Pyridoxine deficiency
| Vitamin B6 deficiency | |
|---|---|
| Classification and external resources | |
 | |
| ICD-10 | E53.1 |
| ICD-9 | 266.1 |
| DiseasesDB | 13923 |
| eMedicine | med/1977 |
| MeSH | D026681 |
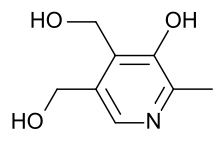
Pyridoxine deficiency (also known as B6 deficiency) is a paediatric disease due to a lack of pyridoxine (or vitamin B6). It usually becomes noticeable within the first 12 months of life in infants with a lack of pyridoxine, a coenzyme responsible for numerous essential metabolic reactions in humans. It is rarely observed, even in developing countries.[1][2]
Symptoms
The disease presents with several key symptoms including seizures, irritability, cheilitis (inflammation of the lips), conjunctivitis and neurologic symptoms. In patients receiving isoniazid, pyridoxine deficiency can lead to a sideroblastic anemia because pyridoxine is a required cofactor in heme synthesis.
Rare forms
Familial pyridoxine-dependent epilepsy causes seizures at birth or shortly afterwards. It has been speculated that the cause of seizures in pyridoxine deficiency lies with abnormalities in the normal ratio of glutamic acid to GABA.[1] Association is noted with ALDH7A1 gene. Irritability and other neurologic symptoms, such as confusion, are common place.[2] Anemia has also been documented as a symptom.[1]
Causes
The main cause of pyridoxine deficiency is a lack of pyridoxine in the diet. Another cause of vitamin B6 deficiency is the use of the tuberculostatic medication isoniazid, and for this reason, it is usually replaced with vitamin B6 whilst using this drug.[2]
Pathophysiology
Decarboxylation of glutamic acid to gamma-aminobutyric acid (GABA, a neurotransmitter) and transamination of glutamic acid to alpha-ketoglutaric acid are both impaired in animals when suffering from pyridoxine deficiency.[1] Neurological symptoms are most likely due to diminished affinity of pyridoxine for the apoenzyme, which can only be overcome by increasing tissue concentrations of the enzyme.[1]
Diagnosis
Pyridoxine deficiency is a very rare condition, even in developing countries. A handful of cases were seen in between 1952 and 1953, particularly in the United States, and occurred in a small percentage of infants who were fed a formula lacking in pyridoxine.[1] A positive diagnosis test for pyridoxine deficiency can be ascertained by measuring erythrocyte levels of aspartate aminotransferase and transketolase in serum.[2]
Treatment
Treatment of pyridoxine deficiency lies with replacing the missing vitamin. Penicillamine or hydrazides, such as isoniazid, are rarely used due to their ability to provoke deficiency symptoms.[1]
References
| |||||||||||||||||||||||||