Tolbutamide
 | |
|---|---|
| Systematic (IUPAC) name | |
| N-[(butylamino)carbonyl]-4-methylbenzenesulfonamide | |
| Clinical data | |
| AHFS/Drugs.com | monograph |
| MedlinePlus | a682481 |
| Licence data | US FDA:link |
| Pregnancy cat. | C (AU) C (US) |
| Legal status | POM (UK) ℞-only (US) |
| Routes | Oral (tablet) |
| Pharmacokinetic data | |
| Protein binding | 96% |
| Metabolism | Hepatic (CYP2C19-mediated) |
| Half-life | 4.5 to 6.5 hours |
| Excretion | Renal |
| Identifiers | |
| CAS number | 64-77-7 |
| ATC code | A10BB03 V04CA01 |
| PubChem | CID 5505 |
| IUPHAR ligand | 2415 |
| DrugBank | DB01124 |
| ChemSpider | 5304 |
| UNII | 982XCM1FOI |
| KEGG | D00380 |
| ChEBI | CHEBI:27999 |
| ChEMBL | CHEMBL782 |
| Chemical data | |
| Formula | C12H18N2O3S |
| Mol. mass | 270.35 g/mol |
| SMILES
| |
| |
| | |
Tolbutamide is a first generation potassium channel blocker, sulfonylurea oral hypoglycemic drug sold under the brand name Orinase. This drug may be used in the management of type II diabetes if diet alone is not effective. Tolbutamide stimulates the secretion of insulin by the pancreas. Since the pancreas must synthesize insulin in order for this drug to work, it is not effective in the management of type I diabetes. It is not routinely used due to a higher incidence of adverse effects compared to newer second generation sulfonylureas, such as glyburide. It generally has a short duration of action due to its rapid metabolism, and is therefore safe for use in elderly diabetics.
History
Orinase was developed by Upjohn Co. at a time when the primary medical treatment for diabetes was insulin injections. Eli Lilly had a lock on the market for insulin production at the time. Orinase, like other treatments for drugs detected by so-called paraclinical signs rather than clinically observable signs or patient-reported symptoms, benefitted from an increased sensitivity and availability of blood glucose testing. According to Jeremy A. Greene, Milton Moskowitz (editor in 1961 of Drug and Cosmetic Industry) claimed that the introduction of Orinase "expanded the total market by bringing under medical care diabetics who were formerly not treated." It did this by changing the mindset about diabetes even more than insulin had. Treatment of this chronic disease was no longer seen as a mere slowing of "inexorable degeneration" but instead viewed through "a model of surveillance and early detection"(Greene 84).
Orinase and other sulfonulureas emerged from European pharmaceutical research into antibiotics, specifically from attempts to develop sulfas. One of the contenders for a new sulfa antibiotic had serious side effects during clinical trials at Montpelier University including blackouts, convulsions, and coma, side effects not observed with any other drugs in the sulfa cohort. An insulin researcher at the same university heard of these side effects and recognized them as common results of hypoglycemia. The resulting class of drugs for lowering blood sugar came to be known as the sulfonylureas, epitomized by Orinase and still in use today in other forms.
Unfortunately for diabetics dependent on insulin as a treatment for their condition, this research at Montpelier occurred in the early 1940s and was significantly disrupted by German occupation of France during World War II. Development of these compounds was taken over by German pharmaceutical companies which were obviously disinclined to share their bounty with nations upon which they were waging war. The German research was, in turn, disrupted by Germany's defeat in 1945 and the partition of Germany into East and West. The sulfonylureas were trapped in East Germany. In 1952, someone smuggled a sample to a West German pharmaceutical company and research resumed. Clinical trials in diabetics began in 1954 in Berlin. In 1956 two different sulfonylureas were brought to market in Germany under the trade names Nadisan and Rastinon. As an important backdrop to this prime example of how society can affect science, American pharmaceutical companies in the post-war period had been seeking to establish business relations with the remnants of German pharmaceutical giants weakened by the war and partition of Germany. Upjohn (based in Kalamazoo up until its purchase by Pharmacia in the 1990s) made deals with the German company Hoechst, maker of Rastinon. The result was a cross-licensing agreement which produced Orinase.
Now begins a portion of the tale which involves intense industrial competition. Recall that Eli Lilly had locked down the market for diabetes therapy with insulin. Upjohn stood to open up a whole new arena of treatment for this chronic condition, one with a built-in and sustainable market, i.e. patient population. Just as two German companies brought sulfonylureas to market within the same year, Upjohn discovered that Eli Lilly had begun clinical trials for another German oral hypoglycemic, carbutamide, and was considering a similar licensing deal with the German pharmaceutical company Boehringer which made Nadisan (carbutamide). Upjohn pushed for large-scale clinical trials from 1955-1957, enrolling over 5,000 patients at multiple sites.
Upjohn's formulation became ascendant when the Lilly formulation demonstrated mounting evidence of toxicity in parallel trials at the Joslin Clinic. Lilly pulled carbutamide and halted development, leaving the field open for Upjohn to market a new treatment for diabetics to a patient population previously monopolized by Eli Lilly. In 1956, Upjohn filed for approval from the Food and Drug Administration. A notable fact about the application is its size: 10,580 pages in 23 volumes with 5,786 cases reports. Jeremy A. Greene analyzes that this was necessary to "render visible the relatively small improvements provided in less severe forms of diabetes." (92) Indeed, Orinase was marketed by Upjohn not as a cure-all for all diabetics, but specifically as a treatment that was "not an oral insulin" and "did not work in all diabetics." Those were the instructions for marketing given to Upjohn's salespeople. This is just as well, for as indicated by the FDA application, Orinase had been demonstrated "not to be effective in severe Diabetes, but only in milder cases of the disease." (Greene 93) Greene's analysis reveals an important fact about Orinase: that it was one of a new class of drugs (including treatments for hypertension and hypercholesterolemia) aimed at providing marginal benefits over existing treatments for patients who had not previously been a target market for pharmaceuticals.
According to Greene, there was a close connection between the launch of Orinase and increased funding by Upjohn for public health efforts to find previously undiagnosed and asymptomatic diabetics. The only way to detect such diabetics was through population-wide screening using urine or blood sugar tests. Such so-called "hidden diabetics", once found, were "unlikely to submit themselves to a lifetime of insulin injections" to prevent themselves from developing symptoms of a condition that currently did not seem to be affecting them at all. Indeed, "Orinase altered this logic. To newly detected, symptomless diabetics, Orinase offered a solution that many found preferable to diet or insulin." (Greene 99) The appeal? It was a pill that required no lifestyle changes and involved no risk of infection or pain such as that incurred by insulin injections. The increase in funding for, and interest in, aggressive detection of hidden diabetics served to identify patients who would be more likely to take Orinase than either of the other two options.
As blood sugar testing for diagnosis of diabetes became more widespread, a curious side effect occurred: because blood sugar testing is not absolutely definitive in diagnoses of diabetes, more and more people were receiving borderline tests regarding their glycemic status. These borderline persons could be conceived of not as having diabetes, but as being at risk for diabetes. We now label such persons as "prediabetic." Prediabetics have high blood sugar, but normal levels of sugar in their urine (glycosuria), whereas high blood sugar combined with glycosuria were considered definitive of diabetes. Upjohn saw an opportunity to potentially benefit and definitely market to a yet-greater expansion of the diabetic population, beyond even the "hidden diabetics" revealed by earlier public health campaigns. What's more, Upjohn found a new use for Orinase: as a diagnostic. Orinase Diagnostic was added to the Orinase product line and, by 1962, was being touted by Upjohn salesmen as means of detecting prediabetes in that an abnormal response to Orinase following administration of cortisone in a "stress test" could be taken to indicate prediabetes. Orinase thus not only served to detect a previously hidden patient population, but also detected a patient population most likely to be interested in Orinase as a treatment for their newly diagnosed prediabetes. By the late 1960s, Orinase Diagnostic was withdrawn and the drug reverted to its therapeutic purpose. By that point, prediabetes had become a diagnosable and treatable condition which had dramatically increased the market for Orinase. The benefits for Upjohn are clear. The benefits for those diagnosed with the condition stemmed from the medical consensus that prediabetes might be reversible whereas diabetes was clearly an irreversible chronic disease, albeit one that could now be treated fairly well.
Orinase began to fall out of favor in May 1970 when asymptomatic prediabetics on long-term regimens of Orinase began to see news reports (beginning with the Washington Post) that Orinase may have serious side effects including death from cardiovascular problems, according to a long-term study. Patients learned of this before their physicians, in many cases, and before the FDA could advise relabeling the medication or suggesting alterations in appropriate usage, a public firestorm began over the use of medications to treat risk conditions that are themselves asymptomatic. The question of whether Orinase did or did not increase cardiovascular problems in those taking it has not been conclusively settled. The result: Orinase and other medical treatments for prediabetes were "rolled back" by the FDA and practitioners in an attempt to focus on symptomatic patients for whom the risks of treatment, whatever they were, might be balanced by the symptoms of the disease. But according to Jeremy A. Greene, "there was no simple path back" from the diagnostic and therapeutic shift to asymptomatic risk conditions.
Pharmacia - Upjohn (now, itself, a casualty of mergers with other companies) stopped making Orinase in 2000, though a generic is still available and occasionally used.
Historical consequences
The heritage of Orinase (tolbutamide) has had a lasting effect on medicine and the pharmaceutical industry. Patients today are still diagnosed with prediabetes, many of them managing to stave off the onset of diabetes through dietary and lifestyle changes. But many also have the option to take Bristol-Myers Squibb's oral antidibetic medication Glucophage (metformin), which demonstrated a 31 percent reduction in three-year incidence of development of diabetes relative to placebo. While impressive, the lifestyle-modification arm of that same trial demonstrated a 58% reduction. (Diabetes Prevention Program Research Group)
Orinase was one of a number of drugs developed during the 1950s and 1960s for a variety of conditions first to treat symptomatic diseases and later to treat asymptomatic conditions that put the patient at risk of developing symptomatic disease. Its use and marketing played a definitive, though not solely sufficient, role in establishing the condition of prediabetes as a legitimate diagnosable condition. As such, it illustrates that science, medicine, markets, and health can interact in complicated and fascinating ways that are neither clearly desirable nor undesirable.
Side Effects
- Hypoglycemia
- Weight gain
- Hypersensitivity- Cross-allergicity with sulfonamide
- Drug Interactions (especially first generation drugs): Increased hypoglycemia with cimetidine, insulin, salicylates, sulfonamides
Salicylates displace tolbutamide from its binding site on plasma binding proteins which lead to increase in free tolbutamide concentration and thus hypoglycemic shock.
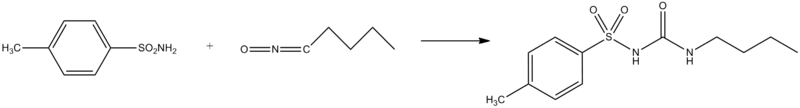
Synthesis
A number of different routes are available for the preparation of tolbutamide. The shortest route involves the simple addition of para-toluenesulfonamide to butyl isocyanate:[1]
Notes
- ↑ Ruschig, H.; Avmuller, W.; Korger, G.; Wagner, H.; Scholtz, J.; Bander, A.; 1961, U.S. Patent 2,976,317.
References
- Diabetes Prevention Program Research Group. "Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin." Journal of the American Medical Association 346: 393-402. 2000.
- Jeremy A. Greene. Prescribing by Numbers: Drugs and the Definition of Disease. Johns Hopkins University Press: Baltimore, MD. 2007.
- William L. Lawrence. "Science in Review: Drug for the Treatment of Diabetes Tested And Found of Great Importance." New York Times February 24, 1957.
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||