Tinzaparin sodium
 | |
|---|---|
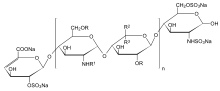
| n = 1 to 25, R = H or SO3Na, R1 = H, SO3Na or COCH3, R2 = H and R3 = COONa or R2 = COONa and R3 = H | |
| Clinical data | |
| AHFS/Drugs.com | monograph |
| Legal status | ? |
| Routes | subcutaneous (once daily) |
| Pharmacokinetic data | |
| Bioavailability | 90% for Anti-Xa activity, 67% for Anti-IIa activity)[1] |
| Metabolism | primarily by liver by desulfation and/or depolymerization |
| Half-life | 200 min. for Anti-Xa activity, 257. min for Anti-IIa activity [2] |
| Identifiers | |
| CAS number | 9005-49-6 [9041-08-1] (sodium salt) |
| ATC code | B01AB10 |
| UNII | 3S182ET3UA |
| KEGG | D07510 |
| ChEMBL | CHEMBL1201414 |
| Chemical data | |
| Formula | ? |
| Mol. mass | 6500 (average)[3] |
| | |
Tinzaparin is an antithrombotic drug in the heparin group. It is a low molecular weight heparin (LMWH) marketed as Innohep worldwide. It has been approved by the U.S. Food and Drug Administration (FDA) for once daily treatment and prophylaxis of deep vein thrombosis and pulmonary embolism.[4] Tinzaparin sodium is the only low molecular weight heparin shown to be safe in pregnancy and in critically ill people with renal failure at both treatment and prophylaxis dose levels.[5]
It can be given subcutaneously by syringe, or intravenously.[6] It was manufactured by Leo pharmaceutical company, who withdrew the product from the US in 2011 due to low sales and a contamination issue.[7]
F.D.A approved indications
In the United States, tinzaparin is FDA approved for the following indications:
- 1-Prophylaxis of DVT in medically ill and elderly patient.
- 2-Total hip & knee replacement,
- 3-Extended hip-replacement,
- 4-Abdominal surgery.
- 5-Treatment of DVT with or without PE.
- 6-prophylaxis and treatment of DVT in pregnant women.
- 7-as an assistant in the process of In Vitro Fertilization (IVF).
Indications approved in the UK and Australia
Tinzaparin is approved for the following
- 1-The prophylaxis of thromboembolism disorders of venous origin, in particular those that may be associated with orthopaedic surgery.
- 2-The prophylaxis of venous thromboembolism (VTE) in medical patients bedridden due to acute illness.
- 3-prophylaxis and treatment of DVT in pregnant women.
- 4-The treatment of venous thromboembolism disease (VTED) presenting with deep vein thrombosis (DVT), pulmonary embolism (PE) or both.
- 5-The treatment of unstable angina (UA) and non-Q-wave myocardial infarction (NQMI), administered concurrently with aspirin.
- 6-The prevention of thrombus formation in the extracorporeal circulation during haemodialysis.
- 7-The prevention of thrombus formation during episodes of lone Atrial Fibrillation, administered concurrently with aspirin (in the absence of long term anticoagulation treatment with warfarin.
Use in elderly
In July 2008, the company revised the prescribing information to restrict the use of tinzaparin in patients 90 years of age or older. FDA is concerned that the preliminary data from the IRIS study suggests that the increased risk of mortality is not limited only to patients 90 years of age or older.
According to the study Innohep increases the risk of death for elderly patients (i.e., 70 years of age and older) with renal insufficiency. Healthcare professionals should consider the use of alternative treatments to Innohep when treating elderly patients over 70 years of age with renal insufficiency and DVT, PE, or both.
(note the previous version of this article made a crucial error by removing the not from the sentence ...the increased risk of mortality is not limited only to patients 90 years of age... This revision corrects this and gives more detail of the advice..
Also see the Health Canada website. http://www.hc-sc.gc.ca/dhp-mps/medeff/advisories-avis/prof/_2010/innohep_hpc-cps-eng.php
Use in pregnancy
No LMWH, except tinzaparin, is licensed for use in gestational hypercoagulability.[8] Still, tinzaparin is often the LMWH of choice in pregnant women.[8]
Side effects
Bleeding in overdose. There is occasionally bruising at the site of injection.
Monitoring
Tinzaparin does NOT affect the international normalized ratio (INR), prothrombin time (PT)[citation needed] Anti-factor Xa levels can be measured, and are often used to monitor tinzaparin
Reversal agent
Protamine sulfate will reverse Tinzaparin by 85% per package insert.
References
- ↑ Cheer S.M. et al. Drugs 2004; 64 (13): 1479–1502
- ↑ Pedersen P.C. et al. Thromb Res 1991; 61 (5-6): 477-487
- ↑ European Pharmacopoeia, 6th Edition, 2008
- ↑ Hull et al. NEJM 1992;326,15:975-982
- ↑ Nagge J, Crowther M, Hirsch J (2002). "Is Impaired Renal Function a Contraindication to the Use of Low-Molecular-Weight Heparin?". Arch Intern Med. 162: 2605–2609. doi:10.1001/archinte.162.22.2605. PMID 12456233.
- ↑ Farmaceutiska Specialiteter i Sverige - the Swedish official drug catalog. Fass.se > Innohep
- ↑ http://www.ashp.org/DrugShortages/NotAvailable/Bulletin.aspx?id=749
- ↑ 8.0 8.1 Therapeutic anticoagulation in pregnancy. Norfolk and Norwich University Hospital (NHS Trust). Reference number CA3017. 9th June 2006 [review June 2009]
- 8- (22)ESHRE April-2011 volume 33 pages 12–13-14
- 9- e-medicine 2011
- 10- RCOG March-2010 (Royal college for Obestetric and Gynecology)
- 11- DVT.org/cardiologist
- 12- ^ Hull, New England Journal of Medicine, 2010 volume 22 page 19
External links
- tinzaparin at the US National Library of Medicine Medical Subject Headings (MeSH)
- Sprigg N, Gray LJ, Bath PM, et al. (2007). "Early recovery and functional outcome are related with causal stroke subtype: data from the tinzaparin in acute ischemic stroke trial". Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association 16 (4): 180–4. doi:10.1016/j.jstrokecerebrovasdis.2007.02.003. PMID 17689415.
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||