Tenatoprazole
 | |
|---|---|
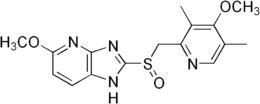
| Systematic (IUPAC) name | |
| (RS)-3-Methoxy-8-[(4-methoxy-3,5-dimethyl-pyridin-2-yl)methylsulfinyl]-2,7,9-triazabicyclo[4.3.0]nona-2,4,8,10-tetraene | |
| Clinical data | |
| Legal status | ? |
| Routes | Oral |
| Pharmacokinetic data | |
| Metabolism | Hepatic (CYP2C19-mediated) |
| Half-life | 4.8 to 7.7 hours |
| Identifiers | |
| CAS number | 113712-98-4 |
| ATC code | None |
| PubChem | CID 636411 |
| ChemSpider | 552196 |
| UNII | RE0689TX2K |
| Chemical data | |
| Formula | C16H18N4O3S |
| Mol. mass | 346.405 g/mol |
| SMILES
| |
| |
| | |
Tenatoprazole (rINN, also benatoprazole), discovered in Japan, is a proton pump inhibitor indicated for the treatment of reflux oesophagitis and peptic ulcer. Discovered by Mitsubishi Pharma, it is an imidazopyridine derivative and has an imidazopyridine ring in place of the benzimidazole moiety found in other proton pump inhibitors. It is activated slowly and its inhibition is said to be resistant to reversal. Tenatoprazole has an extended plasma half-life which makes it more effective in the treatment of nocturnal acid breakthrough than esomeprazole.[1]
Adverse effects
Antacid preparations such as tenatoprazole by suppressing acid mediated break down of proteins, leads to an elevated risk of developing food or drug allergies. This happens due to undigested proteins then passing into the gastrointestinal tract where sensitisation occurs. It is unclear whether this risk occurs with only long-term use or with short-term use as well.[2]
Pharmacological action
Tenatoprazole is a prodrug of the proton pump inhibitor (PPI) class, which is converted to the active sulfenamide or sulfenic acid by acid in the secretory canaliculus of the stimulated parietal cell of the stomach. This active species binds to luminally accessible cysteines of the gastric H+,K+ -ATPase resulting in disulfide formation and acid secretion inhibition. Tenatoprazole binds at the catalytic subunit of the gastric acid pump with a stoichiometry of 2.6 nmol mg(-1) of the enzyme in vitro. In vivo, maximum binding of tenatoprazole was 2.9 nmol mg(-1) of the enzyme at 2 h after IV administration. The binding sites of tenatoprazole were in the TM5/6 region at Cys813 and Cys822 as shown by tryptic and thermolysin digestion of the ATPase labeled by tenatoprazole. Decay of tenatoprazole binding on the gastric H+,K+ -ATPase consisted of two components. One was fast, with a half-life of 3.9 h due to reversal of binding at cysteine 813, and the other was a plateau phase corresponding to ATPase turnover reflecting binding at cysteine 822 that also results in sustained inhibition in the presence of reducing agents in vitro. The stability of inhibition and the long plasma half-life of tenatoprazole should result in prolonged inhibition of acid secretion as compared to omeprazole. The bioavailability of tenatoprazole was twofold greater in the (S)-tenatoprazole sodium salt hydrate form as compared to the free form due to differences in the crystal structure and hydrophobic nature of the two forms.
Pharmacodynamic studies on the same subjects showed an increase of intragastric pH with tenatoprazole 40 mg daily for seven days, significantly higher (p<0.05) than that observed with the same regimen of esomeprazole, the median pH being 4.6±0.9 and 4.2±0.8, respectively. In addition, the time spent above pH 4 at night after tenatoprazole administration was significantly longer than that observed with esomeprazole. The intragastric pH during the night was similarly higher (4.7±1.1 Units with tenatoprazole and 3.6±1.4 Units with esomeprazole, p<0.01), indicating better acid control.
A more recent pharmacodynamic and pharmacokinetic investigation did confirm and extended previous data showing the prolonged duration of acid suppression with tenatoprazole. The proportion of healthy volunteers spending at least 16 h above pH 4 in the 24 h period was remarkably higher with tenatoprazole than with esomeprazole (81.5% versus 34.5%, p<0.001) while the proportion of subjects with NAB was lower (73.1% versus 93.1%, p=0.06), although the difference fell short of statistical significance. Even 3 days after treatment was discontinued, mean 24 h pH, and percentage of time at pH>3 and pH>4 were significantly higher with tenatoprazole, indicating a sustained control of intragastric acidity with this novel PPI compared to esomeprazole. After 7 days repeated dosing, the maximal plasma concentration of tenatoprazole was almost six times higher than that of esomeprazole while AUC was 32 times higher. A significant correlation between AUC and percentage of time intragastric pH>4 was observed with tenatoprazole not only during but also after stopping treatment.
In summary, available studies point out both pharmacokinetic and pharmacodynamic advantages of tenatoprazole over esomeprazole. Since this last compound provides – amongst the members of the class — the most effective control of intragastric pH whatever the parameter considered, it is conceivable that tenatoprazole could similarly be better than the other existing PPIs. Tenatoprazole (as well as its S-isomer) appears a promising PPI for the treatment of acid-related diseases, where it has the potential to address unmet clinical needs.
References
- ↑ Galmiche J, Bruley Des Varannes S, Ducrotté P, Sacher-Huvelin S, Vavasseur F, Taccoen A, Fiorentini P, Homerin M (2004). "Tenatoprazole, a novel proton pump inhibitor with a prolonged plasma half-life: effects on intragastric pH and comparison with esomeprazole in healthy volunteers.". Aliment Pharmacol Ther 19 (6): 655–62. doi:10.1111/j.1365-2036.2004.01893.x. PMID 15023167.
- ↑ Pali-Schöll I, Jensen-Jarolim E (April 2011). "Anti-acid medication as a risk factor for food allergy". Allergy 66 (4): 469–77. doi:10.1111/j.1398-9995.2010.02511.x. PMID 21121928.
- Shin JM, Homerin M, Domagala F, Ficheux H, Sachs G (2006). "Characterization of the inhibitory activity of tenatoprazole on the gastric H+,K+ -ATPase in vitro and in vivo". Biochem. Pharmacol. 71 (6): 837–49. doi:10.1016/j.bcp.2005.11.030. PMID 16405921.
- Scarpignato C, Pelosini I (2006). "Review article: the opportunities and benefits of extended acid suppression". Aliment. Pharmacol. Ther. 23. Suppl 2 (s2): 23–34. doi:10.1111/j.1365-2036.2006.02945.x. PMID 16700900.
- Scarpignato C, Pelosini I, Di Mario F (2006). "Acid suppression therapy: where do we go from here?". Dig Dis 24 (1-2): 11–46. doi:10.1159/000091298. PMID 16699262.
| ||||||||||||||||||||||