Sciatic nerve
| Nerve: Sciatic Nerve | |
|---|---|
 | |
| Left gluteal region, showing surface markings for arteries and sciatic nerve | |
| Latin | Nervus ischiadicus |
| Gray's | p.960 |
| Innervates | Lateral rotator group (except piriformis and quadratus femoris) and the posterior compartment of thigh |
| From | Lumbar and sacral plexus (L4-S3) |
| To | Tibial and common fibular nerve |
The sciatic nerve (/saɪˈætɪk/; also called ischiadic nerve, ischiatic nerve) is a large nerve in humans and other animals. It begins in the lower back and runs through the buttock and down the lower limb. It is the longest and widest single nerve in the human body, going from the top of the leg to the foot on the posterior aspect.[1] The sciatic nerve supplies nearly the whole of the skin of the leg, the muscles of the back of the thigh, and those of the leg and foot. It is derived from spinal nerves L4 through S3. It contains fibres from both the anterior and posterior divisions of the lumbosacral plexus.
Course
The nerve exits the sciatic notch and runs anterior (deep) to piriformis. It then lies posterior (superficial) to the short external rotators (superior gemellus, inferior gemellus and obturator internus). It then runs down the posterior leg where it breaks into its three main divisions at the level of the mid thigh. The terminal branches are the common peroneal and tibial nerve.[2]
Branches
The nerve gives off articular and muscular branches.
- The articular branches (rami articulares) arise from the upper part of the nerve and supply the hip-joint, perforating the posterior part of its capsule; they are sometimes derived from the sacral plexus.
- The muscular branches (rami musculares) are distributed to the following muscles of the lower limb: biceps femoris, semitendinosus, semimembranosus, and the hamstring portion of adductor magnus. The nerve to the short head of the biceps femoris comes from the common fibular part of the sciatic (see below), while the other muscular branches arise from the tibial portion, as may be seen in those cases where there is a high division of the sciatic nerve.
The muscular branch eventually gives off the tibial nerve and common fibular nerve, which innervates the muscles of the (lower) leg. The tibial nerve goes on to innervate all muscles of the foot except the extensor digitorum brevis and the extensor hallucis brevis (which are innervated by the deep fibular nerve).

Sensory supply
The sciatic nerve innervates the skin on the posterior aspect of the thigh and gluteal regions, as well as the entire lower leg (except for its medial aspect).
Pathology
Pain caused by a compression or irritation of the sciatic nerve by a problem in the lower back is called sciatica. Common causes of sciatica include the following lower back and hip conditions: spinal disc herniation, degenerative disc disease, lumbar spinal stenosis, spondylolisthesis, and piriformis syndrome.[3] Other acute causes of sciatica include coughing, muscular hypertension, and sneezing.[4]
Sciatic nerve injury occurs between 0.5% and 2.0% of the time during total hip arthroplasty.[5] Sciatic nerve palsy is a complication of total hip arthroplasty with an incidence of 0.2% to 2.8% of the time, or with an incidence of 1.7% to 7.6% following revision.[6] Following the procedure, in rare cases, a screw, broken piece of trochanteric wire, fragment of methyl methacrylate bone cement, or Burch-Schneider metal cage can impinge on the nerve; this can cause sciatic nerve palsy which may resolve after the fragment is removed and the nerve freed. The nerve can be surrounded in oxidized regenerated cellulose to prevent further scarring. Sciatic nerve palsy can also result from severe spinal stenosis following the procedure, which can be addressed by spinal decompression surgery.[5][7]
Bernese periacetabular osteotomy resulted in major nerve deficits in the sciatic or femoral nerves in 2.1% of 1760 patients, of whom approximately half experienced complete recovery within a mean of 5.5 months.[8]
Sciatic nerve exploration can be done by endoscopy in a minimally invasive procedure to assess lesions of the nerve.[9] Endoscopic treatment for sciatic nerve entrapment has been investigated in deep gluteal syndrome; "Patients were treated with sciatic nerve decompression by resection of fibrovascular scar bands, piriformis tendon release, obturator internus, or quadratus femoris or by hamstring tendon scarring."[10]
Additional images
-

Sciatic nerve.
-

Sciatic nerve.
-
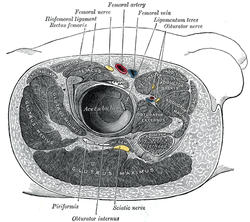
Structures surrounding right hip-joint.
-

Nerves of the right lower extremity. Posterior view.
-
Sciatic nerve.
-
Sciatic nerve.
-
Sciatic nerve.
-
Lumbar and sacral plexus. Deep dissection. Anterior view.
-
Lumbar and sacral plexus. Deep dissection. Anterior view.
-
Lumbar and sacral plexus. Deep dissection. Anterior view.
-
Lumbar and sacral plexus. Deep dissection. Anterior view.
-
Lumbar and sacral plexus. Deep dissection. Anterior view.
-
Lumbar and sacral plexus. Deep dissection. Anterior view.
-
Lumbar and sacral plexus. Deep dissection. Anterior view.
-
Lumbar and sacral plexus. Deep dissection. Anterior view.
-
Lumbar and sacral plexus. Deep dissection. Anterior view.
See also
- Gid hanasheh, Jewish Law related to the sciatic nerve
- Sciatica
References
- ↑ "sciatic nerve (anatomy)". Britannica Online Encyclopedia. Retrieved 23 April 2012.
- ↑ http://www.orthobullets.com/anatomy/10115/sciatic-nerve (accessed 12 Aug 2013)
- ↑ "Sciatica - Topic Overview". WebMD. 21 July 2010. Retrieved 23 April 2012.
- ↑ "What is sciatica: What causes sciatica?". MedicalBug. 11 April 2012. Retrieved 23 April 2012.
- ↑ 5.0 5.1 James B. Stiehl MD and William A. Stewart MD (1998). "Late Sciatic Nerve Entrapment Following Pelvic Plate Reconstruction in Total Hip Arthroplasty". The Journal of Arthroplasty 13 (5): 587–589.
- ↑ Alessandro Bistolfi et al. (2011). "Operative Management of Sciatic Nerve Palsy due to Impingement on the Metal Cage after Total Hip Revision: Case Report". Case Report Med. p. 830296.
- ↑ PMID 2290087 is cited by Stiehl and Stewart for the 0.5-2.0% figure.
- ↑ PMID 22684336
- ↑ PMID 15343436
- ↑ PMID 21071168
This article incorporates text from a public domain edition of Gray's Anatomy.
External links
- Sciatic_nerve at the Duke University Health System's Orthopedics program
- MedlinePlus Image 19503
- pelvis at The Anatomy Lesson by Wesley Norman (Georgetown University) (pelvicnerves)
- glutealregion at The Anatomy Lesson by Wesley Norman (Georgetown University) (glutealner)
- Sciatic Nerve - Cell Centered Database
- Sciatica and the Sciatic Nerve
| |||||||||||||||||||||||||||||||||||||||||||||||||||||











