Kleihauer–Betke test

The Kleihauer–Betke ("KB") test, Kleihauer–Betke ("KB") stain or Kleihauer test, is a blood test used to measure the amount of fetal hemoglobin transferred from a fetus to a mother's bloodstream.[1] It is usually performed on Rhesus-negative mothers to determine the required dose of Rho(D) immune globulin (RhIg) to inhibit formation of Rh antibodies in the mother and prevent Rh disease in future Rh-positive children.[2]
Test details
The KB test is the standard method of quantitating fetal-maternal hemorrhage (FMH). It takes advantage of the differential resistance of fetal hemoglobin to acid. A standard blood smear is prepared from the mother's blood, and exposed to an acid bath. This removes adult hemoglobin, but not fetal hemoglobin, from the red blood cells. Subsequent staining, using Shepard's method,[3] makes fetal cells (containing fetal hemoglobin) appear rose-pink in color, while adult red blood cells are only seen as "ghosts". 2000 cells are counted under the microscope and a percentage of fetal to maternal cells is calculated.
In those with positive tests, follow up testing at a postpartum check should be done to rule out the possibility of a false positive. This could be caused by a process in the mother which causes persistent elevation of fetal hemoglobin, e.g. sickle cell trait.
Comparison with other more expensive or technologically advanced methods such as flow cytometry has shown that the KB stain, like the more advanced methods, is sensitive in its detection of FMH.[1] Background counting errors can result in estimates of as much as 5 ml fetal blood loss when there actually is no such blood loss, but standard methods available in most laboratories admit an extremely low probability of the return of a false positive when more severe FMH has taken place.
Uses
Fetal–maternal hemorrhage severity estimation
To determine if a positive test for FMH should be considered as the likely cause of fetal death, the percent of total fetal blood volume lost should be calculated, making appropriate adjustments based on the following known relationships:
- the size of a fetal red blood cell is 1.22 times that of an adult red blood cell;
- the KB stain is known to have a mean success rate of 92% in detecting fetal red blood cells;
- in a woman at or near term in her pregnancy, the mean volume of maternal red blood cells is approximately 1800 ml;
- the mean fetal hematocrit is 50%; and
- at stillbirth, the mean fetal blood volume is

These constraints can then be applied to yield the formula
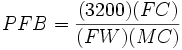
where
-
 is the percentage of fetal blood lost;
is the percentage of fetal blood lost; -
 is the observed number of fetal red blood cells;
is the observed number of fetal red blood cells; -
 is the observed number of maternal red blood cells (N.B. we have that
is the observed number of maternal red blood cells (N.B. we have that 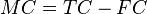 , where
, where  is the total observed number of red blood cells, both maternal and fetal);
is the total observed number of red blood cells, both maternal and fetal); -
 is the stillbirth weight of the fetus in kilograms.
is the stillbirth weight of the fetus in kilograms.
-
Stillbirth resolution
Suppose that a KB stain is performed and  total red blood cells are observed,
total red blood cells are observed,  of which are found to be fetal red blood cells. Suppose further that the stillbirth weight of the fetus under consideration is
of which are found to be fetal red blood cells. Suppose further that the stillbirth weight of the fetus under consideration is 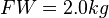 . Then we would conclude that the total percentage of fetal blood lost is approximately
. Then we would conclude that the total percentage of fetal blood lost is approximately
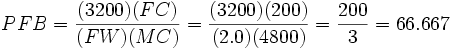
to five significant digits. We would hence conclude that the fetus under consideration lost 66.667% (two-thirds) of its blood via FMH. Generally, stillbirth is highly probable for any value of  , particularly if the fetus abruptly loses this much blood; in this example, we would hence be likely to suspect FMH as the cause of the stillbirth. It is important to note, however, that such a diagnosis is still not completely conclusive; fetuses losing large quantities of blood over long periods of time are able to compensate for this slower blood loss; since the KB stain tells us nothing with regard to the level of acuity of FMH. This means that it is not possible to entirely correlate a positive KB stain and high
, particularly if the fetus abruptly loses this much blood; in this example, we would hence be likely to suspect FMH as the cause of the stillbirth. It is important to note, however, that such a diagnosis is still not completely conclusive; fetuses losing large quantities of blood over long periods of time are able to compensate for this slower blood loss; since the KB stain tells us nothing with regard to the level of acuity of FMH. This means that it is not possible to entirely correlate a positive KB stain and high  with a stillbirth, though in many cases, given other information, such as known hereditary complications of pregnancy, extremely high positive correlation coefficients
with a stillbirth, though in many cases, given other information, such as known hereditary complications of pregnancy, extremely high positive correlation coefficients  between FMH and stillbirth have been observed.
between FMH and stillbirth have been observed.
Fetal red-blood-cell detection problems
Since fetal and maternal blood cells have the same life expectancy in the maternal bloodstream, it is possible to obtain informative results from a KB stain for a fair period of time after a stillbirth. However, if the mother and fetus are ABO incompatible, it is more crucial to quickly perform the KB stain following a stillbirth, as the fetal red blood cells will be eliminated from the maternal bloodstream very quickly, causing the KB stain to underestimate the degree of FMH, if any.
Lots of concern has been raised in the literature concerning false positives when sampling is done after delivery. In general this is not a problem. Delivery does result in higher frequency of detection of micro-hemorrhages but this should not confound interpretation of FMH as a possible cause of stillbirth. It is not necessary to draw the sample before induction, onset of labor, delivery, placental delivery etc. despite what some published literature purports. However, if caesarean section is to be used, failure to draw the sample prior to that will result in a 2% false positive rate.
Finally, anything which causes persistence of fetal hemoglobin in maternal blood cells will make interpretation much trickier. Certain hemoglobinopathies, the most common of which is sickle cell trait, do this. Overall, somewhere around 1–3% of the time this could result in false interpretation.
See also
External links
King Edward Memorial Hospital,Perth Western Australia
References
- ↑ 1.0 1.1 Katiyar R, Kriplani A, Agarwal N, Bhatla N, Kabra M (2007). "Detection of fetomaternal hemorrhage following chorionic villus sampling by Kleihauer–Betke test and rise in maternal serum alpha feto protein". Prenat. Diagn. 27 (2): 139–42. doi:10.1002/pd.1632. PMID 17191260.
- ↑ Kim YA, Makar RS (April 2012). "Detection of fetomaternal hemorrhage". American Journal of Hematology 87 (4): 417–23. doi:10.1002/ajh.22255. PMID 22231030.
- ↑ Alcoholic haematoxylin, acidified ferric chloride, Shepard's counterstain. Shepard's Fixative/Diluent
| |||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||||