Vaginal flora
The micro-organisms that colonize the vagina, collectively referred to as the vaginal microbiota or vaginal microflora, were discovered by the German gynecologist Albert Döderlein in 1892. The amount and type of bacteria present have significant implications for a woman's overall health. The primary colonizing bacteria of a healthy individual are of the genus lactobacillus,[1] such as L. crispatus, and the lactic acid they produce (some species produce hydrogen peroxide or antibiotic), in combination with fluids secreted during sexual arousal, are greatly responsible for the characteristic scent associated with the vaginal area.
Vaginal microflora
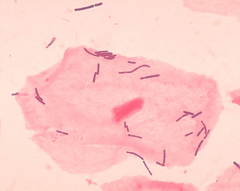
Lactobacilli
The primary colonizing bacteria of a healthy individual are of the genus lactobacillus.[1] Since the first description of lactobacilli by Döderlein, lactobacilli have been generally considered as the gatekeepers of the vaginal ecosystem. Lactobacilli have been shown to inhibit in vitro growth of pathogenic microorganisms, e.g. Bacteroides fragilis, Escherichia coli, Gardnerella vaginalis, Mobiluncus spp., Neisseria gonorrhoeae, Peptostreptococcus anaerobius, P. bivia and Staphylococcus aureus. It is generally accepted that this is achieved through the action of lactic acid primarily.[2][3][4][5] Moreover, lactobacilli ensure long-term colonization of the vagina through adherence to vaginal epithelial cells, blocking the adherence of bacterial pathogens to the vaginal epithelium.[6] Next to lactic acid production and competition for adherence, other antagonistic mechanisms consist of hydrogen peroxide (broad-spectrum antimicrobial) and bacteriocin (targetspecific antimicrobials) production.[7][8][9][10][11][12]
The production of lactic acid
Low pH is generally accepted to be the main mechanism controlling the composition of the vaginal microflora. Although the lactic acid produced by lactobacilli contributes to the vaginal acidity, it is still not proven to be the primary source of low vaginal pH, but the fact remains that most lactobacilli thrive best at a pH < 4.5 .[8][13][14]
Hydrogen peroxide
Production of H2O2 is a well-known mechanism for bacterial antagonism [15][16][17] , inhibiting growth of microorganisms via direct interaction or via human myeloperoxidase.[18][19][20] Hydrogen peroxide-producing lactobacilli have been shown to inactivate HIV-1, herpes simplex virus type 2 (HSV-2), Trichomonas vaginalis, G. vaginalis, P. bivia and E. coli.[10][19][21][22][23][24][25][26] Eschenbach et al.[18] found that 96% of Lactobacillus species from a healthy vaginal ecosystem produced H2O2 (L. jensenii and L. vaginalis produce the highest levels of H2O2,[9][27] whereas only 6% of the lactobacilli recovered from women with BV produced H2O2.[18] In agreement with this, L. iners, most frequently associated with disturbed vaginal microflora,[28][29] is a poor producer of H2O2.[30][31] Vaginal colonization by H2O2-producing lactobacilli has been associated with a decrease in the occurrence of Bacterial vaginosis (BV).[32] However, more recently O‘Hanlon et al.[33] demonstrated that cervicovaginal fluid and semen have a significant H2O2-blocking activity and they later [10] demonstrated that physiological concentrations of H2O2 below 100 μM fail to inactivate any of the 17 tested BV-associated bacteria, e.g. A. vaginae, G. vaginalis, Mobiluncus spp., P. bivia, Prevotella corporis, Mycoplasma hominis, even in the presence of human myeloperoxidase, known to increase the microbicidal activity of H2O2.[10] Only supraphysiologic concentrations of exogenous H2O2 (0.34% w/v, 100 mM) were sufficient to inactivate BV-associated bacteria at which concentration it more potently inactivated vaginal lactobacilli (L. crispatus, L. gasseri, L. iners and L. jensenii). A concentration of 100 mM H2O2 is approximately 50-fold higher than lactobacilli are capable of producing even under optimal aerobic, low-antioxidant conditions, and approximately 5,000-fold higher than the estimated H2O2 concentration in vivo. Even more remarkable, the addition of only 1% vaginal fluid blocked the microbicidal activity of 1 M H2O2. Possible explanations may be that cervicovaginal fluid and semen contain proteins, glycoproteins, polysaccharides, lipids, and other molecules with the potential to react with and inactivate H2O2. In addition, the vagina is hypoxic most of the time, whereas lactobacilli require oxygen to produce hydrogen peroxide. It is also remarkable that catalase, which provides bacteria protection against toxic H2O2, is absent in lactobacilli,[18][21] and as such they would be unprotected against their own H2O2 production. In contrast, under optimal anaerobic growth conditions, physiological concentrations of lactic acid inactivated the BV-associated pathogens without affecting the vaginal lactobacilli.[10][33] In summary, although the hydrogen peroxide production of lactobacilli has been considered as an important antimicrobial component, contributing to the colonization resistance provided by lactobacilli,[9][12] and although there seems to be a link between H2O2-producing lactobacilli and normal vaginal microflora, recent data do not support this role for H2O2.[10][33]
Bacteriocins
Vaginal lactobacilli produce several target specific antimicrobial peptides, i.e. bacteriocins such as lactocin 160 and crispasin A [8] ,[34][35][36] with inhibitory activity ranging from narrow (closely related Lactobacillus species) [37] to broad (diverse groups of bacteria, including G. vaginalis and P. bivia),[4][36][38][39] and bacteriocin-like substances, with a broader spectrum of activity than bacteriocins (e.g. a heat-resistant peptide produced by Lactobacillus salivarius subsp. salivarius CRL 1328).[6][40] Several studies have indicated that the activity of bacteriocins is favored by low pH.[4][41] In summary, the inhibitory substances produced by vaginal Lactobacillus species seem to be a primary factor in protecting the vaginal econiche, with organic acids, bacteriocins (and hydrogen peroxide) acting synergistically to prevent colonization by pathogenic anaerobes. Not all Lactobacillus spp. and not all strains within one Lactobacillus species exhibit all 3 mechanisms.[8] It is of importance to note that only a select group of Lactobacillus species has been found to dominate the vaginal econiche of premenopausal women, i.e. L. crispatus, L. jensenii, L. iners, L. gasseri (and possibly L. vaginalis), as assessed through cultivation-dependent and cultivation-independent techniques.[28][29][30][42][43][44][45][46][47][48] Vaginal lactobacilli have been shown to display a pronounced vaginotropism, and their pili act as ligands for attachment to glycolipid receptors of vaginal epithelial cells.[49][50] The limited number of Lactobacillus spp. found in the human vagina is remarkable, which leads to the possibility that there are host factors that select for specific organisms, that these species have unusual characteristics that allow them to successfully colonize the vagina, or both .[46] However, the vaginotropism, does not only apply to this selected group of lactobacilli that stand for a healthy vagina, but also for the bacterial species associated with BV.[51] The microflora detected in the human genital and gut econiche do not appear to grow outside their host and probably are likely to rely on the close contact between parents and their children for transmission,[51] e.g. mother to neonate transmission of genital microflora, most probably also with gut microflora homogenously distributed over the baby‘s body including skin, the oral cavity, nasopharynx, and feces.[52] Molecular studies have shown that the intestinal microflora of identical and fraternal twins show greater similarities than between twins and their partners, this is probably due to a shared mother.[50]
Other vaginal bacterial species
Several anaerobic bacterial species are frequently found in the vagina, such as the Gram positive cocci: Atopobium vaginae, Peptostreptococcus spp., Staphylococcus spp., Streptococcus spp., and Bacteroides spp., Fusobacterium spp., Gardnerella vaginalis, Mobiluncus, Prevotella spp., and Gram-negative enteric organisms, such as Escherichia coli.[28][29][44][53][54][55][56][57][58] Also Candida albicans, Mycoplasma and Ureaplasma are frequently found in the vagina.[49][53][57] Some of the obligate and facultative anaerobic bacteria are associated with BV.[56] In the pyrosequencing study by Ravel et al.,[44] comprising the vaginal microflora of 396 asymptomatic women, equally representing four ethnic groups (blacks, whites, Asian and Hispanics), five different communities of vaginal microflora were found, with four communities dominated by respectively Lactobacillus crispatus, L. gasseri, L. iners or L. jensenii and the fifth with higher proportions of strictly anaerobic bacteria, predominantly Megasphaera, Prevotella, Sneathia and Streptococcus spp. (designated the diverse group). Hummelen et al.[43] pyrosequenced (16S rRNA gene) the vaginal microflora of 132 HIV positive Tanzanian women and they detected eight major clusters. The two clusters that were strongly associated with normal vaginal microflora, were dominated by L. iners respectively L. crispatus. Four clusters were strongly associated with BV, and were dominated by G. vaginalis, Lachnospiraceae, P. bivia or a mixture of different species. The remaining 2 clusters were represented by the combination L. iners/G. vaginalis and the combination Lachnospiraceae/Veillonellaceae. In addition, G. vaginalis and L. iners were detected in each sample, so they were proposed as core members of the vaginal microflora.[43]
What is normal vaginal microflora?
Recent studies have provided more insight about the composition of vaginal microflora, and it is becoming clearer that a single core of normal vaginal microflora dominated by lactobacilli could be an oversimplification of the reality. More than 20 vaginal species of Lactobacillus have been detected, although only 4 to 5, namely L. crispatus, L. gasseri, L. iners, L. jensenii and possibly L. vaginalis dominate the vaginal econiche.[28][42][44][46][58][59][60][61] Several studies have demonstrated that a significant proportion (7–33%) of healthy, asymptomatic women (especially black and Hispanic women [44][59] lack appreciable numbers of Lactobacillus species in the vagina,[43][44][46][58][59][62] which may be replaced by other lactic acid-producing bacteria that contribute to vaginal acid production by fermentation, i.e. species from the genera Atopobium, Leptotrichia, Leuconostoc, Megasphaera, Pediococcus, Streptococcus and Weissella,[46][59][63][64] and also Escherichia coli isolates have been shown to acidify their growth media in vitro through the production of lactate.[65] C. albicans is also known to produce acid, to thrive in a low pH environment and to coexist with lactobacilli.[66][67] Interestingly, all ethnic populations have vaginal microflora communities containing lactic acid producing bacteria [44][46] .[64][68][69] This is indicative for the fact that, although the structure of the bacterial communities may differ between populations, health can be maintained provided the functions of these communities, for example the production of lactic acid, are maintained .[46][70] This may be in agreement with the findings of previous studies [59][62] and calls for a reassessment of the predominant opinion that normal vaginal microflora is always characterized by the presence of high numbers of lactobacilli. Forney et al.[71] postulated:” We suspect that the causes of and cures for BV will continue to be enigmatic until it is recognized that, although “normal and healthy” can be equated with high numbers of lactobacilli, the converse — “unhealthy” being equated with low numbers of or no lactobacilli — is not necessarily true”. This implies that not all communities may be equally resilient, so that if the resilience of a vaginal community is low then transitory changes in the structure of these communities may occur more readily in response to disturbances of various kinds, including menses, sexual intercourse, douching and contraceptive practices.[59] Zhou et al.[59] hypothesized: ―These differences in the structure and composition of microbial communities may underlie well-known differences in the susceptibility of women in these racial groups to BV and various vaginal infections‖.[59][72][73] Although it can be agreed that we should be cautious about which vaginal microflora should be considered as disturbed, and although (lactic) acid is indeed produced by many species in each of these communities, the remark by Mirmonsef et al.[74] that emphasis should be on vaginal pH and not on mere acid production in establishing normal vaginal microflora may be justified. The importance of maintaining low pH as a protective mechanism also follows from the fact that pH further decreases during pregnancy. Indeed, several studies suggest that BV without clinical symptoms is still a risk factor, not only for STD/HIV infection, but also for poor obstetric outcomes.[66][75] The acid production may be counteracted differently by different types of vaginal microflora, whereby vaginal microflora not dominated by lactoabilli may produce more amines and ammonia, due to proteolytic activity, which is indeed a hallmark of disturbed vaginal microflora.
Menstruation
During menstruation, the concentration of vaginal microbiome is observed to decline.[76] The effect of tampon use on vaginal flora is debated, but application of tampons appears not to significantly modify the balance of bacterial presence.
Disease prevention
A healthy vaginal microbiome aids in the prevention of bacterial vaginosis, yeast infections and other possible problems by maintaining an acidic pH (< 4.5) that is unfavourable for the growth of common pathogens, such as Gardnerella vaginalis. The lactobacilli present in a healthy vaginal microbiome also occupy the ecological niche that would otherwise be available for exploitation by pathogenic organisms. However, harmful bacteria or an imbalance in bacteria can lead to infection.
One method of reducing the risk of infection in the local area of the urethra is to urinate immediately after sex. Additionally, exclusive use of sterile contraceptives can assist in prevention of infection.
See also
- Bacterial vaginosis
- Human flora
- Human microbiome project
- Skin flora
References
- ↑ 1.0 1.1 Vasquez, A.; Jakobsson, T.; Ahrne, S.; Forsum, U.; Molin, G. (2002). "Vaginal Lactobacillus Flora of Healthy Swedish Women". Journal of Clinical Microbiology 40 (8): 2746–2749. doi:10.1128/JCM.40.8.2746-2749.2002. PMC 120688. PMID 12149323.
- ↑ Graver, M., and J. Wade. 2011. The role of acidification in the inhibition of Neisseria gonorrhoeae by vaginal lactobacilli during anaerobic growth. Ann. Clin. Microbiol. Antimicrob. 10:8.
- ↑ Matu, M. N., G. O. Orinda, E. N. M. Njagi, C. R. Cohen, and E. A. Bukusi. 2010. In vitro inhibitory activity of human vaginal lactobacilli against pathogenic bacteria associated with bacterial vaginosis in Kenyan women. Anaerobe 16:210-215.
- ↑ 4.0 4.1 4.2 Skarin, A., and J. Sylwan. 1986. Vaginal Lactobacilli inhibiting growth of Gardnerella vaginalis, Mobiluncus and other bacterial species cultured from vaginal content of women with bacterial vaginosis. APMIS. 94:399-403.
- ↑ Strus, M., M. Malinowska, and P. B. Heczko. 2002. In vitro antagonistic effect of Lactobacillus on organisms associated with bacterial vaginosis. J. Reprod. Med. 47:41-46.
- ↑ 6.0 6.1 Boris, S., and C. Barbes. 2000. Role played by lactobacilli in controlling the population of vaginal pathogens. Microb. Infect. 2:543-546.
- ↑ Al-Mushrif, S., and B. M. Jones. 1998. A study of the prevalence of hydrogen peroxide generating lactobacilli in bacterial vaginosis: The determination of H2O2 concentrations generated, in vitro , by isolated strains and the levels found in vaginal secretions of women with and without infection. J. Obstet. Gynaecol. 18:63-67.
- ↑ 8.0 8.1 8.2 8.3 Aroutcheva, A., D. Gariti, M. Simon, S. Shott, J. Faro, J. A. Simoes, A. Gurguis, and S. Faro. 2001. Defense factors of vaginal lactobacilli. Am. J. Obstet. Gynecol. 185:375-379.
- ↑ 9.0 9.1 9.2 Martin, R., and J. E. Suarez. 2010 Biosynthesis and degradation of H2O2 by vaginal lactobacilli. Appl. Environ. Microbiol. 76:400-405.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 O'Hanlon, D., T. Moench, and R. Cone. 2011. In vaginal fluid, bacteria associated with bacterial vaginosis can be suppressed with lactic acid but not hydrogen peroxide. BMC Infect. Dis.11:200.
- ↑ Tomas, M. S., M. Claudia Otero, V. Ocana, and M. Elena Nader-Macias. 2004. Production of antimicrobial substances by lactic acid bacteria I: Determination of hydrogen peroxide. Methods Mol. Biol. 268:337-346.
- ↑ 12.0 12.1 Vallor, A. C., M. A. Antonio, S. E. Hawes, and S. L. Hillier. 2001. Factors associated with acquisition of, or persistent colonization by, vaginal lactobacilli: Role of hydrogen peroxide production. J. Infect. Dis. 184:1431-1436.
- ↑ Linhares, I. M., P. R. Summers, B. Larsen, P. C. Giraldo, and S. S. Witkin. 2011. Contemporary perspectives on vaginal pH and lactobacilli. Am. J. Obstet. Gynecol. 204:120.e1-120.e5.
- ↑ Redondo-Lopez, V., R. L. Cook, and J. D. Sobel. 1990. Emerging role of lactobacilli in the control and maintenance of the vaginal bacterial microflora. Rev. Infect. Dis. 12:856-872.
- ↑ Dahiya, R. S., and M. L. Speck. 1968. Hydrogen peroxide formation by lactobacilli and its effect on Staphylococcus aureus. J. Dairy Sci. 51:1568-1572.
- ↑ Thompson, R., and A. Johnson. 1951. The inhibitory action of saliva on the diphtheria Bacillus: Hydrogen peroxide, the inhibitory agent produced by salivary streptococci. J. Infect. Dis. 88:81-85.
- ↑ Wheater, D. M., A. Hirsch, and A. T. R. Mattick. 1952. Possible identity of lactobacillin with hydrogen peroxide produced by lactobacilli. Nature 170:623-624.
- ↑ 18.0 18.1 18.2 18.3 Eschenbach, D. A., P. R. Davick, B. L. Williams, S. J. Klebanoff, K. Young-Smith, C. M. Critchlow, and K. K. Holmes. 1989. Prevalence of hydrogen peroxide-producing Lactobacillus species in normal women and women with bacterial vaginosis. J. Clin. Microbiol. 27:251-256.
- ↑ 19.0 19.1 Hillier, S. L., M. A. Krohn, S. J. Klebanoff, and D. A. Eschenbach. 1992. The relationship of hydrogen peroxide-producing lactobacilli to bacterial vaginosis and genital microflora in pregnant women. Obstet. Gynecol. 79:369-373.
- ↑ Klebanoff SJ, S. D. 1970. Peroxidase-mediated antimicrobial activity of rat uterine fluid. Gynecol Invest 1:21-30.
- ↑ 21.0 21.1 Klebanoff, S. J., S. L. Hillier, D. A. Eschenbach, and A. M. Waltersdorph. 1991. Control of the microbial flora of the vagina by H202-generating lactobacilli. J. Infect. Dis. 164:94-100.
- ↑ Klebanoff, S. J., and R. W. Coombs. 1991. Viricidal effect of Lactobacillus acidophilus on human immunodeficiency virus type 1: Possible role in heterosexual transmission. J. Exp. Med. 174:289-292.
- ↑ Atashili, J., C. Poole, P. M. Ndumbe, A. A. Adimora, and J. S. Smith. 2008. Bacterial vaginosis and HIV acquisition: A meta-analysis of published studies. AIDS 22:1493-1501.
- ↑ Baeten, J. M., W. M. Hassan, V. Chohan, B. A. Richardson, K. Mandaliya, J. O. Ndinya-Achola, W. Jaoko, and R. S. McClelland. 2009. Prospective study of correlates of vaginal Lactobacillus colonisation among high-risk HIV-1 seronegative women. Sex. Transm. Infect. 85:348-353.
- ↑ Cantoni, O, Brandi, G, Schiavano, F. G, Albano, A, and Cattabeni, F. 1989. Lethality of hydrogen peroxide in wild type and superoxide dismutase mutants of Escherichia coli. (A hypothesis on the mechanism of H2O2-induced inactivation of Escherichia coli), Vol. 70. Elsevier, Shannon, Ireland.
- ↑ Demba, E., L. Morison, M. van der Loeff, A. Awasana, E. Gooding, R. Bailey, P. Mayaud, and B. West. 2005. Bacterial vaginosis, vaginal flora patterns and vaginal hygiene practices in patients presenting with vaginal discharge syndrome in The Gambia, West Africa. BMC Infect. Dis.5:12.
- ↑ Wilks, M., R. Wiggins, A. Whiley, E. Hennessy, S. Warwick, H. Porter, A. Corfield, and M. Millar. 2004. Identification and H2O2 production of vaginal lactobacilli from pregnant women at high risk of preterm birth and relation with outcome. J. Clin. Microbiol. 42:713-717.
- ↑ 28.0 28.1 28.2 28.3 Verhelst, R., H. Verstraelen, G. Claeys, G. Verschraegen, L. Van Simaey, C. De Ganck, E. De Backer, M. Temmerman, and M. Vaneechoutte. 2005. Comparison between Gram stain and culture for the characterization of vaginal microflora: Definition of a distinct grade that resembles grade I microflora and revised categorization of grade I microflora. BMC Microbiol. 5:61.
- ↑ 29.0 29.1 29.2 De Backer, E., R. Verhelst, H. Verstraelen, M. A. Alqumber, J. P. Burton, J. R. Tagg, M. Temmerman, and M. Vaneechoutte. 2007. Quantitative determination by real-time PCR of four vaginal Lactobacillus species, Gardnerella vaginalis and Atopobium vaginae indicates an inverse relationship between L. gasseri and L. iners. BMC Microbiol. 7:115
- ↑ 30.0 30.1 Antonio, M. A., S. E. Hawes, and S. L. Hillier. 1999. The identification of vaginal Lactobacillus species and the demographic and microbiologic characteristics of women colonized by these species. J. Infect. Dis. 180:1950-1956.
- ↑ Antonio, M. A. D., L. K. Rabe, and S. L. Hillier. 2005. Colonization of the rectum by Lactobacillus species and decreased risk of bacterial vaginosis. J. Infect. Dis. 192:394-398.
- ↑ Hawes, S. E., S. L. Hillier, J. Benedetti, C. E. Stevens, L. A. Koutsky, P. l. Wolner-Hanssen, and K. K. Holmes. 1996. Hydrogen peroxide-producing lactobacilli and acquisition of vaginal infections. J. Infect. Dis. 174:1058-1063.
- ↑ 33.0 33.1 33.2 O'Hanlon, D. E., B. R. Lanier, T. R. Moench, and R. A. Cone. 2010. Cervicovaginal fluid and semen block the microbicidal activity of hydrogen peroxide produced by vaginal lactobacilli. BMC Infect. Dis.10:120.
- ↑ Alpay-Karaoglu, S., F. Aydin, S. S. Kilic, and A. O. Kilic. 2002. Antimicrobial activity and characteristics of bacteriocins produced by vaginal lactobacilli. Turk. J. Med. Sci. 33:7-12.
- ↑ Tahara, T., and K. Kanatani. 1997. Isolation and partial characterization of crispacin A, a cellassociated bacteriocin produced by Lactobacillus crispatus JCM 2009. FEMS Microbiol. Lett. 147:287-290.
- ↑ 36.0 36.1 Turovskiy, Y., R. D. Ludescher, A. A. Aroutcheva, S. Faro, and M. L. Chikindas. 2009. Lactocin 160, a bacteriocin produced by vaginal Lactobacillus rhamnosus, targets cytoplasmic membranes of the vaginal pathogen, Gardnerella vaginalis. Probiotics Antimicrob. Proteins 1:67-74.
- ↑ Klaenhammer, T. R. 1988. Bacteriocins of lactic acid bacteria. Biochimie 70:337-349.
- ↑ ten Brink, B., M. Minekus, J. M. van der Vossen, R. J. Leer, and J. H. Huis in't Veld. 1994. Antimicrobial activity of lactobacilli: Preliminary characterization and optimization of production of acidocin B, a novel bacteriocin produced by Lactobacillus acidophilus M46. J. Appl. Bacteriol.77:140-148.
- ↑ McGroarty, J. A., and G. Reid. 1988. Detection of a Lactobacillus substance that inhibits Escherichia coli. Can. J. Microbiol. 34:974-978.
- ↑ Ocana, V. S., A. A. Pesce de Ruiz Holgado, and M. E. Nader-Marcias. 1991. Characteristics of a bacteriocins-like substance produced by a vaginal Lactobacillus salivarius strain. Appl. Env. Microbiol. 65:5631-5635.
- ↑ Dembele, T., V. Obdrzalek, and M. Votava. 1998. Inhibition of bacterial pathogens by lactobacilli. Zentralbl. Bakteriol. 288:395-401.
- ↑ 42.0 42.1 Lopes dos Santos Santiago, G., P. Cools, H. Verstraelen, M. Trog, G. Missine, N. El Aila, R. Verhelst, I. Tency, G. Claeys, M. Temmerman, and M. Vaneechoutte. 2011. Longitudinal study of the dynamics of vaginal microflora during two consecutive menstrual cycles. PLOS ONE 6:e28180.
- ↑ 43.0 43.1 43.2 43.3 Hummelen, R., A. D. Fernandes, J. M. Macklaim, R. J. Dickson, J. Changalucha, G. B. Gloor, and G. Reid. 2010. Deep sequencing of the vaginal microbiota of women with HIV. PloS One 5:e12078.
- ↑ 44.0 44.1 44.2 44.3 44.4 44.5 44.6 Ravel, J., P. Gajer, Z. Abdo, G. M. Schneider, S. S. Koenig, S. L. McCulle, S. Karlebach, R. Gorle, J. Russell, C. O. Tacket, R. M. Brotman, C. C. Davis, K. Ault, L. Peralta, and L. J. Forney. 2011. Vaginal microbiome of reproductive-age women. Proc. Natl. Acad. Sci. U S A. 108:4680-4687.
- ↑ Giorgi, A., S. Torriani, F. Dellaglio, G. Bo, E. Stola, and L. Bernuzzi. 1987. Identification of vaginal lactobacilli from asymptomatic women. Microbiologica 10:377-384.
- ↑ 46.0 46.1 46.2 46.3 46.4 46.5 46.6 Zhou, X., S. J. Bent, M. G. Schneider, C. C. Davis, M. R. Islam, and L. J. Forney. 2004. Characterization of vaginal microbial communities in adult healthy women using cultivationindependent methods. Microbiol. 150:2565-2573.
- ↑ Zhou, X., M. A. Hansmann, C. C. Davis, H. Suzuki, C. J. Brown, U. Schütte, J. D. Pierson, and L. J. Forney. 2010. The vaginal bacterial communities of Japanese women resemble those of women in other racial groups. FEMS Immunol. Med. Microbiol. 58:169-181.
- ↑ Zozaya-Hinchliffe, M., R. Lillis, D. H. Martin, and M. J. Ferris. 2010. Quantitative PCR assessments of bacterial species in women with and without bacterial vaginosis. J. Clin. Microbiol. 48:1812-1819.
- ↑ 49.0 49.1 Hillier, S. L. 2008. Normal genital flora, p. 289–307, Sex. Transm. Dis. McGraw-Hill Companies, New York.
- ↑ 50.0 50.1 Ley, R. E., D. A. Peterson, and J. I. Gordon. 2006. Ecological and evolutionary forces shaping microbial diversity in the human intestine. Cell 124:837-848.
- ↑ 51.0 51.1 Danielsson, D., P. K. Teigen, and H. Moi. 2011. The genital econiche: Focus on microbiota and bacterial vaginosis. Ann. N. Y. Acad. Sci. 1230:48-58.
- ↑ Dominguez-Bello, M. G., E. K. Costello, M. Contreras, M. Magris, G. Hidalgo, N. Fierer, and R. Knight. 2010. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc. Natl. Acad. Sci. U S A. 107:11971-11975.
- ↑ 53.0 53.1 Bartlett, J. G., A. B. Onderdonk, E. Drude, C. Goldstein, M. Anderka, S. Alpert, and W. M. McCormack. 1977. Quantitative bacteriology of the vaginal flora. J. Infect. Dis. 136:271-277.
- ↑ Johnson, S. R., C. R. Petzold, and R. P. Galask. 1985. Qualitative and quantitative changes of the vaginal microbial flora during the menstrual cycle. Am. J. Reprod. Immunol. Microbiol. 9:1-5.
- ↑ Kalra, A., C. Palcu, J. Sobel, and R. Akins. 2007. Bacterial vaginosis: Culture- and PCR-based characterizations of a complex polymicrobial disease’s pathobiology. Curr. Infect. Dis. Rep. 9:485-500.
- ↑ 56.0 56.1 Larsen, B., and G. R. Monif. 2001. Understanding the bacterial flora of the female genital tract. Clin. Infect. Dis. 32:e69-77.
- ↑ 57.0 57.1 Sautter, R. L., and W. J. Brown. 1980. Sequential vaginal cultures from normal young women. J. Clin. Microbiol. 11:479-484.
- ↑ 58.0 58.1 58.2 Verhelst, R., H. Verstraelen, G. Claeys, G. Verschraegen, J. Delanghe, L. Van Simaey, C. De Ganck, M. Temmerman, and M. Vaneechoutte. 2004. Cloning of 16S rRNA genes amplified from normal and disturbed vaginal microflora suggests a strong association between Atopobium vaginae, Gardnerella vaginalis and bacterial vaginosis. BMC Microbiol. 4:16.
- ↑ 59.0 59.1 59.2 59.3 59.4 59.5 59.6 59.7 Zhou, X., C. J. Brown, Z. Abdo, C. C. Davis, M. A. Hansmann, P. Joyce, J. A. Foster, and L. J. Forney. 2007. Differences in the composition of vaginal microbial communities found in healthy Caucasian and black women. ISME J. 1:121-133.
- ↑ Pavlova, S. I., A. O. Kilic, S. S. Kilic, J. S. So, M. E. Nader-Macias, J. A. Simoes, and L. Tao. 2002. Genetic diversity of vaginal lactobacilli from women in different countries based on 16S rRNA gene sequences. J. Appl. Microbiol. 92:451-459.
- ↑ Burton, J. P., and G. Reid. 2002. Evaluation of the bacterial vaginal flora of 20 postmenopausal women by direct (Nugent score) and molecular (polymerase chain reaction and denaturing gradient gel electrophoresis) techniques. J. Infect. Dis. 186:1770-1780.
- ↑ 62.0 62.1 Hyman, R. W., M. Fukushima, L. Diamond, J. Kumm, L. C. Giudice, and R. W. Davis. 2005. Microbes on the human vaginal epithelium. Proc. Natl. Acad. Sci. U S A. 102:7952-7957.
- ↑ Fredricks, D. N., T. L. Fiedler, and J. M. Marrazzo. 2005. Molecular identification of bacteria associated with bacterial vaginosis. N. Engl. J. Med. 353:1899-1911.
- ↑ 64.0 64.1 Jin, L., L. Tao, S. I. Pavlova, J. S. So, N. Kiwanuka, Z. Namukwaya, B. A. Saberbein, and M. Wawer. 2007. Species diversity and relative abundance of vaginal lactic acid bacteria from women in Uganda and Korea. J. Appl. Microbiol. 102:1107-1115.
- ↑ McCabe, K., M. D. Mann, and M. D. Bowie. 1998. D-lactate production and [14C]succinic acid uptake by adherent and nonadherent Escherichia coli. Infect. Immun. 66:907-911.
- ↑ 66.0 66.1 Martin, H. L., B. A. Richardson, P. M. Nyange, L. Lavreys, S. L. Hillier, B. Chohan, K. Mandaliya, J. O. Ndinya-Achola, J. Bwayo, and J. Kreiss. 1999. Vaginal lactobacilli, microbial flora, and risk of human immunodeficiency virus type 1 and sexually transmitted disease acquisition. J. Infect. Dis. 180:1863-1868.
- ↑ Klinke, T., S. Kneist, J. J. de Soet, E. Kuhlisch, S. Mauersberger, A. Forster, and W. Klimm. 2009. Acid production by oral strains of Candida albicans and lactobacilli. Caries Res. 43:83- 91.
- ↑ Nam, H., K. Whang, and Y. Lee. 2007. Analysis of vaginal lactic acid producing bacteria in healthy women. J. Microbiol. 45:515-520.
- ↑ Rodriguez Jovita, M., M. D. Collins, B. Sjoden, and E. Falsen. 1999. Characterization of a novel Atopobium isolate from the human vagina: Description of Atopobium vaginae sp. nov. Int. J. Syst. Bacteriol. 49:1573-1576.
- ↑ Yamamoto, T., X. Zhou, C. J. Williams, A. Hochwalt, and L. J. Forney. 2009. Bacterial populations in the vaginas of healthy adolescent women. J. Pediatr. Adolesc. Gynecol.22:11- 18.
- ↑ Forney, L. J., J. A. Foster, and W. Ledger. 2006. The vaginal flora of healthy women is not always dominated by Lactobacillus species. J. Infect. Dis. 194:1468-1469.
- ↑ Martin, J. A., B. E. Hamilton, P. D. Sutton, S. J. Ventura, T. J. Mathews, S. Kirmeyer, and M. J. Osterman. 2010. Births: Final data for 2007. National vital statistics reports 58:1-85.
- ↑ Ness, R. B., S. Hillier, H. E. Richter, D. E. Soper, C. Stamm, D. C. Bass, R. L. Sweet, and P. Rice. 2003. Can known risk factors explain racial differences in the occurrence of bacterial vaginosis? J. Natl. Med. Assoc. 95:201-212.
- ↑ Mirmonsef, P., D. Gilbert, R. S. Veazey, J. Wang, S. R. Kendrick, and G. T. Spear. 2012. A comparison of lower genital tract glycogen and lactic acid levels in women and macaques: Implications for HIV and SIV susceptibility. AIDS Res. Hum. Retroviruses 28:76-81.
- ↑ Hillier, S. L., R. P. Nugent, D. A. Eschenbach, M. A. Krohn, R. S. Gibbs, D. H. Martin, M. F. Cotch, R. Edelman, J. G. Pastorek, A. V. Rao, D. McNellis, J. A. Regan, J. C. Carey, and M. A. Klebanoff. 1995. Association between bacterial vaginosis and preterm delivery of a lowbirth- weight infant. N. Engl. J. Med. 333:1737-1742.
- ↑ Onderdonk, A. B.; Zamarchi, G. R.; Walsh, J. A.; Mellor, R. D.; Muñoz, A.; Kass, E. H. (1986). "Methods for quantitative and qualitative evaluation of vaginal microflora during menstruation". Applied and environmental microbiology 51 (2): 333–339. PMC 238869. PMID 3954346.