Orthognathic surgery
| Orthognathic surgery | |
|---|---|
| Intervention | |
| ICD-9-CM | 76.6 |
Orthognathic surgery /ˌɔrθəɡˈnæθɨk/[1] is surgery to correct conditions of the jaw and face related to structure, growth, sleep apnea, TMJ disorders, malocclusion problems owing to skeletal disharmonies, or other orthodontic problems that cannot be easily treated with braces. Originally coined by Dr. Harold Hargis, D.M.D., it is also used in treatment of congenital conditions like cleft palate.[2] Bones can be cut and re-aligned, then held in place with either screws or plates. Orthognathic surgery can also be referred to as corrective jaw surgery.[3]
Indications
- Gross jaw discrepancies (Anteroposterior, Vertical and /or Transverse discrepancies).[4]
- Facial skeletal discrepancies associated with documented sleep apnea, airway defects, and soft tissue discrepancies.
- Facial skeletal discrepancies associated with documented temporomandibular joint pathology.
Surgery
Orthognathic surgery is performed by an oral and maxillofacial surgeon in collaboration with an orthodontist. It often includes braces before and after surgery, and retainers after the final removal of braces. Orthognathic surgery is often needed after reconstruction of cleft palate or other major craniofacial anomalies. Careful coordination between the surgeon and orthodontist is essential to ensure that the teeth will fit correctly after the surgery.
Planning
Planning for the surgery usually involves input from a multidisciplinary team. Involved professionals are oral and maxillofacial surgeons, plastic surgeons, ENT surgeons, orthodontists, and speech and language therapist. As the surgery usually results in a noticeable change in the patient's face a psychological assessment is occasionally required to assess patient's need for surgery and its predicted effect on the patient.
Radiographs and photographs are taken to help in the planning and there is software to predict the shape of the patient's face after surgery,[5][6] which is useful both for planning and for explaining the surgery to the patient and the patient's family.[7] Advanced software can allow the patient to see the predicted results of the surgery.
The main goals of orthognathic surgery are to achieve a correct bite, an aesthetic face and an enlarged airway. While correcting the bite is important, if the face is not considered the resulting bony changes might lead to an unaesthetic result.[8] Orthognathic surgery is also available as a very successful treatment (90–100%) for obstructive sleep apnea.[9] Great care needs to be taken during the planning phase to maximize airway patency.
Procedure
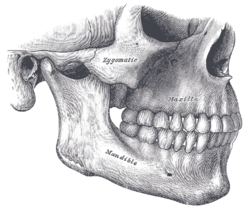
The surgery might involve one jaw or the two jaws during the same procedure. The modification is done by making cuts in the bones of the mandible and / or maxilla and repositioning the cut pieces in the desired alignment. Usually surgery is performed under general anaesthetic and using nasal tube for intubation rather than the more commonly used oral tube; this is to allow wiring the teeth together during surgery. The surgery often does not involve cutting the skin, and instead, the surgeon is often able to go through the inside of the mouth.
Cutting the bone is called osteotomy and in case of performing the surgery on the two jaws at the same time it is called a bi-maxillary osteotomy (two jaws bone cutting) or a maxillomandibular advancement. The bone cutting is traditionally done using special electrical saws and burs, and manual chisels. Recently a machine that can make the bone cuts using ultra-sound waves has been introduced; this is yet to be used on a wide scale. The maxilla can be adjusted using a "Lefort I" level osteotomy (most common). Sometimes the midface can be mobilised as well by using a Lefort II, or Lefort III osteotomy. These techniques are utilized extensively for children suffering from certain craniofacial abnormalities such as Crouzon syndrome.
The jaws will be wired together (inter-maxillary fixation) using stainless steel wires during the surgery to ensure the correct re-positioning of the bones. This in most cases is released before the patient wakes up. Some surgeons prefer to wire the jaws shut.
In some cases, the changing of the jaw structure will cause the cheeks to become depressed and shallow. Some procedures will call for the insertion of implants to give the patient's face a fuller look.[10][11]
Complications
Like any other surgery, there can be some complications such as bleeding, swelling, infection, nausea and vomiting.[12] There could also be some numbness in the face due to nerve damage. The numbness may be either temporary, or, more rarely, permanent.[13] In general, complications of this surgery occur infrequently.[14]
If the surgery involved the upper jaw, then the surgery could have an effect on the shape of the patient's nose. This can be minimised by careful planning and accurate execution of the surgical plan. Sometimes, this is considered part of the benefit.
Post operation
After orthognathic surgery, patients are often required to adhere to an all-liquid diet. After time, soft food can be introduced, and then hard food. Diet is very important after the surgery, to accelerate the healing process. Weight loss due to lack of appetite and the liquid diet is common, but should be avoided if possible. Normal recovery time can range from a few weeks for minor surgery, to up to a year for more complicated surgery.
For some surgeries, pain may be minimal due to minor nerve damage and lack of feeling. Doctors will prescribe pain medication and prophylactic antibiotics to the patient. There is often a large amount of swelling around the jaw area, and in some cases bruising. Most of the swelling will disappear in the first few weeks, but some may remain for a few months.
The surgeon will see the patient for check-ups frequently, to check on the healing, check for infection, and to make sure nothing has moved. The frequency of visits will decrease over time. If the surgeon is unsatisfied with the way the bone is mending, she/he may recommend additional surgery to rectify whatever may have shifted. It is very important to avoid any chewing until the surgeon is satisfied with the healing.
See also
References
- ↑ US dict: ôr′·thəg·năth′·ĭk
- ↑ Bill J, Proff P, Bayerlein T, Blens T, Gedrange T, Reuther J (September 2006). "Orthognathic surgery in cleft patients". J Craniomaxillofac Surg 34 (Suppl 2): 77–81. doi:10.1016/S1010-5182(06)60017-6. PMID 17071397.
- ↑ Maxillofacialcentre.com
- ↑ American Association of Oral and Maxillofacial Surgeons
- ↑ Mischkowski RA, Zinser MJ, Kübler AC, Krug B, Seifert U, Zöller JE (December 2006). "Application of an augmented reality tool for maxillary positioning in orthognathic surgery — a feasibility study". J Craniomaxillofac Surg 34 (8): 478–83. doi:10.1016/j.jcms.2006.07.862. PMID 17157519.
- ↑ Uechi J, Okayama M, Shibata T, et al. (December 2006). "A novel method for the 3-dimensional simulation of orthognathic surgery by using a multimodal image-fusion technique". Am J Orthod Dentofacial Orthop 130 (6): 786–98. doi:10.1016/j.ajodo.2006.03.025. PMID 17169742.
- ↑ Tsuji M, Noguchi N, Shigematsu M, et al. (September 2006). "A new navigation system based on cephalograms and dental casts for oral and maxillofacial surgery". Int J Oral Maxillofac Surg 35 (9): 828–36. doi:10.1016/j.ijom.2006.02.024. PMID 16690251.
- ↑ Arnett GW, Gunson MJ (September 2004). "Facial planning for orthodontists and oral surgeons". Am J Orthod Dentofacial Orthop 126 (3): 290–5. doi:10.1016/S0889540604005232. PMID 15356488.
- ↑ Prinsell JR (December 1999). "Maxillomandibular advancement surgery in a site-specific treatment approach for obstructive sleep apnea in 50 consecutive patients". Chest 116 (6): 1519–29. PMID 10593771.
- ↑ I received this procedure three years ago.
- ↑ http://www.lpsa.co.uk/chin-cheeks-jaw-surgery
- ↑ Silva AC, O'Ryan F, Poor DB (September 2006). "Postoperative nausea and vomiting (PONV) after orthognathic surgery: a retrospective study and literature review". J. Oral Maxillofac. Surg. 64 (9): 1385–97. doi:10.1016/j.joms.2006.05.024. PMID 16916674.
- ↑ Eckert AW, Maurer P, Kriwalsky MS, Schubert J (September 2006). "P.292 Complications in orthognathic surgery". J Craniomaxillofac Surg 34 (Suppl 1): 206. doi:10.1016/S1010-5182(06)60797-X.
- ↑ Panula K, Finne K, Oikarinen K (October 2001). "Incidence of complications and problems related to orthognathic surgery: a review of 655 patients". J. Oral Maxillofac. Surg. 59 (10): 1128–36; discussion 1137. doi:10.1053/joms.2001.26704. PMID 11573165.
| ||||||||||||||||||||||||||||||||||||||||||||||||||