Abfraction

Abfraction or theory of abfraction is a theory explaining non-carious cervical lesions (NCCL). It suggests that they are caused by flexural forces, usually from cyclic loading; the enamel, especially at the cementoenamel junction (CEJ), undergoes this pattern of destruction by separating the enamel rods.
As teeth flex under pressure, the arrangement of teeth touching each other, known as occlusion, causes tension on one side of the tooth and compression on the other side of the tooth. This is believed to cause V-shaped depressions on the side under tension and C-shaped depressions on the side under compression.
This theory of abfraction is disputed by some who think that these types of enamel lesions are due to over-zealous brushing. Studies by T. C. Abrahamsen have shown that toothpaste (not the toothbrush) is abrasive enough to cause this type of damage if the person is too aggressive in brushing the teeth in a very hard and vigorous "sawing" motion. Abrahamson suggests that the term "toothbrush abrasion" be replaced with the term "toothpaste abuse".
Definition
Abfraction is a form of non-carious tooth tissue loss that occurs along the gingival margin.[1] In simple language, abfraction is a loss of tooth structure that is not caused by tooth decay, located along the gum line. There has been a lot of theoretical evidence to support the concept of abfraction, but little experimental evidence exists.[2]
The term abfraction was first published in the 1991 journal article called "Abfractions: A New Classification of Hard Tissue Lesions of Teeth" by John O. Grippo.[3] This article introduced the definition of abfraction as a "pathologic loss of hard tissue tooth substance caused by bio mechanical loading forces". This helped to establish abfraction as a new form of lesion, differing from abrasion, attrition, and erosion.[1]
Tooth tissue is gradually weakened causing tissue loss through fracture and chipping or successively worn away leaving a non-carious lesion on the tooth surface. These lesions occur in both the dentine and enamel of the tooth. These lesions generally occur around the cervical areas of the dentition.[4]
Signs and symptoms
Abfraction lesions will generally occur in the region on the tooth where the greatest tensile stress is located. In statements such as these there is no comment on whether the lesions occur above or below the CEJ. However, it is assumed that the abfraction lesions will occur anywhere in the cervical areas of affected teeth. It is important to note that studies supporting this configuration of abfraction lesions also state that when there is more than one abnormally large tensile stress on a tooth two or more abfraction lesions can result on the one surface.[2]
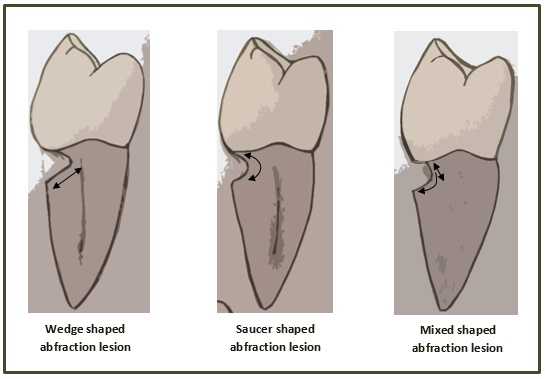
When looking at abfraction lesions there are generally three shapes in which they appear, appearing as either wedge, saucer or mixed patterns .Wedge and saucer shaped lesions are the most common, whereas mixed lesions are less frequently identified in the oral cavity.[5] In reference to figure 1, wedge shaped lesions have the sharpest internal line angles and saucer/mixed shaped lesions are either smooth internally, or a variety.
Clinically, people with abfraction lesions can also present with tooth sensitivity in the associated areas. This occurs because as the abfration lesions appear, dentine/cementum is exposed. The dentine and cementum are less dense than tooth enamel and therefore more susceptible to sensation from thermal/mechanical sources.[6]
Causes
As abfraction is still a controversial theory there are various ideas on what causes the lesions. Because of this controversy the true causes of abfraction also remain disputable.[7] Researchers have proposed that abfraction is caused by forces on the tooth from the teeth touching together, occlusal forces, when chewing and swallowing.[3][8] These lead to a concentration of stress and flexion at the area where the enamel and cementum meet (CEJ).[2][4] This theoretical stress concentration[9] and flexion over time causes the bonds in the enamel of the tooth to break down and either fracture or be worn away from other stressors such as erosion or abrasion.[2][4][7][8] The people who initially proposed the theory of abfraction believe the occlusal forces alone cause the lesions[9] without requiring the added abrasive components such as toothbrush and paste or erosion.[9]
If teeth come together in a non-ideal bite the researchers state that this would create further stress in areas on the teeth.[8] Teeth that come together too soon or come under more load than they are designed for could lead to abfraction lesions.[8] The impacts of restorations on the chewing surfaces of the teeth being the incorrect height has also been raised as another factor adding to the stress at the CEJ.[7]
Further research has shown that the normal occlusal forces from chewing and swallowing are not sufficient to cause the stress and flexion required to cause abfraction lesions.[2] However, these studies have shown that the forces are sufficient in a person who grinds their teeth (bruxism).[2] Several studies have suggested that it is more common among those who grind their teeth,[7][9] as the forces are greater and of longer duration. Yet further studies have shown that these lesions do not always appear in people with bruxism and others without bruxism have these lesions.[4]
There are other researchers who would state that occlusal forces have nothing to do with the lesions along the CEJ and that it is the result of abrasion from toothbrush with toothpaste that causes these lesions.[2][4][7]
Being theoretical in nature there is more than one idea on how abfraction presents clinically in the mouth. One theory of its clinical features suggests that the lesions only form above the cementoenamel junction (CEJ) (which is where the enamel and cementum meet on a tooth).[5][10][11][12] If this is kept in mind, it serves as a platform for it to be distinguished from other non-carious lesions, such as tooth-brush abrasion.
Treatment
Many treatments are available for abfraction, yet treatment of these lesions can be difficult due to the many possible causes. Prior to treatment, it is important that the dental clinician determines the level of activity and predicts possible progression of the lesion. A No.12 scalpel is carefully used by the dental clinician to make a small indentation on the lesion, this is then closely monitored. Loss of a scratch mark signifies that the lesion is active.
It is usually recommended when an abfraction lesion is less than 1millimeter, monitoring at regular intervals is a sufficient treatment option. If there are concerns around aesthetics or clinical consequences such as dentinal hypersensitivity, a dental restoration may be a suitable treatment option.
Aside from restoring the lesion if it is equally important to remove any other possible causative factors. Adjustments to the biting surfaces of the teeth alter the way the upper and lower teeth come together, this may assist by redirecting the occlusal load. The aim of this is to redirect the force of the load to the long axis of the tooth. This can be done by altering cuspal inclines, reducing heavy contacts and removing premature contacts. If bruxism is a deemed a contributing factor an occlusal splint can be effective treatment for eliminating the irregular forces placed on the tooth.
Controversy
Abfraction has been a controversial subject since its creation in 1991.[7] This is due to the clinical presentation of the tooth loss, which often presents in a manner similar to that of abrasion or erosion. The major reasoning behind the controversy is the similarity of abfraction to other non carious lesions and the prevalence of multiple theories to potentially explain the lesion. One of the most prevalent theories is called "the theory of non-carious cervicle lesions" which suggests that tooth flexion occurring due to occlusion factors which impacts on the vulnerable area near the cementoenamel junction.[7] This theory is not widely accepted among the professional community as it suggests that the only factor is occlusion. Many researchers argue that this is inaccurate as they contend that the abfraction lesion is multifactorial (has many causative factors) lesion with other factors such as abrasion or erosion.[4] This controversy around the causative factors, along with the recency of the lesion classification, are some of the reasons why many dental clinicians are looking at the lesion with some scepticism. More research is needed to fully clear up the controversy surrounding the abfraction lesion.
See also
References
- ↑ 1.0 1.1 Bartlett, D.W.; Shah, P (April 2006). "A Critical Review of Non-carious Cervical (Wear) Lesions and the Role of Abfraction, Erosion, and Abrasion". Journal of Dental Research 85 (4): 306–312.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Michael, JA; Townsend, GC; Greenwood, LF; Kaidonis, JA (March 2009). "Abfraction: separating fact from fiction". Australian Dental Journal 54 (1): 2–8. doi:10.1111/j.1834-7819.2008.01080.x.
- ↑ 3.0 3.1 Grippo, John O (January–February 1991). "Abfractions: A New Classification of Hard Tissue Lesions of Teeth". JOURNAL OF ESTHETlC DENTISTRY 3 (1): 14–19.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Sarode, Gargi S; Sarode, Sachin C (May 2013). "Abfraction: A review". Journal of Oral and Maxillofacial Pathology 17 (2): 222–227. doi:10.4103/0973-029X.119788.
- ↑ 5.0 5.1 Hur B, Kim HC, Park JK, Versluis A. Characteristics of non-carious cervical lesions – an ex vivo study using micro computed tomography. Journal of Oral Rehabilitation. 2011;38(6):469-74.
- ↑ Cornelius T. Bamise B, FMCDS; Adeyemi O. Olusile, BDS, MSc; Adeleke O. Oginni BChd, FMCDS. An Analysis of the Etiological and Predisposing Factors Related to Dentin Hypersensitivity. the Journal of Contemporary Dental Practice. 2008;9(5):9.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 Antonelli JR, Hottel TL, Garcia-Godoy F. Abfraction Lesions - Where do They Come From? A Review of the Literature. J Tenn Dent Assoc. 2013; 93(1):14-19
- ↑ 8.0 8.1 8.2 8.3 Grippo JO, Simring M, Coleman TA. Abfraction, Abrasion, Biocorrosion, and the Enigma of Noncarious Cervical Lesions: A 20-Year Perspective. J Esthet Restor Dent. 2012; 24(1):10-23 DOI 10.1111/j.1708-8240.2011.00487.x
- ↑ 9.0 9.1 9.2 9.3 Shetty SM, Shetty RG, Mattigatti S, Managoli NA, Rairam SG, Patil AM. No Carious Cervical Lesions. J Int Oral Health 2013 Sep-Oct; 5(5):142-145
- ↑ Lee HE, Lin CL, Wang CH, Cheng CH, Chang CH. Stresses at the cervical lesion of maxillary premolar—a finite element investigation. Journal of Dentistry.30(7):283-90.
- ↑ Dejak B, Młotkowski A, Romanowicz M. Finite element analysis of stresses in molars during clenching and mastication. Journal of Prosthetic Dentistry.90(6):591-7.
- ↑ Borcic J, Anic I, Smojver I, Catic A, Miletic I, Ribaric SP. 3D finite element model and cervical lesion formation in normal occlusion and in malocclusion. Journal of Oral Rehabilitation. 2005;32(7):504-10.
- Gandara, BK; Truelove, EL (1999). "Diagnosis and management of dental erosion". The journal of contemporary dental practice 1 (1): 16–23. PMID 12167897.
- Summit, James B., J. William Robbins, and Richard S. Schwartz. Fundamentals of Operative Dentistry: A Contemporary Approach. 2nd edition. Carol Stream, Illinois, Quintessence Publishing Co, Inc, 2001. ISBN 0-86715-382-2.
- Lee, WC., Eakle, WS. "Possible role of tensile stress in the etiology of cervical erosive lesions of teeth". Journal of Prosthetic Dentistry (1984) Vol. 52: 374–380.