Thiazolidinedione
The thiazolidinediones /θaɪ.əˌzoʊlɨdiːnˈdaɪ.oʊn/, also known as glitazones, are a class of medications used in the treatment of diabetes mellitus type 2. They were introduced in the late 1990s.
Mechanism of action
Thiazolidinediones or TZDs act by activating PPARs (peroxisome proliferator-activated receptors), a group of nuclear receptors, with greatest specificity for PPARγ (gamma). The endogenous ligands for these receptors are free fatty acids (FFAs) and eicosanoids. When activated, the receptor binds to DNA in complex with the retinoid X receptor (RXR), another nuclear receptor, increasing transcription of a number of specific genes and decreasing transcription of others.
PPARγ transactivation

The activated PPAR/RXR heterodimer binds to peroxisome proliferator hormone response elements upstream of target genes in complex with a number of coactivators such as nuclear receptor coactivator 1 and CREB binding protein, this causes upregulation of genes (for a full list see PPARγ):
- Insulin resistance is decreased
- Adipocyte differentiation is modified[1]
- VEGF-induced angiogenesis is inhibited[2]
- Leptin levels decrease (leading to an increased appetite)
- Levels of certain interleukins (e.g. IL-6) fall
- Antiproliferative action[citation needed]
- Adiponectin levels rise
TZDs also increase the synthesis of certain proteins involved in fat and glucose metabolism, which reduces levels of certain types of lipids, and circulating free fatty acids. TZDs generally decrease triglycerides and increase high-density lipoprotein cholesterol (HDL-C) and low-density lipoprotein cholesterol (LDL-C). Although the increase in LDL-C may be more focused on the larger LDL particles, which may be less atherogenic, the clinical significance of this is currently unknown. Nonetheless, rosiglitazone, a certain glitazone, was suspended from allowed use by medical authorities in Europe, as it has been linked to an increased risk of heart attack and stroke.[3]
PPARγ transrepression

Binding of PPARγ to coactivators appears to reduce the levels of coactivators available for binding to pro-inflammatory transcription factors such as NF-κB, this causes a decrease in transcription of a number of pro inflammatory genes, including various interleukins and tumour necrosis factors.
Members of the class
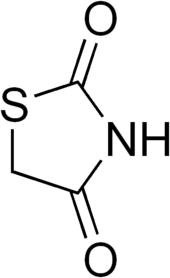
Chemically, the members of this class are derivatives of the parent compound thiazolidinedione, and include:
- Rosiglitazone (Avandia), which was put under selling restrictions in the US and withdrawn from the market in Europe due to some studies suggesting an increased risk of cardiovascular events. Upon re-evaluation of new data in 2013, the FDA lifted the restrictions.
- Pioglitazone (Actos), France and Germany have suspended the sale of the diabetes drug Actos after a study suggested the drug, also known as pioglitazone, could raise the risk of bladder cancer.[4]
- Troglitazone (Rezulin), which was withdrawn from the market due to an increased incidence of drug-induced hepatitis.
Experimental agents include netoglitazone, an antidiabetic agent, rivoglitazone, and the early non-marketed thiazolidinedione ciglitazone.
Replacing one oxygen atom in a thiazolidinedione with an atom of sulfur gives a rhodanine.
Uses
The only approved use of the thiazolidinediones is in diabetes mellitus type 2.
It is being investigated experimentally in polycystic ovary syndrome (PCOS), non-alcoholic steatohepatitis (NASH),[5] psoriasis,[6] autism,[7] ovarian hyperstimulation syndrome (by VEGF inhibition in granulosa cells),[8] lichen planopilaris, and other conditions.[9]
Several forms of lipodystrophy cause insulin resistance, which has responded favorably to thiazolidinediones. There are some indications that thiazolidinediones provide some degree of protection against the initial stages of breast carcinoma development.
Side effects and contraindications
The withdrawal of troglitazone has led to concerns of the other thiazolidinediones also increasing the incidence of hepatitis and potential liver failure, an approximately 1 in 20,000 individual occurrence with troglitazone. Because of this, the FDA recommends two to three month checks of liver enzymes for the first year of thiazolidinedione therapy to check for this rare but potentially catastrophic complication. To date, 2008, the newer thiazolidinediones, rosiglitazone and pioglitazone have been free of this problem.
The main side effect of all thiazolidinediones is water retention, leading to edema, generally a problem in less than 5% of individuals, but a big problem for some and potentially, with significant water retention, leading to a decompensation of potentially previously unrecognized heart failure. Therefore, thiazolidinediones should be prescribed with both caution and patient warnings about the potential for water retention/weight gain, especially in patients with decreased ventricular function (NYHA grade III or IV heart failure).
Though older studies suggested there may be an increased risk of coronary heart disease and heart attacks with rosiglitazone,[10] pioglitazone treatment, in contrast, has shown significant protection from both micro- and macro-vascular cardiovascular events and plaque progression.[11][12][13] These studies led to a period of Food and Drug Administration advisories (2007 - 2013) that, aided by extensive media coverage, led to a substantial decrease in rosiglitazone use. In November 2013, the FDA announced it would remove the usage restrictions for rosiglitazone in patients with coronary artery disease. [14] The new recommendations were largely based on the reasoning that prior meta-analyses leading to the original restrictions were not designed to assess cardiac outcomes and, thus, not uniformly collected or adjudicated. In contrast, one of the largest trials (RECORD trial) that was specifically designed to assess cardiac outcomes found no increased risk of myocardial infarction with rosiglitazone use, even after independent re-evaluation for FDA review.[15]
Preliminary data from a 10-year epidemiological study from Takeda Pharmaceutical Company indicated a possible link between pioglitazone (Actos) and bladder cancer. The findings prompted the FDA to order safety reviews for the drug in September 2010.[16]
Footnotes
- ↑ Waki H, Yamauchi T, Kadowaki T (February 2010). "[Regulation of differentiation and hypertrophy of adipocytes and adipokine network by PPARgamma]". Nippon Rinsho (in Japanese) 68 (2): 210–6. PMID 20158086.
- ↑ Panigrahy D, Singer S, Shen LQ, et al. (2002). "PPARγ ligands inhibit primary tumor growth and metastasis by inhibiting angiogenesis". J. Clin. Invest. 110 (7): 923–32. doi:10.1172/JCI15634. PMC 151148. PMID 12370270.
- ↑ NHS: Avandia diabetes drug suspended, Friday 24 September 2010
- ↑ http://www.huliq.com/3257/diabetes-drug-actos-sales-suspended-france-and-germany
- ↑ Belfort R, Harrison SA, Brown K, et al. (November 2006). "A placebo-controlled trial of pioglitazone in subjects with nonalcoholic steatohepatitis". N. Engl. J. Med. 355 (22): 2297–307. doi:10.1056/NEJMoa060326. PMID 17135584. Clinical trial info
- ↑ Krentz AJ, Friedmann PS (March 2006). "Type 2 diabetes, psoriasis and thiazolidinediones". Int. J. Clin. Pract. 60 (3): 362–3. doi:10.1111/j.1368-5031.2005.00765.x. PMID 16494655.
- ↑ Boris et al. Effect of pioglitazone treatment on behavioral symptoms in autistic children, Journal of Neuroinflammation 2007,4:3
- ↑ Shah DK, Menon KM, Cabrera LM, Vahratian A, Kavoussi SK, Lebovic DI (April 2010). "Thiazolidinediones decrease vascular endothelial growth factor (VEGF) production by human luteinized granulosa cells in vitro". Fertil. Steril. 93 (6): 2042–7. doi:10.1016/j.fertnstert.2009.02.059. PMC 2847675. PMID 19342033.
- ↑ Clinical Trials for Rosiglitazone - from ClinicalTrials.gov, a service of the U.S. National Institutes of Health
- ↑ "Avandia to Carry Stronger Heart Failure Warning - Forbes.com". Archived from the original on 2007-10-21. Retrieved 2007-08-15.
- ↑ Charbonnel B, Dormandy J, Erdmann E, Massi-Benedetti M, Skene A (July 2004). "The prospective pioglitazone clinical trial in macrovascular events (PROactive): can pioglitazone reduce cardiovascular events in diabetes? Study design and baseline characteristics of 5238 patients". Diabetes Care 27 (7): 1647–53. doi:10.2337/diacare.27.7.1647. PMID 15220241.
- ↑ Mannucci E, Monami M, Lamanna C, Gensini GF, Marchionni N (May 2008). "Pioglitazone and cardiovascular risk. A comprehensive meta-analysis of randomized clinical trials". Diabetes Obes Metab 0 (12): 1221–38. doi:10.1111/j.1463-1326.2008.00892.x. PMID 18505403.
- ↑ Nissen SE, Nicholls SJ, Wolski K, et al. (April 2008). "Comparison of pioglitazone vs glimepiride on progression of coronary atherosclerosis in patients with type 2 diabetes: the PERISCOPE randomized controlled trial". JAMA 299 (13): 1561–73. doi:10.1001/jama.299.13.1561. PMID 18378631.
- ↑ http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm376516.htm
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/?term=23895806
- ↑ Peck, Peggy (September 17, 2010). "FDA Says It Will Review Pioglitazone Safety". MedPage Today. Retrieved 18 September 2010.
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||