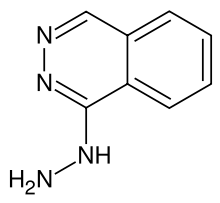
Hydralazine
 | |
|---|---|
| Systematic (IUPAC) name | |
| 1-hydrazinylphthalazine | |
| Clinical data | |
| AHFS/Drugs.com | monograph |
| MedlinePlus | a682246 |
| Pregnancy cat. | C Commonly used to treat severe PIH |
| Legal status | ? |
| Routes | Oral, intravenous |
| Pharmacokinetic data | |
| Bioavailability | 26-55% |
| Metabolism | Hepatic |
| Half-life | 2-4 hours |
| Excretion | Renal |
| Identifiers | |
| CAS number | 86-54-4 |
| ATC code | C02DB02 |
| PubChem | CID 3637 |
| DrugBank | DB01275 |
| ChemSpider | 3511 |
| UNII | 26NAK24LS8 |
| KEGG | D08044 |
| ChEBI | CHEBI:5775 |
| ChEMBL | CHEMBL276832 |
| Chemical data | |
| Formula | C8H8N4 |
| Mol. mass | 160.176 g/mol |
| SMILES
| |
| |
| | |
Hydralazine (apresoline) is a direct-acting smooth muscle relaxant used to treat hypertension by acting as a vasodilator primarily in arteries and arterioles. By relaxing vascular smooth muscle, vasodilators act to decrease peripheral resistance, thereby lowering blood pressure and decreasing afterload.[1]
However, this only has a short term effect on blood pressure, as the system will reset to the previous, high blood pressure necessary to maintain pressure in the kidney necessary for natriuresis. The long term effect of antihypertensive drugs comes from their effects on the pressure natriuresis curve.
It belongs to the hydrazinophthalazine class of drugs.[2]
Mechanism of action
Hydralazine binds to and activates gated potassium channels on vascular smooth muscle. The result is an efflux of potassium and a subsequent hyperpolarization of the cell. This prevents calcium-mediated activation and constriction of the smooth muscle, resulting in vasodilation. However, this induced vasodilation triggers the baroreflex resulting in tachycardia and vasoconstriction. Hydralazine is therefore not a great candidate for control of hypertension alone. It is often co-administered with a beta blocker to mitigate the effects of the baroreflex.
Hydralazine requires the endothelium to provide NO (nitric oxide.[3] ) thus only provides the effects of NO in vivo with functional endothelium. It will not work to vasodilate in vitro in an isolated blood vessel.
Activation of hypoxia-inducible factors has been suggested as a mechanism.[4]
Clinical use
Hydralazine is not used as a primary drug for treating hypertension because it elicits a reflex sympathetic stimulation of the heart (the baroreceptor reflex). The sympathetic stimulation may increase heart rate and cardiac output, and in patients with coronary artery disease may cause angina pectoris or myocardial infarction.[1] Hydralazine may also increase plasma renin concentration, resulting in fluid retention. In order to prevent these undesirable side-effects, hydralazine is usually prescribed in combination with a beta-blocker (e.g., propranolol) and a diuretic.[1] In the UK, labetalol tends to be the first line beta-blocker.
Hydralazine is used to treat severe hypertension, but again, it is not a first-line therapy for essential hypertension. However, hydralazine is the first-line therapy for hypertension in pregnancy, with methyldopa.[5]
Pre-clinical research
Multiple sclerosis: Due to its ability to damage myelin nerve sheaths, acrolein may be a factor in the development of multiple sclerosis. Hydralazine, a known scavenger of acrolein, was found to reduce myelin damage and significantly improve behavioral outcomes in a mouse model of multiple sclerosis (experimental autoimmune encephalomyelitis).[6]
Side effects
Common side-effects include:
- Diarrhea
- Compensatory tachycardia due to baroreceptor reflex ->Angina
- Headache
- Loss of appetite
- Nausea or vomiting
- Depression
- Pounding heartbeat
- Vitamin B6 deficiency [7]
- Drug-Induced Lupus Erythematosus[8][9]
- ANCA-associated Vasculitis - Generally MPO-ANCA positive
Patients given hydralazine over a period of six months may develop a lupus-like syndrome or other immune-related diseases that, in general, are reversible with withdrawal.[1] Hydralazine is differentially acetylated by fast and slow acetylator phenotypes, hence incidence of lupus-like disease in slow acetylators.[citation needed] Rarely, hydralazine may cause Dyscrasia typically manifested as a type of leukopenia. As such, your physician may request you undergo regular Complete blood count tests.[10]
See also
References
- ↑ 1.0 1.1 1.2 1.3 Harvey, Richard A., Pamela A. Harvey, and Mark J. Mycek. Lippincott's Illustrated Reviews: Pharmacology. 2nd ed. Philadelphia: Lipincott, Williams & Wilkins, 2000. 190.
- ↑ Bourreli, B.; Pinaud, M.; Passuti, N.; Gunst, J. P.; Drouet, J. C.; Remi, J. P. (1988). "Additive effects of dihydralazine during enflurane or isoflurane hypotensive anaesthesia for spinal fusion". Canadian Journal of Anaesthesia 35 (3): 242–248. doi:10.1007/BF03010617. PMID 3383316.
- ↑ "antihtn". Retrieved 2008-10-05.
- ↑ Knowles HJ, Tian YM, Mole DR, Harris AL (July 2004). "Novel mechanism of action for hydralazine: induction of hypoxia-inducible factor-1alpha, vascular endothelial growth factor, and angiogenesis by inhibition of prolyl hydroxylases". Circ. Res. 95 (2): 162–9. doi:10.1161/01.RES.0000134924.89412.70. PMID 15192023.
- ↑ Bhushan, Vikas, Tao T. Lee, and Ali Ozturk. First Aid for the USMLE Step 1. New York: McGraw-Hill Medical, 2007. 251.
- ↑ Leung, G; Sun W, Zheng L, Brookes S, Tully M, Shi R (2010). "Anti-acrolein treatment improves behavioral outcome and alleviates myelin damage in EAE mouse". Neuroscience 173: 150–5. doi:10.1016/j.neuroscience.2010.11.018. PMC 3034379. PMID 21081153.
- ↑ Sanders, Lisa (2010-06-06). "DIAGNOSIS; Dizzying Symptoms". The New York Times.
- ↑ Schoonen WM,et al. Do selected drugs increase the risk of lupus? A matched case-control study. Br J Clin Pharmacol. 2010 Oct;70(4):588-96. doi:10.1111/j.1365-2125.2010.03733.x.
- ↑ Mazari L, Ouarzane M, Zouali M (April 2007). "Subversion of B lymphocyte tolerance by hydralazine, a potential mechanism for drug-induced lupus". Proc. Natl. Acad. Sci. U.S.A. 104 (15): 6317–22. doi:10.1073/pnas.0610434104. PMC 1851062. PMID 17404230.
- ↑ "Hydralazine Hydrochloride". DailyMed. U.S. National Library of Medicine.
| |||||||||||||||||||||||||