Chigoe flea
| Chigoe flea | |
|---|---|
 | |
| Scientific classification | |
| Kingdom: | Animalia |
| Phylum: | Arthropoda |
| Class: | Insecta |
| Order: | Siphonaptera |
| Family: | Hectopsyllidae |
| Genus: | Tunga |
| Species: | T. penetrans |
| Binomial name | |
| Tunga penetrans (Linnaeus, 1758) | |
.JPG)
.jpg)
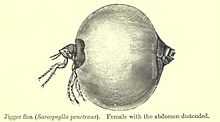
The chigoe flea or jigger (Tunga penetrans) is a parasitic arthropod found in most tropical and sub-tropical climates, not to be confused with the larval form of Trombiculidae (called chiggers) found in more temperate climates. It is native to Central and South America, and has been inadvertently introduced by humans to sub-Saharan Africa.[1] At 1 mm long, the chigoe flea is the smallest known flea.[1] Breeding female chigoes burrow into exposed skin on the feet of mammals and remain there for two weeks while developing eggs, during which time they swell dramatically, sometimes causing intense irritation (condition called tungiasis). After this point, the skin lesion looks like a 5- to 10-mm blister with a central black dot, which are the flea's exposed hind legs, respiratory spiracles and reproductive organs.[2]
If the flea is left within the skin, dangerous complications can occur including secondary infections, loss of nails, and toe deformation. These are relatively rare, but heavy infestations combined with unsanitary conditions greatly increases the likelihood of complications.[1]
The parasitic flea lives in soil and sand, and feeds intermittently on warm-blooded hosts, such as humans, cattle, sheep, dogs, mice (but apparently not rats),[1] and other animals. Males leave the host after a blood meal like other fleas, but the female flea burrows head-first into the host's skin, leaving the caudal tip of its abdomen visible through an orifice in a skin lesion. This orifice allows the chigoe flea to breathe and defecate while feeding on blood vessels in the cutaneous and subcutaneous dermal layer. Over the next two weeks, its abdomen swells with up to several dozen eggs, which it releases through the caudal orifice to fall to the ground when ready to hatch. The flea then dies and is sloughed off with the host's skin. Within the next three to four days, the eggs hatch, and mature into adult fleas within three to four weeks.
Since the fleas spend most of their time on the ground, tungiasis lesions are usually on the feet; however, like most fleas they are capable of jumping up 20 cm, and lesions may occur on any part of the body, favoring regions of soft skin such as between the toes.[1] During the first day or two of infection, the host may feel an itching or irritation which then passes as the area around the flea calluses and becomes insensitive. As the flea's abdomen swells with eggs later in the cycle, the pressure from the swelling may press neighbouring nerves or blood vessels. Depending on the exact site, this can cause sensations ranging from mild irritation to serious discomfort.
A study published in 2006[3] concluded, "Contrary to common belief, a protective effect of frequent use of closed footwear could not be demonstrated."
Synonyms
- Sarcopsylla penetrans
- Pulex penetrans
The chigoe flea, "jigger," is often confused with the chigger, (Trombiculidae) or harvest mite due to the similarity of their names. In Lingala-speaking areas, it is commonly known as liyanzi (singular) or mayanzi (plural). In Kiswahili, it is known as funza. In Brazil, the parasite is referred to as bicho-de-pé (foot bug). In Spanish, the chigoe is commonly known as pique due to the itching and burning sensation it produces; in Colombia, it is known as nigua. In Luganda, it's known as nvunza. In Guarani, the national language of Paraguay, it is known as tũ. In Kinyarwanda and Kirundi, they are known as ivunja or imvunja (singular) or amavunja (plural).
See also
- Tungiasis
- Trombiculidae (chigger) and trombiculosis
External links
| Wikimedia Commons has media related to Tunga penetrans. |
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Cestari TF, Pessato S, Ramos-e-Silva M Tungiasis and myiasis. Clin Dermatol. 2007 Mar-Apr;25(2):158-64.
- ↑ Muehlstaedt M Periungual Tungiasis (2008) Images in clinical medicine. N Engl J Med 359(24):e30.
- ↑ Muehlen M, Feldmeier H, et al. Identifying risk factors for tungiasis and heavy infestation in a resource-poor community in northeast Brazil. Trans R Soc Trop Med Hyg. 2006 Apr;100(4):371-80