Vigabatrin
 | |
|---|---|
 | |
| Systematic (IUPAC) name | |
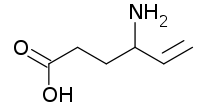
| (RS)-4-aminohex-5-enoic acid | |
| Clinical data | |
| Trade names | Sabril |
| AHFS/Drugs.com | Consumer Drug Information |
| MedlinePlus | a610016 |
| Pregnancy cat. | D (AU) |
| Legal status | Not a controlled substance |
| Routes | Oral |
| Pharmacokinetic data | |
| Bioavailability | 80–90% |
| Protein binding | Nil |
| Metabolism | Almost no metabolic transformation occurs |
| Half-life | 5–8 hours in young adults, 12–13 hours in the elderly. |
| Excretion | Renal |
| Identifiers | |
| CAS number | 60643-86-9 |
| ATC code | N03AG04 |
| PubChem | CID 5665 |
| DrugBank | DB01080 |
| ChemSpider | 5463 |
| UNII | GR120KRT6K |
| KEGG | D00535 |
| ChEMBL | CHEMBL89598 |
| Chemical data | |
| Formula | C6H11NO2 |
| Mol. mass | 129.157 g/mol |
| SMILES
| |
| |
| | |
Vigabatrin is an antiepileptic drug that inhibits the catabolism of gamma-aminobutyric acid (GABA) by irreversibly inhibiting GABA transaminase. It is an analog of GABA, but it is not a receptor agonist.[1] It is sold under the brand name Sabril.
Indications
Epilepsy
In Canada, vigabatrin is approved for use as an adjunctive treatment (with other drugs) in treatment resistant epilepsy, complex partial seizures, secondary generalized seizures, and for monotherapy use in infantile spasms in West syndrome.[1]
As of 2003, vigabatrin is approved in Mexico for the treatment of epilepsy that is not satisfactorily controlled by conventional therapy (adjunctive or monotherapy) or in recently diagnosed patients who have not tried other agents (monotherapy).[2]
Vigabatrin is also indicated for monotherapy use in secondarily generalized tonic-clonic seizures, partial seizures, and in infantile spasms due to West syndrome.[2]
On August 21, 2009, Lundbeck announced that the U.S. Food and Drug Administration had granted two New Drug Application approvals for vigabatrin. The drug is indicated as monotherapy for pediatric patients one month to two years of age with infantile spasms for whom the potential benefits outweigh the potential risk of vision loss, and as adjunctive (add-on) therapy for adult patients with refractory complex partial seizures (CPS) who have inadequately responded to several alternative treatments and for whom the potential benefits outweigh the risk of vision loss.
In 1994, Feucht and Brantner-Inthaler reported that vigabatrin reduced seizures by 50-100% in 85% of children with Lennox-Gastaut syndrome who had poor results with a valproate.[3]
Substance dependence
Fechtner et al. found in an eight week study that vigabatrin was effective in the treatment of cocaine and/or methamphetamine dependence. Twenty-eight subjects were enrolled; twenty stayed after the escalation phase and out of those, eighteen completed the study and follow-up. Out of those, sixteen subjects tested negative for cocaine and methamphetamine during the last six weeks. No ocular adverse effects were noted.[4]
Other
Vigabatrin reduced cholecystokinin tetrapeptide-induced symptoms of panic disorder, in addition to elevated cortisol and ACTH levels, in healthy volunteers.[5]
Vigabatrin is also used to treat seizures in succinic acid semialdehyde deficiency, which is an inborn neurotransmitter (gamma amino butyric acid) catabolism defect that causes mental retardation, hypotonia, seizures, speech disturbance, and ataxia through the accumulation of 4-hydroxybutyric acid. Vigabatrin inhibits the formation of succinic acid semialdehyde through GABA transaminase inhibition. However, this is in the brain only; it has no effect on peripheral GABA transaminase, so the 4-hydroxybutyric acid keeps building up and eventually reaches the brain.[6]
Mechanism of action
Vigabatrin is an irreversible suicide inhibitor of gamma-aminobutyric acid transaminase (GABA-T), the enzyme responsible for the catabolism of GABA, which increases the level of GABA in the brain.[1][7] Vigabatrin is a racemic compound, and its [S]-enantiomer is pharmacologically active.[8],[9]
Adverse effects
Central nervous system
Out of 2,081 subjects, somnolence (12.5%), headache (3.8%), dizziness (3.8%), nervousness (2.7%), depression (2.5%), memory disturbances (2.3%), diplopia (2.2%), aggression (2.0%), ataxia (1.9%), vertigo (1.9%), hyperactivity (1.8%), vision abnormalities (1.6%), confusion (1.4%), insomnia (1.3%), impaired concentration (1.2%), personality disorder (1.1%).[1] Out of 299 children, 33 (11%) became hyperactive.[1]
Some patients develop psychosis during the course of vigabatrin therapy,[10] which is more common in adults than in children.[11] This can happen even in patients with no prior history of psychosis.[12] Other rare CNS side effects include anxiety, emotional lability, irritability, tremor, abnormal gait, and speech disorder.[1]
Gastrointestinal
Abdominal pain (1.6%), constipation (1.4%), vomiting (1.4%), and nausea (1.4%). Dyspepsia and increased appetite occurred in less than 1% of subjects in clinical trials.[1]
Body as a Whole
Fatigue (9.2%), weight gain (5.0%), asthenia (1.1%).[1]
Teratogenicity
A teratology study conducted in rabbits found that a dose of 150 mg/kg/day caused cleft palate in 2% of pups and a dose of 200 mg/kg/day caused it in 9%.[1] This may be due to a decrease in methionine levels, according to a study published in March 2001.[13] In 2005, a study conducted at the University of Catania was published stating that rats whose mothers had consumed 250–1000 mg/kg/day had poorer performance in the water maze and open-field tasks, rats in the 750-mg group were underweight at birth and did not catch up to the control group, and rats in the 1000 mg group did not survive pregnancy.[14]
There is no controlled teratology data in humans to date.
Sensory
In 2003, vigabatrin was shown by Frisén and Malmgren to cause irreversible diffuse atrophy of the retinal nerve fiber layer in a retrospective study of 25 patients.[15] This has the most effect on the outer area (as opposed to the macular, or central area) of the retina.[16] Visual field defects had been reported as early as 1997 by Tom Eke and others, in the UK. Some authors, including Comaish et al. believe that visual field loss and electrophysiological changes may be demonstrable in up to 50% of Vigabatrin users.
The retinal toxicity of vigabatrin can be attributed to a taurine depletion.[17]
Drug interactions
A study published in 2002 found that vigabatrin causes a statistically significant increase in plasma clearance of carbamazepine.[18]
In 1984, Drs Rimmer and Richens at the University of Wales reported that administering vigabatrin with phenytoin lowered the serum phenytoin concentration in patients with treatment-resistant epilepsy.[19] Five years later, the same two scientists reported a fall in concentration of phenytoin of 23% within five weeks in a paper describing their failed attempt at elucidating the mechanism behind this interaction.[20]
Pharmacokinetics
With most drugs, elimination half-life is a useful predictor of dosing schedules and the time needed to reach steady state concentrations. In the case of vigabatrin, however, it has been found that the half-life of biologic activity is far longer than the elimination half-life.[21]
For vigabatrin, there is no range of target concentrations because researchers found no difference between the serum concentration levels of responders and those of non-responders.[22] Instead, the duration of action is believed to be more a function of the GABA-T resynthesis rate; levels of GABA-T do not usually return to their normal state until six days after stopping the medication.[9]
Brand names
Vigabatrin is sold as Sabril in Canada,[23] Mexico,[2] and the United Kingdom.[24] The brand name in Denmark is Sabrilex. Sabril was approved in the United States on August 21, 2009 and is currently marketed in the U.S. by Lundbeck Inc., which acquired Ovation Pharmaceuticals, the U.S. sponsor in March 2009.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Long, Phillip W. "Vigabatrin." Internet Mental Health. 1995–2003.
- ↑ 2.0 2.1 2.2 DEF MEXICO: SABRIL Diccionario de Especialdades Farmaceuticas. Edicion 49, 2003.
- ↑ Feucht M, Brantner-Inthaler S (1994). "Gamma-vinyl-GABA (vigabatrin) in the therapy of Lennox-Gastaut syndrome: an open study" (PDF). Epilepsia 35 (5): 993–8. doi:10.1111/j.1528-1157.1994.tb02544.x. PMID 7925171. Retrieved 2006-05-25.
- ↑ Fechtner, Robert D.; Albert S. Khouri, Emilia Figueroa, Marina Ramirez, MD; Martha Federico, Stephen L. Dewey, Jonathan D. Brodie (September 2006). "Short-term Treatment of Cocaine and/or Methamphetamine Abuse With Vigabatrin: Ocular Safety Pilot Results". Archives of Ophthalmology 124 (9): 1257–62. doi:10.1001/archopht.124.9.1257. PMID 16966620. Retrieved 2007-10-20.
- ↑ Zwanzger P, Baghai TC, Schuele C, Strohle A, Padberg F, Kathmann N, Schwarz M, Moller HJ, Rupprecht R (2001). "Vigabatrin decreases cholecystokinin-tetrapeptide (CCK-4) induced panic in healthy volunteers". Neuropsychopharmacology 25 (5): 699–703. doi:10.1016/S0893-133X(01)00266-4. PMID 11682253.
- ↑ Pearl, Phillip L; Robbins, Emily; Capp, Philip K; Gasior, Maciej; Gibson, K Michael (May 5, 2004). "Succinic Semialdehyde Dehydrogenase Deficiency". GeneReviews. Seattle, Washington: University of Washington. Retrieved 9-6-2010.
- ↑ Rogawski MA, Löscher W. (2004). "The neurobiology of antiepileptic drugs.". Nat Rev Neurosci 5 (7): 553–564. doi:10.1038/nrn1430. PMID 15208697.
- ↑ Sheean, G.; Schramm T, Anderson DS, Eadie MJ. (1992). "Vigabatrin--plasma enantiomer concentrations and clinical effects". Clinical and Experimental Neurology 29: 107–16. PMID 1343855.
- ↑ 9.0 9.1 Gram L, Larsson OM, Johnsen A, Schousboe A (1989). "Experimental studies of the influence of vigabatrin on the GABA system". British Journal of Clinical Pharmacology 27 (Suppl 1): 13S–17S. PMC 1379673. PMID 2757904.
- ↑ Sander JW, Hart YM (1990). "Vigabatrin and behaviour disturbance". Lancet 335 (8680): 57. doi:10.1016/0140-6736(90)90190-G. PMID 1967367.
- ↑ Chiaretti A, Castorina M, Tortorolo L, Piastra M, Polidori G (1994). "[Acute psychosis and vigabatrin in childhood]". La Pediatria Medica e Chirurgica : Medical and surgical pediatrics 16 (5): 489–90. [Article in Italian] PMID 7885961
- ↑ Sander JW, Hart YM, Trimble MR, Shorvon SD (1991). "Vigabatrin and psychosis". Journal of Neurology, Neurosurgery, and Psychiatry 54 (5): 435–9. doi:10.1136/jnnp.54.5.435. PMC 488544. PMID 1865207.
- ↑ Abdulrazzaq YM, Padmanabhan R, Bastaki SM, Ibrahim A, Bener A (2001). "Placental transfer of vigabatrin (gamma-vinyl GABA) and its effect on concentration of amino acids in the embryo of TO mice". Teratology 63 (3): 127–33. doi:10.1002/tera.1023. PMID 11283969.
- ↑ Lombardo SA, Leanza G, Meli C, Lombardo ME, Mazzone L, Vincenti I, Cioni M (2005). "Maternal exposure to the antiepileptic drug vigabatrin affects postnatal development in the rat". Neurological Sciences 26 (2): 89–94. doi:10.1007/s10072-005-0441-6. PMID 15995825.
- ↑ Frisén L, Malmgren K (2003). "Characterization of vigabatrin-associated optic atrophy". Acta Ophthalmologica Scandinavica 81 (5): 466–73. doi:10.1034/j.1600-0420.2003.00125.x. PMID 14510793.
- ↑ Buncic JR, Westall CA, Panton CM, Munn JR, MacKeen LD, Logan WJ (2004). "Characteristic retinal atrophy with secondary "inverse" optic atrophy identifies vigabatrin toxicity in children". Ophthalmology 111 (10): 1935–42. doi:10.1016/j.ophtha.2004.03.036. PMID 15465561.
- ↑ (English) Gaucher D, Arnault E, Husson Z et al. Taurine deficiency damages retinal neurones: cone photoreceptors and retinal ganglion cells. Amino Acids. 2012 Nov;43(5):1979–93. doi:10.1007/s00726-012-1273-3. PMID 22476345. This is an open access article, distributed under the terms of the Creative Commons Attribution License.
- ↑ Sanchez-Alcaraz, Agustín; Quintana MB, Lopez E, Rodriguez I, Llopis P (2002). "Effect of vigabatrin on the pharmacokinetics of carbamazepine". Journal of Clinical Pharmacology and Therapeutics 27 (6): 427–30. doi:10.1046/j.1365-2710.2002.00441.x. PMID 12472982.
- ↑ Rimmer EM, Richens A (1984). "Double-blind study of gamma-vinyl GABA in patients with refractory epilepsy". Lancet 1 (8370): 189–90. doi:10.1016/S0140-6736(84)92112-3. PMID 6141335.
- ↑ Rimmer EM, Richens A (1989). "Interaction between vigabatrin and phenytoin". British Journal of Clinical Pharmacology 27 (Suppl 1): 27S–33S. PMC 1379676. PMID 2757906.
- ↑ Browne TR (1998). "Pharmacokinetics of antiepileptic drugs". Neurology 51 (5 suppl 4): S2–7. PMID 9818917.
- ↑ Lindberger M, Luhr O, Johannessen SI, Larsson S, Tomson T (2003). "Serum concentrations and effects of gabapentin and vigabatrin: observations from a dose titration study". Therapeutic Drug Monitoring 25 (4): 457–62. doi:10.1097/00007691-200308000-00007. PMID 12883229.
- ↑ drugs.com Vigabatrin Drug Information
- ↑ Treatments for Epilepsy - Vigabatrin Norfolk and Waveney Mental Health Partnership NHS Trust
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||