Polymyalgia rheumatica
| Polymyalgia rheumatica | |
|---|---|
| Classification and external resources | |
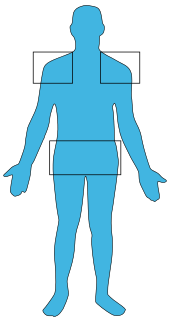 In polmyalgia rheumatica (PMR), pain is usually located in the shoulders and hips. | |
| ICD-10 | M35.3 |
| ICD-9 | 725 |
| DiseasesDB | 10331 |
| MedlinePlus | 000415 |
| eMedicine | emerg/473 |
| MeSH | D011111 |
Polymyalgia rheumatica (which takes its name from the word "polymyalgia" which means "pain in many muscles" in Greek followed by the term "rheumatica") abbreviated as PMR, is a syndrome with pain or stiffness, usually in the neck, shoulders, and hips. The pain can be very sudden, or can occur gradually over a period. It may be caused by an inflammatory condition of blood vessels such as temporal arteritis.
Most PMR sufferers wake up in the morning with pain in their muscles; however, there have been cases in which the patient has developed the pain during the evenings.[1] Patients who have polymyalgia rheumatica may also have temporal arteritis, an inflammation of blood vessels in the face which can cause blindness if not treated quickly.
PMR is usually treated with courses of oral corticosteroids.[2] Most people need to continue the corticosteroid treatment for two to three years.[3] PMR usually goes away on its own in a year or two, but medications and self-care measures can improve the rate of recovery.[4]
Symptoms and signs
There are a wide range of symptoms that indicate if a person has polymyalgia rheumatica. The classic symptoms include:
- Pain and stiffness (moderate to severe) in the neck, shoulders, and hips, which inhibits activity, especially in the morning/after sleeping.
- Fatigue and lack of appetite (possibly leading to weight loss) are also indicative of polymyalgia rheumatica.
- Anemia
- An overall feeling of illness
- Low-grade (mild) fever[5]
About 15% of people who are diagnosed with polymyalgia rheumatica also have temporal arteritis, and about 50% of people with temporal arteritis have polymyalgia rheumatica. Some symptoms of temporal arteritis include headaches, scalp tenderness, jaw or facial soreness, distorted vision or aching in the limbs caused by decreased blood flow, and fatigue.[1]
Causes
The cause of PMR is not well understood. The pain and stiffness result from the activity of inflammatory cells and proteins that are normally a part of the body's disease-fighting immune system, and the inflammatory activity seems to be concentrated in tissues surrounding the affected joints.[6] During this disorder, the white blood cells in the body attack the lining of the joints, causing inflammation.[7] Recent studies have found that inherited factors also play a role in the probability that an individual will develop polymyalgia rheumatica. Several theories have included viral stimulation of the immune system in genetically susceptible individuals.[8]
Infectious disease may be a contributing factor. This would be expected with sudden onset of symptoms for example. In addition, appearance of new cases often appear in cycles in the general population, implying a viral connection. Studies are inconclusive, however several somewhat common viruses were identified as possible triggers for PMR.[6] The viruses thought to be involved include the adenovirus, which causes respiratory infections; the human parvovirus B19, an infection that affects children; and the human parainfluenza virus.[7]
People who have the HLA-DR4 type of human leucocyte antigen appear to have a higher risk of polymyalgia rheumatica.[9]
One reported cause is food sensitivities. Sufferers often do not know they are affected by them, but medical tests exist to verify.[citation needed]
Diagnosis
There is no specific test to diagnose polymyalgia rheumatica. There are many other diseases which cause inflammation and pain in muscles, but there are a few tests that can help narrow down the cause of the pain. Limitation in shoulder motion, or swelling of the joints in the wrists or hands are noted by the doctor.[8] A patient's answers to questions, a general physical exam, and the results of tests can help a doctor determine the cause of pain and stiffness.[10]
One blood test that is usually performed is the erythrocyte sedimentation rate (ESR) which measures how fast the patient's red blood cells settle in a test tube. The faster the blood cells settle, the higher the ESR value, which means that there is inflammation. Many conditions can cause an elevated ESR, so this test alone is not proof that a person has polymyalgia rheumatica.[10][11]
Another test that checks the level of C-reactive protein (CRP) in the blood may also be conducted. CRP is produced by the liver in response to an injury or infection and people with polymyalgia rheumatica usually have high levels.[10][11] However, like the ESR, this test is also very non-specific.
Polymyalgia rheumatica is sometimes associated with temporal arteritis, a condition requiring more aggressive therapy. To test for this additional disorder, a biopsy sample may be taken of the temporal artery.[10]
Treatment
Prednisone is the drug of choice for PMR[12] and treatment duration is frequently greater than one year.[8] If the patient does not experience dramatic improvement after three days of 10–20 mg oral prednisone per day, the diagnosis should be reconsidered.[13]
Non steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen are ineffective in the initial treatment of PMR,[14] but they may be used in conjunction with the maintenance dose of corticosteroid.[15]
Along with medical treatment, patients are encouraged to exercise and eat healthily. Exercise will help strengthen the weak muscles, and help to prevent weight gain. A healthy diet will help to keep a strong immune system, and also help build strong muscles and bones.[16] Eat a diet of fruits, vegetables, whole grains, and low-fat meat and dairy products. Avoid foods with high levels of refined sugars and salt (sodium).[17]
Epidemiology
There are no certain circumstances for which an individual will get polymyalgia rheumatica, but there are a few factors that show a relationship with the disorder.
- Usually affects adults over the age of 60[1]
- The average age of a person who has PMR is about 70 years old[1][18]
- Women are twice as likely to get PMR as men[18]
- Caucasians are more likely to get this disease.[1] It is more likely to affect people of Northern European origin; Scandinavians are especially vulnerable.[18]
- 50% of people with temporal arteritis also have polymyalgia rheumatica[1]
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Gelfand JL (November 18, 2007). "Polymyalgia Rheumatica and Temporal Arteritis". WebMD. Retrieved 2008-06-10.
- ↑ Polymyalgia rheumatica at eMedicine
- ↑ "Polymyalgia Rheumatica treatments and drugs". MayoClinic. Dec 4, 2010. Retrieved 2012-01-19.
- ↑ "Polymyalgia Rheumatica definition". MayoClinic. May 17, 2008. Retrieved 2012-01-19.
- ↑ "Polymyalgia Rheumatica symptoms". MayoClinic. Dec 4, 2010. Retrieved 2012-01-19.
- ↑ 6.0 6.1 "Polymyalgia Rheumatica causes". MayoClinic. Dec 4, 2010. Retrieved 2012-01-19.
- ↑ 7.0 7.1 "Polymyalgia Rheumatica causes". MayoClinic. May 17, 2008. Retrieved 2012-01-19.
- ↑ 8.0 8.1 8.2 Shiel Jr WC (2008-03-13). "Polymyalgia Rheumatica (PMR) & Giant Cell Arteritis (Temporal Arteritis)". MedicineNet. Retrieved 2008-06-10.
- ↑ Page 255 in: Elizabeth D Agabegi; Agabegi, Steven S. (2008). Step-Up to Medicine (Step-Up Series). Hagerstwon, MD: Lippincott Williams & Wilkins. ISBN 0-7817-7153-6.
- ↑ 10.0 10.1 10.2 10.3 "Polymyalgia Rheumatica tests and diagnosis". MayoClinic. Dec 4, 2010. Retrieved 2012-01-19.
- ↑ 11.0 11.1 "Polymyalgia Rheumatica tests and diagnosis". MayoClinic. May 17, 2008. Retrieved 2012-01-19.
- ↑ Hernández-Rodríguez J, Cid MC, López-Soto A, Espigol-Frigolé G, Bosch X (November 2009). "Treatment of polymyalgia rheumatica: a systematic review". Arch. Intern. Med. 169 (20): 1839–50. doi:10.1001/archinternmed.2009.352. PMID 19901135.
- ↑ McPhee, Stephen J.; Papadakis, Maxine A. 2010 Current Medical Diagnosis and Treatment. p. 767.
- ↑ Docken WP (August 2009). "Polymyalgia rheumatica". American College of Rheumatology. Retrieved 2012-01-20.
- ↑ MDGuidelines (August 1991-2010). "Polymyalgia rheumatica". Reed Group. Retrieved 2012-01-20.
- ↑ "Polymyalgia Rheumatica lifestyle and home remedies". MayoClinic. May 17, 2008. Retrieved 2012-01-19.
- ↑ "Polymyalgia Rheumatica lifestyle and home remedies". MayoClinic. Dec 4, 2010. Retrieved 2012-01-19.
- ↑ 18.0 18.1 18.2 "Polymyalgia Rheumatica risk factors". MayoClinic. Dec 4, 2010. Retrieved 2012-01-19.
External links
| |||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||