241–8. doi:10.1164/ajrccm.159.4.9806077. PMID 10194172.
- ↑ Kaplan LJ, Bailey H, Formosa V (2001). "Airway pressure release ventilation increases cardiac performance in patients with acute lung injury/adult respiratory distress syndrome.". Crit Care 5 (4): 221–6. PMC 37408. PMID 11511336.
- ↑ Kaplan LJ. Bailey H. Formosa V. “Airway pressure release ventilation increases cardiac performance in patients with acute lung injury/adult respiratory distress syndrome” Critical Care (London). 5(4):221-6, 2001 Aug.
- ↑ Adrian A. Maung & Lewis J. Kaplan (July 2011). "Airway pressure release ventilation in acute respiratory distress syndrome". Critical care clinics 27 (3): 501–509. doi:10.1016/j.ccc.2011.05.003. PMID 21742214.
- ↑ Sydow M, Burchardi H, Ephraim E, Zielmann S, Crozier TA (1994). "Long-term effects of two different ventilatory modes on oxygenation in acute lung injury. Comparison of airway pressure release ventilation and volume-controlled inverse ratio ventilation.". Am J Respir Crit Care Med 149 (6): 1550–6. doi:10.1164/ajrccm.149.6.8004312. PMID 8004312.
- ↑ Räsänen J, Cane RD, Downs JB, Hurst JM, Jousela IT, Kirby RR et al. (1991). "Airway pressure release ventilation during acute lung injury: a prospective multicenter trial.". Critical Care Medicine 19 (10): 1234–41. doi:10.1097/00003246-199110000-00004. PMID 1914479.
- ↑ M. Baum, H. Benzer, C. Putensen, W. Koller & G. Putz (September 1989). "[Biphasic positive airway pressure (BIPAP)--a new form of augmented ventilation]". Der Anaesthesist 38 (9): 452–458. PMID 2686487.
- ↑ C. Putensen, S. Zech, H. Wrigge, J. Zinserling, F. Stuber, T. Von Spiegel & N. Mutz (July 2001). "Long-term effects of spontaneous breathing during ventilatory support in patients with acute lung injury". American journal of respiratory and critical care medicine 164 (1): 43–49. doi:10.1164/ajrccm.164.1.2001078. PMID 11435237.
- ↑ Wrigge H, Zinserling J, Hering R, Schwalfenberg N, Stüber F, von Spiegel T et al. (2001). "Cardiorespiratory effects of automatic tube compensation during airway pressure release ventilation in patients with acute lung injury.". Anesthesiology 95 (2): 382–9. doi:10.1097/00000542-200108000-00020. PMID 11506110.
Daoud EG, Farag HL, Chatburn RL (2012). "Airway pressure release ventilation: what do we know?". Respir Care 57 (2): 282–92. doi:10.4187/respcare.01238. PMID 21762559.
| ||||||||||||||||||||||||||||||||||||||||||||