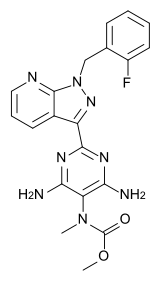
Riociguat
 | |
|---|---|
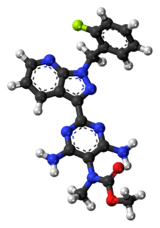 | |
| Systematic (IUPAC) name | |
| Methyl N-[4,6-Diamino-2-[1-[(2-fluorophenyl)methyl]-1H-pyrazolo[3,4-b]pyridin-3-yl]-5-pyrimidinyl]-N-methyl-carbaminate | |
| Clinical data | |
| Trade names | Adempas |
| AHFS/Drugs.com | entry |
| Pregnancy cat. | X (US) |
| Legal status | ℞-only (US) |
| Routes | oral |
| Pharmacokinetic data | |
| Half-life | 5–10 h |
| Identifiers | |
| CAS number | 625115-55-1 |
| ATC code | None |
| UNII | RU3FE2Y4XI |
| ChEBI | CHEBI:76018 |
| Chemical data | |
| Formula | C20H19FN8O2 |
| Mol. mass | 422.415 g/mol |
| SMILES
| |
| | |
Riociguat (BAY 63-2521, trade name Adempas) is a novel drug that is in clinical development by Bayer. It is a stimulator of soluble guanylate cyclase (sGC). At the moment Phase III clinical trials investigate the use of riociguat as a new approach to treat two forms of pulmonary hypertension (PH): chronic thromboembolic pulmonary hypertension (CTEPH) and pulmonary arterial hypertension (PAH). Riociguat constitutes the first drug of a novel class of sGC stimulators.[1]
Contraindications
Riociguat can cause fetal harm and is therefore contraindicated in pregnant women.[2]
Adverse effects
Serious adverse effects in clinical trials included bleeding. Hypotension (low blood pressure), headache, and gastrointestinal disorders also occurred.[2]
Interactions
Nitrates and phosphodiesterase inhibitors (including PDE5 inhibitors) increase the hypotensive (blood pressure lowering) effect of riociguat. Combining such drugs is therefore contraindicated. Riociguat levels in the blood are reduced by tobacco smoking and strong inhibitors of the liver enzyme CYP3A4, and increased by strong cytochrome inducers.[2]
Chemistry and mechanism of action
In healthy individuals nitric oxide (NO) acts as a signalling molecule on vascular smooth muscle cells to induce vasodilation. NO binds to soluble guanylate cyclase (sGC) and mediates the synthesis of the secondary messenger cyclic guanosine monophosphate (cGMP). sGC forms heterodimers consisting of a larger alpha-subunit and a smaller haem-binding beta-subunit. The synthesised cGMP acts as a secondary messenger and activates cGMP-dependent protein kinase (protein kinase G) to regulate cytosolic calcium ion concentration. This changes the actin–myosin contractility, which results in vasodilation. In patients with pulmonary arterial hypertension endothelial NO synthase, the enzyme that is responsible for the production of NO, is expressed to reduced levels. This results in overall lower levels of endothelial cell-derived NO and reduced vasodilation of smooth muscle cells. NO also reduces pulmonary smooth muscle cell growth and antagonises platelet inhibition, factors which play a key role in the pathogenesis of PAH.[3] In contrast to NO- and haem-independent sGC activators like cinaciguat, the sGC stimulator riociguat directly stimulates sGC activity independent of NO [4] and also acts in synergy with NO to produce anti-aggregatory, anti-proliferative, and vasodilatory effects.[5][6]
Pharmacology
Riociguat at concentration between 0.1 and 100 mmol stimulates in a dose-dependent manner sGC activity up to 73-fold. In addition, it acts synergistically with diethylamine/NO, the donor of NO, to increase sGC activity in vitro up to 112-fold.[7] A phase I study showed that riociguat is rapidly absorbed, and maximum plasma concentration is reached between 0.5–1.5 h.[8] The mean elimination half-life appears to be 5–10 hours.[8] Riociguat plasma concentrations have been also shown to be quite variable between patients, indicating that for clinical use it is probably necessary to titrate the drug specifically for each individual.
History
Discovery
The first nitric oxide (NO) independent, haem-dependent sGC stimulator YC-1, a synthetic benzylindazole derivative, was described in 1978.[9] The characterisation 20 years later demonstrated that as well as increasing sGC activity, YC-1 acted in synergy with NO to stimulate sGC. However, YC-1 was a relatively weak vasodilator and had side effects. Therefore, the search began for novel indazole compounds that were more potent and more specific sGC stimulators. The result was the identification of BAY 41-2272 and BAY 41-8543.[10] Both compounds were tested in various preclinical studies on different animal models and appeared to improve systemic arterial oxygenation. To improve the pharmacologic and pharmacokinetic profile an additional 1000 compounds were screened leading to the discovery of riociguat.[4][11] Riociguat was tested in mouse and rat disease models, where it effectively reduced pulmonary hypertension and reversed the associated right heart hypertrophy and ventricular remodelling.
Several clinical trials have been undertaken to investigate and evaluate diverse aspects of riociguat and some of them are still ongoing.[12]
Phase I clinical trials
One of the first studies was designed to test the safety profile, pharmacokinetics and pharmacodynamics of single oral doses of riociguat (0.25–5 mg). 58 healthy male subjects were given riociguat orally (oral solution or immediate-release tablet) in a randomised, placebo-controlled trial. Doses of riociguat were increased stepwise, and riociguat was well tolerated up to 2.5 mg.[8]
Phase II clinical trials
A proof-of-concept study, reported by the University of Gießen Lung Center, was the first small study (in 4 PAH patients) to investigate safety, tolerability, pharmacokinetics and efficacy parameters.[5] The drug was well-tolerated and superior to NO in efficacy and duration.
An open-label, non-controlled phase II trial of riociguat in 75 adult patients (42 with CTEPH and 33 with PAH, all in World Health Organization (WHO) functional class II or III) evaluated the safety and tolerability, and the effects on hemodynamics, exercise capacity and functional class. Riociguat was given three times daily for 12 weeks. Doses were titrated at 2-week intervals from 1.0 mg three times daily to a maximum of 2.5 mg three times daily. Riociguat had a favourable safety profile, and also significantly improved exercise capacity and hemodynamic parameters such as pulmonary vascular resistance, cardiac output and pulmonary arterial pressure compared to baseline values.[13]
In addition, a phase II study of riociguat is underway in patients suffering from other forms of PH such as associated with interstitial lung disease (PH-ILD). First results from this study are expected in 2011.[14]
Phase III clinical trials
The phase III trials on riociguat are multi-center studies. The study program includes large randomized, double-blind, placebo-controlled pivotal trial phase (CHEST-1 and PATENT-1), and open-label extensions of these studies (CHEST-2 and PATENT-2). Details of these studies are reported on ClinicalTrials.gov, a register of studies maintained by the National Institutes of Health (NIH).[12]
CHEST
The Chronic Thromboembolic Pulmonary Hypertension sGC-Stimulator Trial (CHEST) is a randomized, placebo-controlled trial that is aimed to analyse the efficacy and safety of riociguat in CTEPH patients.[1] After a 16 week riociguat treatment the patient’s exercise capacity will be evaluated by measuring the change in the six-minute walk test (6-MWT).[15] Patients having completed CHEST-1 will be invited to enter the extension trial, CHEST-2. The trial is ongoing as of December 2009.[16]
PATENT
The Pulmonary Arterial Hypertension sGC-Stimulator Trial (PATENT) is a randomized, placebo-controlled trial that investigates the efficacy and safety of riociguat in PAH patients.[1] After a 12 week treatment the patient’s exercise capacity will be evaluated by measuring the change in the 6-MWT.[17] Patients having completed PATENT-1 will be invited to enter the extension trial, PATENT-2.[18] The trial is ongoing as of December 2009.
Other studies
Effect of riociguat on bone metabolism
This randomized, double blind, placebo controlled Phase I study investigates the effect of riociguat, administered as 2.5 mg immediate-release (IR)-tablets twice daily over 14 days, on the bone metabolism.[19] Final data collection is expected in December 2009.
Interaction study with sildenafil
This study investigates safety, tolerability, pharmacokinetics and the impact on pulmonary and systemic haemodynamics of single doses of 0.5 and 1 mg of riociguat in patients with PAH and stable treatment of sildenafil (20 mg thrice daily) in a non-randomized uncontrolled trial.[20] The study has been completed in Aug 2009, results are outstanding as of December 2009.
See also
- Cinaciguat, a sGC activator (not sCG stimulator).
- PDE5 inhibitors act downstream in the nitric oxide signalling pathway, reducing cyclic GMP degradation.
- Endothelin receptor antagonist, another class of drugs used in PAH
References
- ↑ 1.0 1.1 1.2 "Background Riociguat". Bayer HealthCare. Retrieved 15 December 2009.
- ↑ 2.0 2.1 2.2 FDA Professional Drug Information
- ↑ Giaid A, Saleh D (July 1995). "Reduced expression of endothelial nitric oxide synthase in the lungs of patients with pulmonary hypertension". The New England Journal of Medicine 333 (4): 214–21. doi:10.1056/NEJM199507273330403. PMID 7540722.
- ↑ 4.0 4.1 Evgenov OV, Pacher P, Schmidt PM, Haskó G, Schmidt HH, Stasch JP (September 2006). "NO-independent stimulators and activators of soluble guanylate cyclase: discovery and therapeutic potential". Nature Reviews. Drug Discovery 5 (9): 755–68. doi:10.1038/nrd2038. PMC 2225477. PMID 16955067.
- ↑ 5.0 5.1 Grimminger F, Weimann G, Frey R, et al. (April 2009). "First acute haemodynamic study of soluble guanylate cyclase stimulator riociguat in pulmonary hypertension". The European Respiratory Journal 33 (4): 785–92. doi:10.1183/09031936.00039808. PMID 19129292.
- ↑ Stasch JP, Hobbs AJ (2009). "NO-independent, haem-dependent soluble guanylate cyclase stimulators". Handbook of Experimental Pharmacology. Handbook of Experimental Pharmacology 191 (191): 277–308. doi:10.1007/978-3-540-68964-5_13. ISBN 978-3-540-68960-7. PMID 19089334.
- ↑ Schermuly RT, Stasch JP, Pullamsetti SS, et al. (October 2008). "Expression and function of soluble guanylate cyclase in pulmonary arterial hypertension". The European Respiratory Journal 32 (4): 881–91. doi:10.1183/09031936.00114407. PMID 18550612.
- ↑ 8.0 8.1 8.2 Frey R, Mück W, Unger S, Artmeier-Brandt U, Weimann G, Wensing G (December 2008). "Pharmacokinetics, pharmacodynamics, tolerability, and safety of the soluble guanylate cyclase activator cinaciguat (BAY 58-2667) in healthy male volunteers". Journal of Clinical Pharmacology 48 (12): 1400–10. doi:10.1177/0091270008322906. PMID 18779378.
- ↑ Yoshina S, Tanaka A, Kuo SC (March 1978). "Studies on heterocyclic compounds. XXXVI. Synthesis of furo[3,2-c]pyrazole derivatives. (4) Synthesis of 1,3-diphenylfuro[3,2-c]pyrazole-5-carboxaldehyde and its derivatives (author's transl)". Yakugaku Zasshi (in Japanese) 98 (3): 272–9. PMID 650406.
- ↑ Stasch JP, Becker EM, Alonso-Alija C, et al. (March 2001). "NO-independent regulatory site on soluble guanylate cyclase". Nature 410 (6825): 212–5. doi:10.1038/35065611. PMID 11242081.
- ↑ Mittendorf J, Weigand S, Alonso-Alija C, et al. (May 2009). "Discovery of riociguat (BAY 63-2521): a potent, oral stimulator of soluble guanylate cyclase for the treatment of pulmonary hypertension". Chemmedchem 4 (5): 853–65. doi:10.1002/cmdc.200900014. PMID 19263460.
- ↑ 12.0 12.1 ClinicalTrials.gov: Riociguat
- ↑ "ATS International conference". American Thoracic Society. 2009.
- ↑ ClinicalTrials.gov NCT00694850 Impact of Multiple Doses of BAY 63-2521 on Safety, Tolerability, Pharmacokinetics and Pharmacodynamics in Patients With Interstitial Lung Disease (ILD) Associated Pulmonary Hypertension
- ↑ ClinicalTrials.gov NCT00855465 A Study to Evaluate Efficacy and Safety of Oral BAY63-2521 in Patients With CTEPH
- ↑ ClinicalTrials.gov NCT00910429 BAY63-2521 - Long-term Extension Study in Patients With Chronic Thromboembolic Pulmonary Hypertension
- ↑ ClinicalTrials.gov NCT00810693 A Study to Evaluate Efficacy and Safety of Oral BAY63-2521 in Patients With Pulmonary Arterial Hypertension (PAH)
- ↑ ClinicalTrials.gov NCT00863681 BAY63-2521:Long-term Extension Study in Patients With Pulmonary Arterial Hypertension
- ↑ ClinicalTrials.gov NCT00855660 Effect of Riociguat on Bone Metabolism
- ↑ ClinicalTrials.gov NCT00680654 Interaction Study in Patients With Pulmonary Hypertension and Stable Treatment of Sildenafil 20 mg TID