Radiation treatment planning

In radiotherapy, radiation treatment planning is the process in which a team consisting of radiation oncologists, radiation therapist, medical physicists and medical dosimetrists plan the appropriate external beam radiotherapy or internal brachytherapy treatment technique for a patient with cancer.
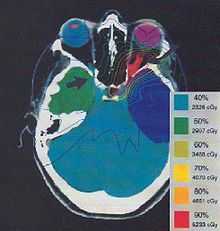
Typically, medical imaging (i.e., x-ray computed tomography often the primary image set for treatment planning, magnetic resonance imaging excellent secondary image set for soft tissue contouring, and positron emission tomography less commonly used and reserved for cases where specific uptake studies can enhance planning target volume delineation) are used to form a virtual patient for a computer-aided design procedure. Treatment simulations are used to plan the geometric, radiological, and dosimetric aspects of the therapy using radiation transport simulations and optimization. For intensity modulated radiation therapy (IMRT), this process involves selecting the appropriate beam energy (photons, and perhaps protons), energy (e.g. 6 MV, 18 MV) and arrangements. For brachytherapy, involves selecting the appropriate catheter positions and source dwell times[1][2] (in HDR brachytherapy) or seeds positions (in LDR brachytherapy). The more formal optimization process is typically referred to as forward planning and inverse planning.[3][4] Plans are often assessed with the aid of dose-volume histograms, allowing the clinician to evaluate the uniformity of the dose to the diseased tissue (tumor) and sparing of healthy structures.
Today, treatment planning is almost entirely computer based using patient computed tomography (CT) data sets. Modern treatment planning systems provide tools for multimodality image matching, also known as image coregistration or fusion.
Forward planning
Forward planning is a technique used in external-beam radiotherapy to produce a treatment plan. In forward planning, a treatment Medical physicist places beams into a radiotherapy treatment planning system which can deliver sufficient radiation to a tumour while both sparing critical organs and minimising the dose to healthy tissue. The required decisions include how many radiation beams to use, which angles each will be delivered from, whether attenuating wedges be used, and which multileaf collimator configuration will be used to shape the radiation from each beam.
Once the treatment planner has made an initial plan, the treatment planning system calculates the required monitor units to deliver a prescribed dose to a specific area in the patient which is dependant on beam modifiers that include wedges, specialized collimation, field sizes, tumor depth, etc. The information from a prior CT scan of the patient allows more accurate modeling of the behaviour of the radiation as it travels through the patient's tissues. Different dose prediction models are available, including pencil beam, convolution-superposition and monte carlo simulation, with precision versus computation time being the relevant trade-off.
This type of planning is used for the majority of external-beam radiotherapy treatments, but is only sufficiently adept to handle relatively simple cases—cases in which the tumour has a simple shape and is not near any critical organs. For more sophisticated plans, inverse planning is used to create an intensity-modulated treatment plan. This is now also used as a part of post-mastectomy radiotherapy (PMRT) planning.
Inverse planning
Inverse planning is a technique used to design a radiotherapy treatment plan. A radiation oncologist defines a patient's critical organs and tumour then Physicist gives target doses and importance factors for each. Then, an optimisation program is run to find the treatment plan which best matches all the input criteria.
The term "inverse planning" is somewhat of a misnomer; it was devised in contrast to the manual trial-and-error process known in oncology as "forward planning". It has stuck for historical reasons. Outside of the field of oncology, this procedure would be better described as "automated planning".
HIPO (Hybrid Inverse Planning & Optimization), developed by Pi-Medical Ltd., is one algorithm.
List of Radiation Treatment Planning Systems (RTPS)
Commercial
- ScandiPlan (Scanditronix - commercial release of UMPlan)
- ADAC -> Pinnacle3(Philips Healthcare)
- ISOgray (DOSIsoft)
- BrainSCAN -> Brainlab; predecessor of iPlan RT Dose
- CAT3D -> Mevis
- Focus -> XiO (CMS, recently purchased by Elekta) [5]
- iPlan RT Dose -> Brainlab ; successor of BrainSCAN [6]
- Render-Plan 3-D -> PrecisePLAN (Elekta)
- Monaco (CMS/Elekta)
- Theraplan Plus (Theratronics -> Nucletron)
- Oncentra MasterPlan - External Beam and Brachy Therapy (Nucletron)
- Oncentra Prostate - Prostate HDR Brachytherapy (Nucletron / developed by Pi-Medical & MedCom)
- Oncentra GYN - Gynecologic brachytherapy (Nucletron / developed by Pi-Medical & MedCom)
- Plato RTS (Nucletron)
- Plato BPS (Nucletron)
- Cad Plan - predecessor of Eclipse Varian Medical Systems
- Corvus (Nomos)
- RAHD
- ROCS
- Simuplan Planning System
- GE
- KLZ Healthcare
- Prowess
- Brachyvision (Varian)
- Gammaknife (Elekta)
- RIT
- Eclipse - designed by Varian Medical Systems; successor of the CadPlan System
- VariSeed - Prostate LDR Brachytherapy (Varian)
- XKnife (Integra Radionics)
Non-commercial
- UMPlan - The University of Michigan Comprehensive 3D Treatment Planning System
- GRATIS - George's RAdiotherapy Treatment desIgn System (project discontinued and not available any more)
- PLUNC (planning system written by University of North Carolina-Chapel Hill
- Prism (planning system written by Prof Ira Kalet at University of Washington)
- MMCTP (McGill Monte Carlo Treatment Planning system)
References
- ↑ Karabis A., Belloti P. and Baltas D. Optimization of Catheter Position and Dwell Time in Prostate HDR Brachytherapy using HIPO and Linear Programming WC in Med. Physics & Biomedical Eng., Sept. 7-12, 2009, Munich, Germany, IFMBE Proceedings, O. Dössel and W.C. Schlegel (Eds.), Vol. 25/I, pp. 612-615, Springer, 2009
- ↑ Lahanas M,Baltas D,Giannouli S (2003) Global convergence analysis of fast multiobjective gradient-based dose optimization algorithms for high-dose-rate brachytherapy. Phys Med Biol 48:599-617
- ↑ Galvin, JM; Ezzel, G; Eisbrauch, A; Yu, C; Butler, B; Xiao, Y; Rosen, I; Rosenman, J et al. (April 2004), "Implementing IMRT in clinical practice: a joint document of the American Society for Therapeutic Radiology and Oncology and the American Association of Physicists in Medicine.", Int J Radiat Oncol Biol Phys. 58 (5): 1616–34., doi:10.1016/j.ijrobp.2003.12.008, PMID 15050343
- ↑ Hendee W., Ibbott G. and Hendee E. (2005). Radiation Therapy Physics. Wiley-Liss Publ. ISBN 0-471-39493-9.
- ↑ Elekta negotiates to acquire CMS (copy from original)
- ↑ RT Treatment Planning Software Brainlab. Retrieved 2013-05-22.