Neuromyelitis optica
| Devic's disease | |
|---|---|
| Classification and external resources | |
| ICD-10 | G36.0 |
| ICD-9 | 341.0 |
| DiseasesDB | 29470 |
| MeSH | D009471 |
Neuromyelitis optica (NMO), also known as Devic's disease or Devic's syndrome, is an heterogeneous condition consisting of recurrent and simultaneous inflammation and demyelination of the optic nerve (optic neuritis) and the spinal cord (myelitis).
Currently at least two different causes are proposed based on the presence of autoantibodies against AQP4. AQP4+ NMO is currently considered an autoimmune disease (autoimmune astrocytopathy, or autoimmune astrocytic channelopathy) in which a person's own immune system attacks the astrocytes of the optic nerves and spinal cord. The cause of the AQP4- variants is unknown.
Although inflammation may also affect the brain, the lesions are different from those observed in the related condition, multiple sclerosis.[1] Spinal cord lesions lead to varying degrees of weakness or paralysis in the legs or arms, loss of sensation (including blindness),[2] and/or bladder and bowel dysfunction.[3]
Devic's disease is a rare disorder which resembles multiple sclerosis (MS) in several ways, but requires a different course of treatment for optimal results.[3] It has also been suggested to be a variant form of acute disseminated encephalomyelitis.[4]
In AQP+ variants, CNS astrocytes, which are the basis for the glymphatic system [5] are the target of the autoimmune attack.
Symptoms
The main symptoms of Devic's disease are loss of vision and spinal cord function. Optic neuritis may manifest as visual impairment with decreased visual acuity, although visual field defects, or loss of color vision may occur in isolation or prior to formal loss of acuity. Spinal cord dysfunction can lead to muscle weakness, reduced sensation, or loss of bladder and bowel control.[6] The typical patient has an acute and severe spastic weakness of the legs (paraparesis) or all four limbs (quadriparesis) with sensory signs, often accompanied by loss of bladder control.
Mechanism
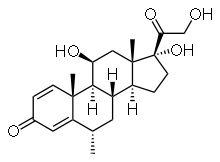
Devic's disease is similar to MS in that the body's immune system attacks the myelin surrounding nerve cells. Unlike standard MS, the attacks are not believed to be mediated by the immune system's T cells, but rather by antibodies called NMO-IgG, or simply NMO antibodies. These antibodies target the protein aquaporin 4 in the cell membranes of astrocytes which acts as a channel for the transport of water across the cell membrane.[3] Aquaporin 4 is found in the processes of the astrocytes that surround the blood–brain barrier, a system responsible for preventing substances in the blood from crossing into the brain. The blood–brain barrier is weakened in Devic's disease, but it is currently unknown how the NMO-IgG immune response leads to demyelination.
Most research into the pathology of Devic's disease has focused on the spinal cord. The damage can range from inflammatory demyelination to necrotic damage of the white and grey matters. The inflammatory lesions in Devic's disease have been classified as type II lesions (complement-mediated demyelinization), but they differ from MS pattern II lesions in their prominent perivascular distribution. Therefore, the pattern of inflammation is often quite distinct from that seen in MS.[3][7]
Diagnosis
The Mayo Clinic proposed a revised set of criteria for diagnosis of Devic's disease in 2006. The new guidelines require two absolute criteria plus at least two of three supportive criteria.[8]
Absolute criteria:
- Optic neuritis
- Acute myelitis
Supportive criteria:
- Brain MRI not meeting criteria for MS at disease onset
- Spinal cord MRI with contiguous T2-weighted signal abnormality extending over three or more vertebral segments, indicating a relatively large lesion in the spinal cord
- NMO-IgG seropositive status (The NMO-IgG test checks the existence of antibodies against the aquaporin 4 antigen.)
Variants
After the development of the NMO-IgG test, the spectrum of disorders comprising Devic's disease was expanded. The spectrum is now believed to consist of:
- Standard Devic's disease, according to the diagnostic criteria described above
- Limited forms of Devic's disease, such as single or recurrent events of longitudinally extensive myelitis, and bilateral simultaneous or recurrent optic neuritis
- Asian optic-spinal MS - this variant can present CNS involvement like MS.[9]
- Longitudinally extensive myelitis or optic neuritis associated with systemic autoimmune disease
- Optic neuritis or myelitis associated with lesions in specific brain areas such as the hypothalamus, periventricular nucleus, and brainstem[10]
- NMO-IgG negative NMO: AQP4 antibody-seronegative NMO poses a diagnostic challenge.[11][12]
Whether Devic's disease is a distinct disease or part of the wide spectrum of multiple sclerosis is debated.[13] Devic's disease differs in that it usually has more severe sequelae after an acute episode than standard MS, MS infrequently presents as transverse myelitis, and oligoclonal bands in the CSF, as well as white matter lesions on brain MRI, are uncommon in Devic's disease, but occur in over 90% of MS patients.[14]
Recently, AQP4 has been found to distinguish standard multiple sclerosis from neuromyelitis optica, but as MS is a heterogeneous condition,[15] and some MS cases are reported to be Kir4.1 channelopathies[16] (autoimmunity against the potasium channels) it is still possible to consider NMO as part of the MS spectrum.
Causes
Devic's disease has been associated with many systemic diseases, based on anecdoctal evidence of some Devic's disease patients with a comorbid condition. Such conditions include: collagen vascular diseases, autoantibody syndromes, infections with varicella-zoster virus, Epstein-Barr virus, and HIV, and exposure to clioquinol and antituberculosis drugs.[17]
The discovery of NMO-IgG has opened a new way into the research for the causes, but it is still unknown how the antibodies against AQP4 appear.
Treatment
Currently, there is no cure for Devic's disease, but symptoms can be treated. Some patients recover, but many are left with impairment of vision and limbs, which can be severe.
Attacks
Attacks are treated with short courses of high dosage intravenous corticosteroids such as methylprednisolone IV.
Plasmapheresis can be an effective treatment.[10] when attacks progress or do not respond to corticosteroid treatment, Clinical trials for these treatments contain very small numbers, and most are uncontrolled, though some report high success percentage[18]
Secondary prevention
No controlled trials have established the effectiveness of treatments for the prevention of attacks. Many clinicians agree that long term immunosuppression is required to reduce the frequency and severity of attacks, while others argue the exact opposite.[19] Commonly used immunosuppressant treatments include azathioprine (Imuran) plus prednisone, mycophenolate mofetil plus prednisone, rituximab, mitoxantrone, intravenous immunoglobulin (IVIG), and cyclophosphamide.[10][20] The monoclonal antibody rituximab is under study.[21] In 2007, Devic's disease was reported to be responsive to glatiramer acetate[22] and to low-dose corticosteroids.[23]
Prognosis
Normally, some measure of improvement appears in a few weeks, but residual signs and disability may persist, sometimes severely.
The disease can be monophasic, i.e. a single episode with permanent remission. However, at least 85% of patients have a relapsing form of the disease with repeated attacks of transverse myelitis and/or optic neuritis. In patients with the monophasic form, the transverse myelitis and optic neuritis occur simultaneously or within days of each other. On the other hand, patients with the relapsing form are more likely to have weeks or months between the initial attacks, and to have better motor recovery after the initial transverse myelitis event. Relapses usually occur early, with about 55% of patients having a relapse in the first year and 90% in the first five years.[3] Unlike multiple sclerosis, Devic's disease rarely has a secondary progressive phase in which patients have increasing neurologic decline between attacks without remission. Instead, disabilities arise from the acute attacks.[3]
Approximately 20% of patients with monophasic Devic's disease have permanent visual loss, and 30% have permanent paralysis in one or both legs. Among patients with relapsing Devic's disease, 50% have paralysis or blindness within five years. In some patients (33% in one study), transverse myelitis in the cervical spinal cord resulted in respiratory failure and subsequent death. However, the spectrum of Devic's disease has widened due to improved diagnostic criteria, and the options for treatment have improved; as a result, researchers believe these estimates will be lowered.[3]
Epidemiology
The prevalence and incidence of Devic's disease has not been established, partly because the disease is underrecognized and often confused with MS.[3] Devic's disease is more common in women than men, with women comprising over two-thirds of patients and more than 80% of those with the relapsing form of the disease.[3]
According to the Walton Centre in England, "NMO seems to be present across the world unlike MS, which has a higher incidence in temperate climates and white races. Africans and Asians especially in Far East may have a higher risk of NMO, although the exact incidence of this disease is unknown, making specific conclusions difficult". Although many people who have Devic's disease were initially misdiagnosed with MS, 35% of African Americans are often misdiagnosed with MS when they really have NMO.
Devic's disease is more common in Asiana than Caucasians. In fact, Asian optic-spinal MS (which constitutes 30% of the cases of MS in Japan) has been suggested to be identical to Devic's disease (differences between optic-spinal and classic MS in Japanese patients). In the indigenous populations of tropical and subtropical regions, MS is rare, but when it appears, it often takes the form of optic-spinal MS.[24]
The majority of Devic's disease patients have no affected relatives, and it is generally regarded as a nonfamilial condition.[3]
Neuromyelitis optica spectrum disorders
Since the discovery of AQP4 autoantibody, it has been found that it appears also in patients with NMO-like symptoms that do not fullfil the requirements to be diagnosed NMO (Recurrent and simultaneous optic nerve and spinal cord inflammation).[25]
The collection of these condition has been named "Neuromyelitis optica spectrum disorders" (NMSD) and they are expected to respond to the same treatments than standard NMO.[26]
History

In 1870, Sir Thomas Clifford Allbutt first reported an association between myelitis and an optic nerve disorder. In 1894, Eugène Devic and his PhD student Fernand Gault described 16 patients who had lost vision in one or both eyes and within weeks developed severe spastic weakness of the limbs, loss of sensation and often bladder control. They recognized these symptoms were the result of inflammation of the optic nerve and spinal cord, respectively.[27][28]
Similar instances of optic neuritis and myelitis were reported, and many believed it constituted a distinct clinical entity. However, some patients had pathology in other parts of the brain, a feature which was more suggestive of acute disseminated encephalomyelitis or MS.
In 2004, Mayo Clinic researchers identified the aquaporin 4 protein as the target of the disease and developed a test to aid in the diagnosis of Devic's disease by detection of an antibody, NMO-IgG, in the blood.[5] Some patients with NMO may be seronegative for NMO-IgG, whilst some patients with NMO-IgG may still not fulfill clinical criteria for NMO thus serological testing is now an important part of the diagnostic procedure and seropositive and seronegative cases are described in a manner similar to myasthenia gravis. According to the Mayo Clinic report, this was the first time a molecular target had been identified for a type of demyelinating inflammatory disease.[29]
Research directions
Since the discovery of AQP-4 involvement, some research studies have focused on targeted treatment aimed at anti-aquaporin 4 antibodies. The most established method for antibody removal is plasmapheresis. A number of drugs is being studied: aquaporumab (non-pathogenic antibody blocker of AQP4-IgG binding), sivelestat (neutrophil elastase inhibitor), and eculizumab (complement inhibitor).[30]
See also
- Idiopathic inflammatory demyelinating diseases
References
- ↑ Pittock SJ, Weinshenker BG, Lucchinetti CF, Wingerchuk DM, Corboy JR, Lennon VA (2006). "Neuromyelitis optica brain lesions localized at sites of high aquaporin 4 expression". Arch. Neurol. 63 (7): 964–968. doi:10.1001/archneur.63.7.964. PMID 16831965.
- ↑ "neuromyelitis optica" at Dorland's Medical Dictionary
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Wingerchuk, DM (2006). "Neuromyelitis optica". The International MS Journal 13 (2): 42–50. PMID 16635421.
- ↑ Lennon VA, Wingerchuk DM, Kryzer TJ, et al. (2004). "A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis". Lancet 364 (9451): 2106–2112. doi:10.1016/S0140-6736(04)17551-X. PMID 15589308.
- ↑ 5.0 5.1 Lennon VA, Kryzer TJ, Pittock SJ, Verkman AS, Hinson SR (2005). "IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel". J. Exp. Med. 202 (4): 473–477. doi:10.1084/jem.20050304. PMC 2212860. PMID 16087714.
- ↑ Mayo Clinic. "Devic's Disease Symptoms". Archived from the original on 2008-01-02. Retrieved 2008-03-11.
- ↑ Lucchinetti CF, Mandler RN, McGavern D, et al. (2002). "A role for humoral mechanisms in the pathogenesis of Devic's neuromyelitis optica". Brain 125 (Pt 7): 1450–1461. doi:10.1093/brain/awf151. PMID 12076996.
- ↑ Wingerchuk DM, Lennon VA, Pittock SJ, Lucchinetti CF, Weinshenker BG (2006). "Revised diagnostic criteria for neuromyelitis optica". Neurology 66 (10): 1485–1489. doi:10.1212/01.wnl.0000216139.44259.74. PMID 16717206.
- ↑ Li Y, Xie P, Lv F, et al. (2008). "Brain magnetic resonance imaging abnormalities in neuromyelitis optica". Acta Neurol. Scand. 0 (4): 218–25. doi:10.1111/j.1600-0404.2008.01012.x. PMID 18384459.
- ↑ 10.0 10.1 10.2 Wingerchuk, Dean (2006). "Neuromyelitis Optica (Devic's Syndrome)" (PDF). 2006 Rare Neuroimmunologic Disorders Symposium. Retrieved 2007-01-05.
- ↑ Fujihara K, Leite MI. Seronegative NMO: A sensitive AQP4 antibody test clarifies clinical features and next challenges, Neurology. 2013 May 8
- ↑ Marignier R, Bernard-Valnet R, Giraudon P, Collongues N, Papeix C, Zéphir H, Cavillon G, Rogemond V, Casey R, Frangoulis B, De Sèze J, Vukusic S, Honnorat J, Confavreux C; For the NOMADMUS Study Group. Aquaporin-4 antibody-negative neuromyelitis optica: Distinct assay sensitivity-dependent entity, Neurology. 2013 May 8
- ↑ Pearce JM (2008). "Overview of MS: proposal of new MS definition/classification and review of the results of recent clinical trials". Nippon Rinsho (abstract) 66 (6): 1081–6. PMID 18540351.
- ↑ Pearce JM (2005). "Neuromyelitis optica" (abstract). Spinal Cord 43 (11): 631–634. doi:10.1038/sj.sc.3101758. PMID 15968305.
- ↑ Lassmann, H; Brück, W; Lucchinetti, C (2001). "Heterogeneity of multiple sclerosis pathogenesis: Implications for diagnosis and therapy". Trends in molecular medicine 7 (3): 115–21. PMID 11286782.
- ↑ Schneider, R (2013). "Autoantibodies to Potassium Channel KIR4.1 in Multiple Sclerosis". Frontiers in neurology 4: 125. doi:10.3389/fneur.2013.00125. PMC 3759297. PMID 24032025.
- ↑ Cree BA, Goodin DS, Hauser SL (2002). "Neuromyelitis optica". Seminars in neurology 22 (2): 105–122. doi:10.1055/s-2002-36534. PMID 12524556.
- ↑ Morgan SM, Zantek ND, Carpenter AF. Therapeutic plasma exchange in neuromyelitis optica: A case series. J Clin Apher. 2013 Oct 17. doi: 10.1002/jca.21304
- ↑ Poser CM, Brinar VV (2007). "Disseminated encephalomyelitis and multiple sclerosis: two different diseases – a critical review". Acta Neurol. Scand. 116 (4): 201–206. doi:10.1111/j.1600-0404.2007.00902.x. PMID 17824894.
- ↑ Weinstock-Guttman B, Ramanathan M, Lincoff N, et al. (2006). "Study of mitoxantrone for the treatment of recurrent neuromyelitis optica (Devic disease)". Arch. Neurol. 63 (7): 957–963. doi:10.1001/archneur.63.7.957. PMID 16831964.
- ↑ Matiello M, Jacob A, Wingerchuk DM, Weinshenker BG (2007). "Neuromyelitis optica". Current Opinion in Neurology 20 (3): 255–260. doi:10.1097/WCO.0b013e32814f1c6b. PMID 17495617.
- ↑ Gartzen K, Limmroth V, Putzki N (2007). "Relapsing neuromyelitis optica responsive to glatiramer acetate treatment". Eur. J. Neurol. 14 (6): e12–3. doi:10.1111/j.1468-1331.2007.01807.x. PMID 17539924.
- ↑ Watanabe S, Misu T, Miyazawa I, et al. (2007). "Low-dose corticosteroids reduce relapses in neuromyelitis optica: a retrospective analysis". Multiple Sclerosis 13 (8): 968–74. doi:10.1177/1352458507077189. PMID 17623727.
- ↑ Cabre P, Signate A, Olindo S, et al. (2005). "Role of return migration in the emergence of multiple sclerosis in the French West Indies". Brain 128 (Pt 12): 2899–2910. doi:10.1093/brain/awh624. PMID 16183661.
- ↑ Masaki K, Suzuki SO, Matsushita T, Matsuoka T, Imamura S, Yamasaki R, Suzuki M, Suenaga T, Iwaki T, Kira J., Connexin 43 astrocytopathy linked to rapidly progressive multiple sclerosis and neuromyelitis optica, PMID 23991165
- ↑ Fujihara K, Sato DK., AQP4 antibody serostatus: Is its luster being lost in the management and pathogenesis of NMO?, PMID 23997154
- ↑ Devic E (1894). "Myélite subaiguë compliquée de névrite optique". Bull Med (in French) 8: 1033.
- ↑ T. Jock Murray (2005). Multiple Sclerosis: The History of a Disease. New York: Demos Medical Publishing. ISBN 1-888799-80-3.
- ↑ "Devic's Disease Research – Mayo Clinic". Retrieved 2007-11-22.
- ↑ Papadopoulos MC, Verkman AS (June 2012). "Aquaporin 4 and neuromyelitis optica". Lancet Neurol 11 (6): 535–44. doi:10.1016/S1474-4422(12)70133-3. PMC 3678971. PMID 22608667.
External links
- Devic's Disease (Neuromyelitis Optica) at myelitis.org
- Devics Disease – Information and treatment options at Mayo Clinic
- The Guthy-Jackson Charitable Foundation – for NMO Research
- The SistaMoon Foundation For Devic's Disease Information on Research as it relates to Devic's/NMO and Resources
- Specialist NMO information from the UK NHS NMO diagnostic and advisory service
| |||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||