Cyclophosphamide
 | |
|---|---|
 | |
| Systematic (IUPAC) name | |
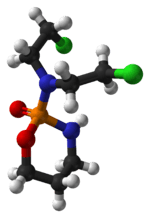
| (RS)-N,N-bis(2-chloroethyl)-1,3,2-oxazaphosphinan-2-amine 2-oxide | |
| Clinical data | |
| Trade names | Lyophilizedcytoxan |
| AHFS/Drugs.com | monograph |
| MedlinePlus | a682080 |
| Pregnancy cat. | D (AU) D (US) |
| Legal status | ℞ Prescription only |
| Routes | Oral, intravenous |
| Pharmacokinetic data | |
| Bioavailability | >75% (oral) |
| Protein binding | >60% |
| Metabolism | Hepatic |
| Half-life | 3-12 hours |
| Excretion | Renal |
| Identifiers | |
| CAS number | 50-18-0 |
| ATC code | L01AA01 |
| DrugBank | DB00531 |
| ChemSpider | 2804 |
| UNII | 6UXW23996M |
| KEGG | D07760 |
| ChEBI | CHEBI:4027 |
| ChEMBL | CHEMBL88 |
| Chemical data | |
| Formula | C7H15Cl2N2O2P |
| Mol. mass | 261.086 g/mol |
| SMILES
| |
| |
| Physical data | |
| Melt. point | 2 °C (36 °F) |
| | |
Cyclophosphamide (INN, trade names Endoxan, Cytoxan, Neosar, Procytox, Revimmune), also known as cytophosphane,[1] is a nitrogen mustard alkylating agent,[2] from the oxazaphosphinans group.
An alkylating agent adds an alkyl group (CnH2n+1) to DNA. It attaches the alkyl group to the guanine base of DNA, at the number 7 nitrogen atom of the imidazole ring. This interferes with DNA replication by forming intrastrand and interstrand DNA crosslinks.
It is used to treat cancers and autoimmune disorders. As a prodrug, it is converted in the liver to active forms that have chemotherapeutic activity.
Cyclophosphamide has severe and life-threatening adverse effects, including acute myeloid leukemia, bladder cancer, hemorrhagic cystitis, and permanent infertility, especially at higher doses. For autoimmune diseases, doctors often substitute less-toxic methotrexate or azathioprine after an acute crisis.[3]
The main hepatic active metabolite of cyclophosphamide, 4-hydroperoxycyclophosphamide, has its own use in medicine. It is often used for extracorporal cell treatment. For example, it is used to "purge" the collected donor bone marrow or hematopoietic stem cells off of the lymphocytes while preserving myeloid predecessors (CD34 positive cells). It is also used to "purge" patient's own (autologous) stem cells off of any malignant cells that may be still present in it at the time of harvesting.
Uses
Cyclophosphamide is used to treat cancer and immune diseases.
Cancer

The main use of cyclophosphamide is with other chemotherapy agents in the treatment of lymphomas, some forms of brain cancer, leukemia[4] and some solid tumors.[5] It is a chemotherapy drug that works by inducing the death of certain T cells.
A 2004 study[6] showed the biological actions of cyclophosphamide are dose-dependent. At higher doses, it is associated with increased cytotoxicity and immunosuppression, while at low, continuous doses, it shows immunostimulatory and antiangiogenic properties. A 2009 study of 17 patients with docetaxel-resistant metastatic hormone refractory prostate cancer showed a prostate-specific antigen (PSA) decrease in 9 of the 17 patients. Median survival was 24 months for the entire group, and 60 months for those with a PSA response. The study concluded low-dose cyclophosphamide "might be a viable alternative" treatment for docetaxel-resistant MHRPC and "is an interesting candidate for combination therapies, e.g., immunotherapy, tyrosine kinase inhibitors, and antiangiogenisis."[7]
Autoimmune diseases
Cyclophosphamide also decreases the immune system's response to various diseases and conditions. Therefore, it has been used in autoimmune diseases where disease-modifying antirheumatic drugs (DMARDs) have been ineffective. For example, systemic lupus erythematosus with severe lupus nephritis[8] may respond to pulsed cyclophosphamide. Cyclophosphamide is also used to treat minimal change disease,[9] severe rheumatoid arthritis,[10] Wegener's granulomatosis[11] (with trade name Cytoxan), and multiple sclerosis[12] (with trade name Revimmune).
Pharmacokinetics/pharmacodynamics
Cyclophosphamide is converted by mixed-function oxidase enzymes (cytochrome P450 system) in the liver to active metabolites.[13] The main active metabolite is 4-hydroperoxycyclophosphamide, which exists in equilibrium with its tautomer, aldophosphamide. Most of the aldophosphamide is then oxidised by the enzyme aldehyde dehydrogenase (ALDH) to make carboxyphosphamide. A small proportion of aldophosphamide freely diffuses into cells, it is decomposed into two compounds, phosphoramide mustard and acrolein.[14] Acrolein is toxic to the bladder epithelium and can lead to hemorrhagic cystitis.[15] This can be prevented through the use of aggressive hydration and/or mesna.
Cyclophosphamide induces beneficial immunomodulatory effects in adaptive immunotherapy. Suggested mechanisms include:[citation needed]
- Elimination of T regulatory cells (CD4+CD25+ T cells) in naive and tumor-bearing hosts
- Induction of T cell growth factors, such as type I IFNs, and/or
- Enhanced grafting of adoptively transferred, tumor-reactive effector T cells by the creation of an immunologic space niche.
Thus, cyclophosphamide preconditioning of recipient hosts (for donor T cells) has been used to enhance immunity in naïve hosts, and to enhance adoptive T cell immunotherapy regimens, as well as active vaccination strategies, inducing objective antitumor immunity.
Mechanism of action
The main effect of cyclophosphamide is due to its metabolite phosphoramide mustard. This metabolite is only formed in cells that have low levels of ALDH.
Phosphoramide mustard forms DNA crosslinks both between and within DNA strands at guanine N-7 positions (known as interstrand and intrastrand crosslinkages, respectively). This is irreversible and leads to cell apoptosis.
Cyclophosphamide has relatively little typical chemotherapy toxicity as ALDHs are present in relatively large concentrations in bone marrow stem cells, liver and intestinal epithelium. ALDHs protect these actively proliferating tissues against toxic effects of phosphoramide mustard and acrolein by converting aldophosphamide to carboxyphosphamide that does not give rise to the toxic metabolites phosphoramide mustard and acrolein.
Side effects
Adverse drug reactions include chemotherapy-induced nausea and vomiting, bone marrow suppression, stomach ache, hemorrhagic cystitis, diarrhea, darkening of the skin/nails, alopecia (hair loss) or thinning of hair, changes in color and texture of the hair, and lethargy. Hemorrhagic cystitis is a frequent complication, but this is prevented by adequate fluid intake and mesna (sodium 2-mercaptoethane sulfonate), a sulfhydryl donor which binds acrolein.
Cyclophosphamide is itself carcinogenic, potentially causing transitional cell carcinoma of the bladder as a long-term complication. It can lower the body's ability to fight an infection. It can cause temporary or (rarely) permanent sterility. A serious potential side effect is acute myeloid leukemia, referred to as secondary AML (therapy-related AML, or "t-AML"), thought to occur either by cyclophosphamide inducing mutations or selecting for a high-risk myeloid clone.[16] The risk may be dependent on dose and a number of other factors, including the condition being treated, other agents or treatment modalities used (including radiotherapy), treatment intensity and length of treatment. For some regimens, it is a very rare occurrence. For instance, CMF-therapy for breast cancer (where the cumulative dose is typically less than 20 grams of cyclophosphamide) seems to carry an AML risk of less than 1/2000th, with some studies even finding no increased risk compared to the background population. Other treatment regimens involving higher doses may carry risks of 1-2% or higher, depending on regimen. Cyclophosphamide-induced AML, when it happens, typically presents some years after treatment, with incidence peaking around 3–9 years. After nine years, the risk has fallen to the level of the regular population. When AML occurs, it is often preceded by a myelodysplastic syndrome phase, before developing into overt acute leukemia. Cyclophosphamide-induced leukemia will often involve complex cytogenetics, which carries a worse prognosis than de novo AML.
Other side effects include:
- easy bruising/bleeding
- gross and microscopic hematuria
- joint pain
- mouth sores
- slow-healing existing wounds
- syndrome of inappropriate antidiuretic hormone (SIADH)
- unusual decrease in the amount of urine
- unusual tiredness or weakness
History
As reported by O.M. Colvin in his study of the development of cyclophosphomide and its clinical applications,
Phosphoramide mustard, one of the principle toxic metabolites of cyclophosphamide, was synthesized and reported by Friedman and Seligman in 1954[17] ...It was postulated that the presence of the phosphate bond to the nitrogen atom could inactivate the nitrogen mustard moiety, but the phosphate bond would be cleaved in gastric cancers and other tumors which had a high phosphamidase content. However, in studies carried out after the clinical efficacy of cyclophosphamide was demonstrated, phosphoramide mustard proved to be cytotoxic in vitro (footnote omitted), but to have a low therapeutic index in vivo.[18]
Cyclophosphamide and the related nitrogen mustard-derived alkylating agent ifosfamide were developed by Norbert Brock and ASTA (now Baxter Oncology). Brock and his team synthesised and screened more than 1,000 candidate oxazaphosphorine compounds.[19] They converted the base nitrogen mustard into a nontoxic "transport form". This transport form was a prodrug, subsequently actively transported into the cancer cells. Once in the cells, the prodrug was enzymatically converted into the active, toxic form. The first clinical trials were published at the end of the 1950s.[20][21][22] In 1959 it became the eighth cytotoxic anticancer agent to be approved by the FDA.[15]
References
- ↑ National Cancer Dictionary: cyclophosphamide
- ↑ Takimoto CH, Calvo E. "Principles of Oncologic Pharmacotherapy" in Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ (Eds) Cancer Management: A Multidisciplinary Approach. 11 ed. 2008.
- ↑ Kasper, Dennis L; Braunwald, Eugene; Fauci, Anthony; et al. (2005). Harrison's Principles of Internal Medicine, 16th ed. New York: McGraw-Hill. p. 2066. ISBN 978-0-07-139140-5.
- ↑ Shanafelt TD, Lin T, Geyer SM, et al. (June 2007). "Pentostatin, cyclophosphamide, and rituximab regimen in older patients with chronic lymphocytic leukemia". Cancer 109 (11): 2291–8. doi:10.1002/cncr.22662. PMID 17514743.
- ↑ Young SD, Whissell M, Noble JC, et al. (2006). "Phase II clinical trial results involving treatment with low-dose daily oral cyclophosphamide, weekly vinblastine, and rofecoxib in patients with advanced solid tumors and". Clinical Cancer Research 12 (10): 3092–8. doi:10.1158/1078-0432.CCR-05-2255. PMID 16707607.
- ↑ Nicolini A, Mancini P, Ferrari P, et al (2004). "Oral dose cyclophosphamide in metastatic hormone refractory prostate cancer (MHRPC)". Biomed Parmacother. 58 (8): 447–50. doi:10.1016/j.biopha.2004.08.006. PMID 15464874.
- ↑ Nelius T, Klatte T, et al (April 2009). "Clinical outcome of patients with docetaxel-resistant hormone-refractory prostate cancer treated with second-line cyclophosphamide-based metronomic chemotherapy" (PDF). Medical Oncology 27 (2): 363–7. doi:10.1007/s12032-009-9218-8. PMID 19365737.
- ↑ Steinberg AD, Kaltreider HB, Staples PJ, et al. (August 1971). "Cyclophosphamide in lupus nephritis: a controlled trial". Annals of Internal Medicine 75 (2): 165–71. PMID 4104337.
- ↑ Brenner and Rector's The Kidney: Volume 8
- ↑ Townes AS, Sowa JM, Shulman LE (May–June 1976). "Controlled trial of cyclophosphamide in rheumatoid arthritis". Arthritis & Rheumatism 19 (3): 563–73. doi:10.1002/art.1780190308. PMID 779796.
- ↑ Novack SN, Pearson CM. (April 1971). "Cyclophosphamide therapy in Wegener's granulomatosis". New England Journal of Medicine 284 (17): 938–42. doi:10.1056/NEJM197104292841703. PMID 5551803.
- ↑ Makhani N, Gorman MP, Branson HM, et al. (June 2009). "Cyclophosphamide therapy in pediatric multiple sclerosis". Neurology 72 (24): 2076–82. doi:10.1212/WNL.0b013e3181a8164c. PMC 2923592. PMID 19439723.
- ↑ Cohen JL, Jao JY (1970). "Enzymatic basis of cyclophosphamide activation by hepatic microsomes of the rat". Journal of Pharmacology and Experimental Therapeutics 174 (2): 206–10. PMID 4393764.
- ↑ Boddy AV, Yule SM (2000). "Metabolism and pharmacokinetics of oxazaphosphorines.". Clin Pharmacokinet 38 (4): 291–304. doi:10.2165/00003088-200038040-00001. PMID 10803453.
- ↑ 15.0 15.1 Emadi A, Jones RJ, Brodsky RA (2009). "Cyclophosphamide and cancer: golden anniversary.". Nat Rev Clin Oncol 6 (11): 638–47. doi:10.1038/nrclinonc.2009.146. PMID 19786984.
- ↑ http://asheducationbook.hematologylibrary.org/content/2007/1/453.full
- ↑ O.M. Friedman and A.M. Seligman (1954), J. Amer. Chem. Soc. 76, 655
- ↑ O.M. Colvin (August 1999), "An Overview of Cyclophosphamide's Development and Clinical Applications", Current Pharmaceutical Design, 5(8):555–60. Colvin, O. M. (1999). "An overview of cyclophosphamide development and clinical applications". Current pharmaceutical design 5 (8): 555–560. PMID 10469891..
- ↑ Brock N (1996). "The history of the oxazaphosphorine cytostatics". Cancer 78 (3): 542–7. doi:10.1002/(SICI)1097-0142(19960801)78:3<542::AID-CNCR23>3.0.CO;2-Y. PMID 8697402.
- ↑ Wilmanns, H. (1958). Asta-Forschung und Therapie.
- ↑ Gross, R., and Wulf, G. (1959). "Klinische und experimentelle Erfahrungen mit zyk lischen und nichtzyklischen Phosphamidestern des N-Losl in der Chemotherapie von Tumoren". Strahlentherapie. 41 (Sonderband III): 361–367.
- ↑ Brock N (1989). "Oxazaphosphorine cytostatics: past-present-future. Seventh Cain Memorial Award lecture" (PDF). Cancer Res. 49 (1): 1–7. PMID 2491747.