Breast augmentation
Breast augmentation and augmentation mammoplasty are plastic surgery terms for the breast-implant and the fat-graft mammoplasty approaches used to increase the size, change the shape, and alter the texture of the breasts of a woman. As a primary reconstruction, augmentation mammoplasty is applied to effect a post–mastectomy breast reconstruction, the repair of the chest wound consequent to the removal of a cancerous breast; to correct congenital defects of the breast(s); and to correct congenital defects of the chest wall. As an elective, cosmetic surgery, primary augmentation changes the aesthetics — of size, shape, and texture — of healthy breasts.

The surgical implantation approach effects the global augmentation of the breast hemisphere using a breast implant, either an implant filled with saline-solution, or an implant filled with silicone-gel; moreover, the surgical augmentation approach can include the application of transplanted autologous skin flaps harvested from the woman’s body. The fat-graft transfer approach augments the size and corrects contour defects of the breast hemisphere with grafts of autologous adipocyte fat tissue, drawn from the woman’s body
In a breast-reconstruction procedure, within a multi-stage reconstruction-mammoplasty, a tissue expander (a temporary breast-implant device) is emplaced and used to prepare (shape and enlarge) the recipient site (implant-pocket) to receive and accommodate the breast implant prosthesis. In a non-implant breast-augmentation procedure, some fat-graft injection approaches feature tissue-engineering, which is the pre-operative, external expansion of the tissues of the recipient site to receive the grafts of adipocyte tissue drawn from the woman’s body. Non-surgical approaches to breast augmentation can consist either of an externally applied vacuum-device that will expand the tissues of the recipient site. Moreover, in most instances of fat-graft breast augmentation the increase is of medium volume — usually one brassière cup-size or less — which usually is the physiologic limit allowed by the metabolism of the woman’s body.[1]
Surgical breast augmentation
Breast implants
For breast reconstruction, and for the augmentation and enhancement of the aesthetics — size, shape, and texture — of a woman’s breasts, there are three types of breast implant devices:
- saline implants filled with sterile saline solution
- silicone implants filled with viscous silicone gel
- alternative-composition implants, filled with miscellaneous fillers — soy oil, polypropylene string, et cetera — that are no longer manufactured.

- I. Saline breast implant
The saline breast implant — filled with saline solution (biological-concentration salt water 0.90% w/v of NaCl, ca. 300 mOsm/L.) — was first manufactured by the Laboratoires Arion company, in France, and was introduced for use as a prosthetic medical device in 1964. The contemporary models of saline breast implant are manufactured with thicker, room-temperature vulcanized (RTV) shells made of a silicone elastomer. The study In vitro Deflation of Pre-filled Saline Breast Implants (2006) reported that the rates of deflation (filler leakage) of the pre-filled saline breast implant made it a second-choice prosthesis for corrective breast surgery.[2] Nonetheless, in the 1990s, the saline breast implant was the prosthesis usual for breast augmentation surgery, because of the U.S. FDA’s restriction against the importation of silicone-filled breast implants.
The technical goal of saline-implant technology was a physically less invasive surgical technique for emplacing an empty breast-implant device through a smaller surgical incision.[3] In surgical praxis, after having emplaced the empty breast implants to the implant pockets, the plastic surgeon then filled each device with saline solution, and, because the required insertion-incisions are short and small, the resultant incision-scars will be smaller and shorter than the surgical scars usual to the long incisions required for inserting pre-filled, silicone-gel implants.
When compared to the results achieved with a silicone-gel breast implant, the saline implant can yield good-to-excellent results, of increased breast-size, smoother hemisphere-contour, and realistic texture; yet, it is likelier to cause cosmetic problems, such as the rippling and the wrinkling of the breast-envelope skin, and technical problems, such as the presence of the implant being noticeable to the eye and to the touch. The occurrence of such cosmetic problems is likelier in the case of the woman with very little breast tissue, and in the case of the woman who requires post-mastectomy breast reconstruction; thus, the silicone-gel implant is the technically superior prosthetic device for breast augmentation, and for breast reconstruction. In the case of the woman with much breast tissue, for whom sub-muscular emplacement is the recommended surgical approach, saline breast implants can afford an aesthetic result much like that afforded by silicone breast implants — a “look” of proportionate breast size, smooth contour, and realistic texture.[4]
- II. Silicone-gel breast implant
The modern prosthetic breast was invented in 1961, by the American plastic surgeons Thomas Cronin and Frank Gerow, and manufactured by the Dow Corning Corporation; in due course, the first augmentation mammoplasty was performed in 1962. There are five generations of medical device technology for the breast-implant models filled with silicone gel; each generation of breast prosthesis is defined by common model-manufacturing techniques.
- First generation
The Cronin–Gerow Implant, prosthesis model 1963, was a silicone rubber envelope-sac, shaped like a teardrop, which was filled with viscous silicone-gel. To reduce the rotation of the emplaced breast-implant upon the chest wall, the model 1963 prosthesis was affixed to the implant pocket with a fastener-patch, made of Dacron material (Polyethylene terephthalate), which was attached to the rear of the breast-implant shell.[5]
- Second generation
In the 1970s, manufacturers presented the second generation of breast-implant prostheses that featured functional developments and aesthetic improvements to the technology:
- the first technological developments were a thinner-gauge device-shell, and a filler gel of low-cohesion silicone, which improved the functionality and the verisimilitude (size, appearance, and texture) of the silicone-gel breast implant. Yet, in clinical practice, second-generation breast implants proved fragile, and suffered greater incidences of shell rupture, and of filler leakage (“silicone-gel bleed”) through the intact device shell. The consequent, increased incidence-rates of medical complications (e.g. capsular contracture) precipitated faulty-product, class action-lawsuits, by the U.S. government, against the Dow Corning Corporation, and other manufacturers of breast prostheses.
- the second technological development was a polyurethane foam coating for the shell of the breast implant; the coating reduced the incidence of capsular contracture, by causing an inflammatory reaction that impeded the formation of a capsule of fibrous collagen tissue around the breast implant. Nevertheless, despite that prophylactic measure, the medical use of polyurethane-coated breast implants was briefly discontinued, because of the potential health-risk posed by 2,4-toluenediamine (TDA), a carcinogenic by-product of the chemical breakdown of the polyurethane foam coating of the breast implant.[6]
- After reviewing the medical data, the U.S. Food and Drug Administration concluded that TDA-induced breast cancer was an infinitesimal health-risk to women with breast implants, and did not justify legally requiring physicians to explain the matter to their patients. In the event, polyurethane-coated breast implants remain in plastic surgery practice in Europe and in South America; and no manufacturer has sought FDA approval for medical sales of such breast implants in the U.S.[7]
- the third technological development was the double lumen breast-implant device, a double-cavity prosthesis composed of a silicone breast-implant contained within a saline breast-implant. The two-fold, technical goal was: (i) the cosmetic benefits of silicone-gel (the inner lumen) enclosed in saline solution (the outer lumen); (ii) a breast-implant device the volume of which is post-operatively adjustable. Nevertheless, the more complex design of the double-lumen breast-implant suffered a device-failure rate greater than that of single-lumen breast implants. The contemporary versions of second-generation breast-implant devices (presented in 1984) are the “Becker Expandable” models of breast implant, which are primarily used for breast reconstruction.
- Third and Fourth generations
In the 1980s, the models of the Third and of the Fourth generations of breast-implant devices were sequential advances in manufacturing technology, such as elastomer-coated shells that decreased gel-bleed (filler leakage), and a thicker (increased-cohesion) filler gel. Sociologically, the manufacturers of prosthetic breasts then designed and made anatomic models (natural breast) and shaped models (round, tapered) that realistically corresponded with the breast- and body- types of women. The tapered models of breast implant have a uniformly textured surface, which reduces the rotation of the prosthesis within the implant pocket; the round models of breast implant are available in smooth-surface- and textured-surface- types.
- Fifth generation
Since the mid-1990s, the Fifth generation of silicone-gel breast implant is made of a semi-solid gel that mostly eliminates the occurrences of filler leakage (“silicone-gel bleed”) and of the migration of the silicone filler from the implant-pocket to elsewhere in the woman’s body. The studies Experience with Anatomical Soft Cohesive Silicone gel Prosthesis in Cosmetic and Reconstructive Breast Implant Surgery (2004) and Cohesive Silicone gel Breast Implants in Aesthetic and Reconstructive Breast Surgery (2005) reported low incidence-rates of capsular contracture and of device-shell rupture; and greater rates of improved medical-safety and technical-efficacy than that of early generation breast-implant devices.[8][9][10]
Implants and breast-feeding
The breasts are apocrine glands that produce milk for the feeding of infant children; each breast has a nipple within an areola (nipple-areola complex, NAC), the skin color of which varies from pink to dark brown, and has sebaceous glands. Within the mammary gland, the lactiferous ducts produce breast milk, and are distributed throughout the breast, with two-thirds of the tissue within 30 mm of the base of the nipple. In each breast, 4–18 lactiferous ducts drain to the nipple; the glands-to-fat ratio is 2:1 in lactating women, and to 1:1 in non-lactating women; besides milk glands, the breast is composed of connective tissue (collagen, elastin), adipose tissue (white fat), and the suspensory Cooper's ligaments. The peripheral nervous system innervation of the breast is by the anterior and lateral cutaneous branches of the fourth, fifth, and sixth intercostal nerves, while the thoracic spinal nerve 4 (T4) innervating the dermatomic area supplies sensation to the nipple-areola complex.[11][12]

1. Chest wall
2. Pectoralis muscles
3. Lobules
4. Nipple
5. Areola
6. Milk duct
7. Fatty tissue
8. Skin envelope

- The functional breast
Digestive contamination and systemic toxicity are the principal infant-health concerns; the leakage of breast implant filler to the breast milk, and if the filler is dangerous to the nursing infant. Breast implant device fillers are biologically inert—saline filler is salt water, and silicone filler is indigestible—because each substance is chemically inert, and environmentally common. Moreover, proponent physicians have said there “should be no absolute contraindication to breast-feeding by women with silicone breast implants.”[13] In the early 1990s, at the beginning of the silicone breast-implant sickness occurrences, small-scale, non-random studies (i.e. “patients came with complaints, which might have many sources”, not “doctors performed random tests”) indicated possible breast-feeding complications from silicone implants; yet no study reported device–disease causality.[14]
- The augmented breast
The woman with breast implants is able to breast-feed her infant; yet breast implant devices occasionally cause functional breast-feeding difficulties, especially the mammoplasty procedures that feature periareolar incisions and subglandular emplacement, which have greater incidences of breast-feeding difficulties. Therefore, to ensure her breast-feeding functionality post-surgery, the woman of child-bearing age seeking breast implants discusses with her plastic surgeon the implantation procedure that will least damage her lactiferous ducts and the nerves of the nipple-areola complex (NAC).[15][16][17] Before the augmentation mammoplasty, the woman consults with a lactation consultant, to learn what post-operative lactation and breast-feeding conditions to expect; and consults with the plastic surgeon to jointly decide upon the implantation procedure and surgical techniques that will least damage the breast nerves, the milk ducts, the T4 dermatomic area and the lactiferous ducts, so that she might nurse her infant child.
Functional breast-feeding difficulties arise if the surgeon cut the milk ducts or the major nerves innervating the breast, or if the milk glands were otherwise damaged. Milk duct and nerve damage are more common to the periareolar incision implantation procedure, which cuts tissue near the nipple, whereas other implantation incision-plans—IMF (inframammary fold), TABA (Trans-Axillary Breast Augmentation), TUBA (trans-umbilical breast augmentation)—avoid the tissue of the nipple-areola complex; if the woman is concerned about possible breast-feeding difficulties, the periareolar incisions can be effected to reduce damage to the milk ducts and to the nerves of the NAC. The milk glands are affected most by subglandular implants (under the gland), and by large-sized breast implants, which pinch the lactiferous ducts and impede milk flow. Small-sized breast implants, and submuscular implantation, cause fewer breast-function problems; however, women have successfully breast-fed after undergoing periareolar incisions and subglandular emplacement.[17]
The patient
Psychology
The usual breast augmentation patient is a young woman whose personality profile indicates psychological distress about her personal appearance and her body (self image), and a history of having endured criticism (teasing) about the aesthetics of her person.[18] The studies Body Image Concerns of Breast Augmentation Patients (2003) and Body Dysmorphic Disorder and Cosmetic Surgery (2006) reported that the woman who underwent breast augmentation surgery also had undergone psychotherapy, suffered low self-esteem, presented frequent occurrences of psychological depression, had attempted suicide, and suffered body dysmorphia—a type of mental illness wherein she perceives non-existent physical defects. Post-operative patient surveys about the mental health and the quality of life of the women, reported improved physical health, physical appearance, social life, self-confidence, self-esteem, and satisfactory sexual functioning. Furthermore, most of the women reported long-term satisfaction with their breast implants; some despite having suffered medical complications that required surgical revision, either corrective or aesthetic. Likewise, in Denmark, 8.0 per cent of breast augmentation patients had a pre-operative history of psychiatric hospitalization.[19][20][21][22][23][24][25][26][27]
Women bodybuilders

The Cosmeticsurgery.com article They Need Bosoms, too—Women Weight Lifters (2013) reported that women weight-lifters have resorted to breast augmentation surgery to maintain a feminine physique, and so compensate for the loss of breast mass consequent to the increased lean-body mass and decreased body-fat consequent to lifting weights.[28]
Mental health
The longitudinal study Excess Mortality from Suicide and other External Causes of Death Among Women with Cosmetic Breast Implants (2007), reported that women who sought breast implants are almost 3.0 times as likely to commit suicide as are women who have not sought breast implants. Compared to the standard suicide-rate for women of the general populace, the suicide-rate for women with augmented breasts remained alike until 10-years post-implantation, yet it increased to 4.5 times greater at the 11-year mark, and so remained until the 19-year mark, when it increased to 6.0 times greater at 20-years post-implantation. Moreover, additional to the suicide-risk, women with breast implants also faced a trebled death risk from alcoholism and drugs abuse (prescription and recreational).[29][30] Although seven studies have statistically connected a woman’s undergoing a breast augmentation procedure to a greater suicide-rate, the research indicates that augmenation surgery does not increase the suicide death-rate; and that, in the first instance, it is the psychopathologically-inclined woman who is likelier to undergo breast augmentation.[31][32][33][34][35][36]
Moreover, the study Effect of Breast Augmentation Mammoplasty on Self-Esteem and Sexuality: A Quantitative Analysis (2007), reported that the women attributed their improved self-esteem, self-image, and increased, satisfactory sexual functioning to having undergone breast augmentation; the cohort, aged 21–57 years, averaged post-operative self-esteem increases ranging from 20.7 to 24.9 points on the 30-point Rosenberg self-esteem scale, which data supported the 78.6 per cent increase in the woman’s libido, relative to her pre-operative level of libido. Therefore, before agreeing to any surgical procedure, the plastic surgeon evaluates and considers the woman’s mental health to determine if breast implants can positively affect her self-esteem and sexual functioning.[37]
Surgical procedures
Indications

An augmenation mammoplasty for emplacing breast implants has three therapeutic purposes:
- primary reconstruction: to replace breast tissues damaged by trauma (blunt, penetrating, blast), disease (breast cancer), and failed anatomic development (tuberous breast deformity).
- revision and reconstruction: to revise (correct) the outcome of a previous breast reconstruction surgery.
- primary augmentation: to aesthetically augment the size, form, and feel of the breasts.
The operating room time of post–mastectomy breast reconstruction, and of breast augmentation surgery is determined by the emplacement procedure employed, the type of incisional technique, the breast implant (type and materials), and the pectoral locale of the implant pocket.
Incision types
The emplacement of a breast implant device is performed with five types of surgical incisions:[38]
- Inframammary: an incision made below the breast, in the infra-mammary fold (IMF), which affords maximal access for precise dissection and emplacement of the breast implant devices. It is the preferred surgical technique for emplacing silicone-gel implants, because of the longer incisions required; yet, IMF implantation can produce thicker, slightly more visible surgical scars.
- Periareolar: an incision made along the areolar periphery (border), which provides an optimal approach when adjustments to the IMF position are required, or when a mastopexy (breast lift) is included to the primary mammoplasty procedure. In the periareolar emplacement method, the incision is around the medial-half (inferior half) of the areola’s circumference. Silicone-gel implants can be difficult to emplace with this incision, because of the short, five-centimetre length (~ 5.0 cm.) of the required access-incision. Aesthetically, because the scars are at the areola’s border, they usually are less visible than the IMF-incision scars of women with light-pigment areolae. Furthermore, periareolar implantation produces a greater incidence of capsular contracture, severs the milk ducts and the nerves to the nipple, thus causes the most post-operative functional problems, e.g. impeded breast feeding.
- Transaxillary: an incision made to the axilla (armpit), from which the dissection tunnels medially, thus allows emplacing the implants without producing visible scars upon the breast proper; yet is likelier to produce inferior asymmetry of the implant-device position. Therefore, surgical revision of transaxillary emplaced breast implants usually requires either an IMF incision or a periareolar incision. Transaxillary emplacement can be performed bluntly or with an endoscope (illuminated video microcamera).
- Transumbilical: a trans-umbilical breast augmentation (TUBA) is a less common implant-device insertion technique wherein the incision is at the navel, and the dissection tunnels superiorly. This surgical approach enables emplacing the breast implants without producing visible scars upon the breast; but it makes appropriate dissection and device-emplacement more technically difficult. A TUBA procedure is performed bluntly—without the endoscope’s visual assistance—and is not appropriate for emplacing (pre-filled) silicone-gel implants, because of the great potential for damaging the elastomer silicone shell of the breast-implant device during its manual insertion through the short—two-centimetre (~2.0 cm.)—incision at the navel, and because pre-filled silicone-gel implants are incompressible, and cannot be inserted through so small an incision.[39]
- Transabdominal—as in the TUBA procedure, in the transabdominoplasty breast augmentation (TABA), the breast implants are tunneled superiorly from the abdominal incision into bluntly dissected implant pockets, whilst the patient simultaneously undergoes an abdominoplasty.[40]
Implant pocket placement
The four (4) surgical approaches to emplacing a breast implant to the implant pocket are described in anatomical relation to the pectoralis major muscle.
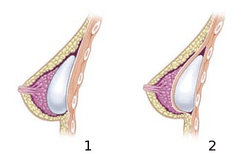
- Subglandular — the breast implant is emplaced to the retromammary space, between the breast tissue (the mammary gland) and the pectoralis major muscle (major muscle of the chest), which most approximates the plane of normal breast tissue, and affords the most aesthetic results. Yet, in women with thin pectoral soft-tissue, the subglandular position is likelier to show the ripples and wrinkles of the underlying implant. Moreover, the capsular contracture incidence rate is slightly greater with subglandular implantation.
- Subfascial — the breast implant is emplaced beneath the fascia of the pectoralis major muscle; the subfascial position is a variant of the subglandular position for the breast implant.[41] The technical advantages of the subfascial implant-pocket technique are debated; proponent surgeons report that the layer of fascial tissue provides greater implant coverage and better sustains its position.[42]
- Subpectoral (dual plane) — the breast implant is emplaced beneath the pectoralis major muscle, after the surgeon releases the inferior muscular attachments, with or without partial dissection of the subglandular plane. Resultantly, the upper pole of the implant is partially beneath the pectoralis major muscle, while the lower pole of the implant is in the subglandular plane. This implantation technique achieves maximal coverage of the upper pole of the implant, whilst allowing the expansion of the implant’s lower pole; however, “animation deformity”, the movement of the implants in the subpectoral plane can be excessive for some patients.[43]
- Submuscular — the breast implant is emplaced beneath the pectoralis major muscle, without releasing the inferior origin of the muscle proper. Total muscular coverage of the implant can be achieved by releasing the lateral muscles of the chest wall — either the serratus muscle or the pectoralis minor muscle, or both — and suturing it, or them, to the pectoralis major muscle. In breast reconstruction surgery, the submuscular implantation approach effects maximal coverage of the breast implants.
Post-surgical recovery
The surgical scars of a breast augmentation mammoplasty heal at 6-weeks post-operative, and fade within several months, according to the skin type of the woman. Depending upon the daily physical activity the woman might require, the augmentation mammoplasty patient usually resumes her normal life activities at about 1-week post-operative. The woman who underwent submuscular implantation (beneath the pectoralis major muscles) usually has a longer post–operative convalescence, and experiences more pain, because of the healing of the deep-tissue cuts into the chest muscles for the breast augmenation. The patient usually does not exercise or engage in strenuous physical activities for about 6 weeks. Moreover, during the initial convalescence, the patient is encouraged to regularly exercise (flex and move) her arms to alleviate pain and discomfort; and, as required, analgesic medication catheters for alleviating pain.[44][45]
Medical complications
The plastic surgical emplacement of breast-implant devices, either for breast reconstruction or for aesthetic purpose, presents the same health risks common to surgery, such as adverse reaction to anesthesia, hematoma (post-operative bleeding), seroma (fluid accumulation), incision-site breakdown (wound infection). Complications specific to breast augmentation include breast pain, altered sensation, impeded breast-feeding function, visible wrinkling, asymmetry, thinning of the breast tissue, and symmastia, the “bread loafing” of the bust that interrupts the natural plane between the breasts. Specific treatments for the complications of indwelling breast implants—capsular contracture and capsular rupture—are periodic MRI monitoring and physical examinations. Furthermore, complications and re-operations related to the implantation surgery, and to tissue expanders (implant place-holders during surgery) can cause unfavorable scarring in approximately 6–7% of the patients. [26][46][47] Statistically, 20% of women who underwent cosmetic implantation, and 50% of women who underwent breast reconstruction implantation, required their explantation at the 10-year mark.[48]
Implant rupture
Because a breast implant is a Class III medical device of limited product-life, the principal rupture-rate factors are its age and design; Nonetheless, a breast implant device can retain its mechanical integrity for decades in a woman’s body.[49] When a saline breast implant ruptures, leaks, and empties, it quickly deflates, and thus can be readily explanted (surgically removed). The follow-up report, Natrelle Saline-filled Breast Implants: a Prospective 10-year Study (2009) indicated rupture-deflation rates of 3–5 per cent at 3-years post-implantation, and 7–10 per cent rupture-deflation rates at 10-years post-implantation.[50]

When a silicone breast implant ruptures it usually does not deflate, yet the filler gel does leak from it, which can migrate to the implant pocket; therefore, an intracapsular rupture (in-capsule leak) can become an extracapsular rupture (out-of-capsule leak), and each occurrence is resolved by explantation. Although the leaked silicone filler-gel can migrate from the chest tissues to elsewhere in the woman’s body, most clinical complications are limited to the breast and armpit areas, usually manifested as granulomas (inflammatory nodules) and axillary lymphadenopathy (enlarged lymph glands in the armpit area).[51][52][53]
- The suspected mechanisms of breast-implant rupture are
- damage during implantation
- damage during (other) surgical procedures
- chemical degradation of the breast implant shell
- trauma (blunt trauma, penetrating trauma, blast trauma)
- mechanical pressure of traditional mammographic breast examination [54]
Silicone implant rupture can be evaluated using magnetic resonance imaging; from the long-term MRI data for single-lumen breast implants, the European literature about second generation silicone-gel breast implants (1970s design), reported silent device-rupture rates of 8–15 per cent at 10-years post-implantation (15–30% of the patients).[55][56][57][58]
The study Safety and Effectiveness of Mentor’s MemoryGel Implants at 6 Years (2009), which was a branch study of the U.S. FDA’s core clinical trials for primary breast augmentation surgery patients, reported low device-rupture rates of 1.1 per cent at 6-years post-implantation.[59] The first series of MRI evaluations of the silicone breast implants with thick filler-gel reported a device-rupture rate of 1.0 per cent, or less, at the median 6-year device-age.[60] Statistically, the manual examination (palpation) of the woman is inadequate for accurately evaluating if a breast implant has ruptured. The study, The Diagnosis of Silicone Breast-implant Rupture: Clinical Findings Compared with Findings at Magnetic Resonance Imaging (2005), reported that, in asymptomatic patients, only 30 per cent of the of ruptured breast implants is accurately palpated and detected by an experienced plastic surgeon, whereas MRI examinations accurately detected 86 per cent of breast-implant ruptures.[61] Therefore, the U.S. FDA recommended scheduled MRI examinations, as silent-rupture screenings, beginning at the 3-year-mark post-implantation, and then every two years, thereafter.[26] Nonetheless, beyond the U.S., the medical establishments of other nations have not endorsed routine MRI screening, and, in its stead, proposed that such a radiologic examination be reserved for two purposes: (i) for the woman with a suspected breast-implant rupture; and (ii) for the confirmation of mammographic and ultrasonic studies that indicate the presence of a ruptured breast implant.[62]
Furthermore, The Effect of Study design Biases on the Diagnostic Accuracy of Magnetic Resonance Imaging for Detecting Silicone Breast Implant Ruptures: a Meta-analysis (2011) reported that the breast-screening MRIs of asymptomatic women might overestimate the incidence of breast-implant rupture.[63] In the event, the U.S. Food and Drug Administration emphasised that “breast implants are not lifetime devices. The longer a woman has silicone gel-filled breast implants, the more likely she is to experience complications.”[64]
Capsular contracture
The human body’s immune response to a surgically installed foreign object — breast implant, cardiac pacemaker, orthopedic prosthesis — is to encapsulate it with scar tissue capsules of tightly woven collagen fibers, in order to maintain the integrity of the body by isolating the foreign object, and so tolerate its presence. Capsular contracture — which should be distinguished from normal capsular tissue — occurs when the collagen-fiber capsule thickens and compresses the breast implant; it is a painful complication that might distort either the breast implant, or the breast, or both.

The cause of capsular contracture is unknown, but the common incidence factors include bacterial contamination, device-shell rupture, filler leakage, and hematoma. The surgical implantation procedures that have reduced the incidence of capsular contracture include submuscular emplacement, the use of breast implants with a textured surface (polyurethane-coated);[65][66][67] limited pre-operative handling of the implants, limited contact with the chest skin of the implant pocket before the emplacement of the breast implant, and irrigation of the recipient site with triple-antibiotic solutions.[68][69]
The correction of capsular contracture might require an open capsulotomy (surgical release) of the collagen-fiber capsule, or the removal, and possible replacement, of the breast implant. Furthermore, in treating capsular contracture, the closed capsulotomy (disruption via external manipulation) once was a common maneuver for treating hard capsules, but now is a discouraged technique, because it can rupture the breast implant. Non-surgical treatments for collagen-fiber capsules include massage, external ultrasonic therapy, leukotriene pathway inhibitors such as zafirlukast (Accolate) or montelukast (Singulair), and pulsed electromagnetic field therapy (PEMFT).[70][71][72][73]
Repair and revision surgeries
When the woman is unsatisfied with the outcome of the augmentation mammoplasty; or when technical or medical complications occur; or because of the breast implants’ limited product life (Class III medical device, in the U.S.), it is likely she might require replacing the breast implants. The common revision surgery indications include major and minor medical complications, capsular contracture, shell rupture, and device deflation.[54] Revision incidence rates were greater for breast reconstruction patients, because of the post-mastectomy changes to the soft-tissues and to the skin envelope of the breast, and to the anatomical borders of the breast, especially in women who received adjuvant external radiation therapy.[54] Moreover, besides breast reconstruction, breast cancer patients usually undergo revision surgery of the nipple-areola complex (NAC), and symmetry procedures upon the opposite breast, to create a bust of natural appearance, size, form, and feel. Carefully matching the type and size of the breast implants to the patient’s pectoral soft-tissue characteristics reduces the incidence of revision surgery. Appropriate tissue matching, implant selection, and proper implantation technique, the re-operation rate was 3.0% at the 7-year-mark, compared with the re-operation rate of 20% at the 3-year-mark, as reported by the U.S. Food and Drug Administration.[74][75]
Systemic disease and sickness
Since the 1990s, reviews of the studies that sought causal links between silicone-gel breast implants and systemic disease reported no link between the implants and subsequent systemic and autoimmune diseases.[62][76][77][78] Nonetheless, during the 1990s, thousands of women claimed sicknesses they believed were caused by their breast implants, including neurological and rheumatological health problems.

In the study Long-term Health Status of Danish Women with Silicone Breast Implants (2004), the national healthcare system of Denmark reported that women with implants did not risk a greater incidence and diagnosis of autoimmune disease, when compared to same-age women in the general population; that the incidence of musculoskeletal disease was lower among women with breast implants than among women who had undergone other types of cosmetic surgery; and that they had a lower incidence rate than like women in the general population.[79][80]
Follow-up longitudinal studies of these breast implant patients confirmed the previous findings on the matter.[81] European and North American studies reported that women who underwent augmentation mammoplasty, and any plastic surgery procedure, tended to be healthier and wealthier than the general population, before and after implantation; that plastic surgery patients had a lower standardized mortality ratio than did patients for other surgeries; yet faced an increased risk of death by lung cancer than other plastic surgery patients. Moreover, because only one study, the Swedish Long-term Cancer Risk Among Swedish Women with Cosmetic Breast Implants: an Update of a Nationwide Study (2006), controlled for tobacco smoking information, the data were insufficient to establish verifiable statistical differences between smokers and non-smokers that might contribute to the higher lung cancer mortality rate of women with breast implants.[82][83] The long-term study of 25,000 women, Mortality among Canadian Women with Cosmetic Breast Implants (2006), reported that the “findings suggest that breast implants do not directly increase mortality in women.”[34]
The study Silicone gel Breast Implant Rupture, Extracapsular Silicone, and Health Status in a Population of Women (2001), reported increased incidences of fibromyalgia among women who suffered extracapsular silicone-gel leakage than among women whose breast implants neither ruptured nor leaked.[84] The study later was criticized as significantly methodologically flawed, and a number of large subsequent follow-up studies have not shown any evidence of a causal device–disease association. After investigating, the U.S. FDA has concluded “the weight of the epidemiological evidence published in the literature does not support an association between fibromyalgia and breast implants.”.[85][86] The systemic review study, Silicone Breast implants and Connective tissue Disease: No Association (2011) reported the investigational conclusion that “any claims that remain regarding an association between cosmetic breast implants and CTDs are not supported by the scientific literature”.[87]
Platinum toxicity
The manufacture of silicone breast implants requires the metallic element Platinum (Pt., 78) as a catalyst to accelerate the transformation of silicone oil into silicone gel for making the elastomer silicone shells, and for making other medical-silicone devices.[88] The literature indicates that trace quantities of platinum leak from such types of silicone breast implant; therefore, platinum is present in the surrounding pectoral tissue(s). The rare pathogenic consequence is an accumulation of platinum in the bone marrow, from where blood cells might deliver it to nerve endings, thus causing nervous system disorders such as blindness, deafness, and nervous tics (involuntary muscle contractions).[88]
In 2002, the U.S. Food and Drug Administration (U.S. FDA) reviewed the studies on the human biological effects of breast-implant platinum, and reported little causal evidence of platinum toxicity to women with breast implants.[89] Furthermore, in the journal “Analytical Chemistry”, the study Total Platinum Concentration and Platinum Oxidation States in Body Fluids, Tissue, and Explants from Women Exposed to Silicone and Saline Breast Implants by IC-ICPMS (2006), proved controversial for claiming to have identified previously undocumented toxic platinum oxidative states in vivo.[90] Later, in a letter to the readers, the editors of the “Analytical Chemistry” journal published their concerns about the faulty experimental design of the study, and warned readers to “use caution in evaluating the conclusions drawn in the paper.”[91]
Furthermore, after reviewing the research data of the study Total Platinum Concentration and Platinum Oxidation States in Body Fluids, Tissue, and Explants from Women Exposed to Silicone and Saline Breast Implants by IC-ICPMS, and other pertinent literature, the U.S. FDA reported that the data do not support the findings presented; that the platinum used, in new-model breast-implant devices, likely is not ionized, and therefore is not a significant risk to the health of the women.[92]
Non-implant breast augmentation
Technical background
- Liposuction
The technique of liposuction (lipoplasty) was conceived and developed by the Italian plastic surgeons Arpat Fischer and Giorgio Fischer in 1974, and was put into medico-clinical practice in 1975.[93] Access to the woman’s autologous adipocyte fat was by means of 5-mm incisions, and was harvested with an electrically and pneumatically –powered instrument, which rotated and alternated in its aspiration of the fat through a cannula. Meanwhile, through a separate incision to the fat-tissue harvest site, saline solution was injected to dilute the body fat, and so facilitate its aspiration.[94]
In 1977, Fisher and Fischer reviewed 245 cases with the planotome instrument for treating cellulite in the lateral trochanteric (hip-thigh) areas. There was a 4.9 per cent incidence of seromas, despite incision-wound suction catheters and compression dressings; 2.0 per cent of the cases presented pseudo-cyst formation that required removal of the capsule (cyst) through a wider incision (+ 5.0 mm) and the use of the panotome.[95][96]
The advent of liposuction technology facilitated medical applications of the liposuction-harvested fat tissue as autologous filler for injection to correct bodily defects, and for breast augmentation. Dr. Melvin Bircoll introduced the practice of contouring the breast and for correcting bodily defects with autologous fat grafts harvested by liposuction; and he presented the fat-injection method used for emplacing the fat grafts.[97][98] The surgeon E. Krulig emplaced fat grafts with a syringe and needle (lipo-injection), and later used a disposable fat trap to facilitate the collection and to ensure the sterility of the harvested adipocyte tissue.[99][100]
- Lipo-injector gun
To emplace the grafts of autologous fat-tissue, doctors J. Newman and J. Levin designed a lipo-injector gun with a gear-driven plunger, which allowed the even injection of autologous fat-tissue to the desired recipient sites. The control afforded by the lipo-injector gun assisted the plastic surgeon in controlling excessive pressure to the fat in the barrel of the syringe, thus avoiding over-filling the recipient site.[101] The later-design lipo-injector gun featured a ratchet-gear operation that afforded the surgeon greater control in accurately emplacing grafts of autologous fat to the recipient site; a trigger action injected 0.1 cm3 of filler.[102] Since 1989, most non-surgical, fat-graft augmentation of the breast features the emplacement of adipocyte fat outside the breast parenchyma — up to 300 ml of fat — in three equal measures (aliquots), is emplaced to the subpectoral space and to the intrapectoral space of the pectoralis major muscle, and the submammary space, to achieve a breast outcome of natural appearance and contour.[103]
Autologous fat grafting
The technique of autologous fat-graft injection to the breast is applied for the correction of breast asymmetry; of breast deformities; for post-mastectomy breast reconstruction (as a primary and as an adjunct technique); for the improvement of soft-tissue coverage of breast implants; and for the aesthetic enhancement of the bust. The careful harvesting and centrifugal refinement of the mature adipocyte tissue (injected in small aliquots) allows the transplanted fat tissue to remain viable in the breast, where it provides the anatomical structure and the hemispheric contour that cannot be achieved solely with breast implants or with corrective plastic surgery.

In fat-graft breast augmentation procedures, there is the risk that the adipocyte tissue grafted to the breast(s) can undergo necrosis, metastatic calcification, develop cysts, and agglomerate into palpable lumps. Although the cause of metastatic calcification is unknown, the post-procedure biological changes occurred to the fat-graft tissue resemble the tissue changes usual to breast surgery procedures such as reduction mammoplasty. The French study Radiological Evaluation of Breasts Reconstructed with Lipo-modeling (2005) indicates the therapeutic efficacy of fat-graft breast reconstruction in the treatment of radiation therapy damage to the chest, the incidental reduction of capsular contracture, and the improved soft-tissue coverage of breast implants.[104][105][106][107][108][109]
The study Fat Grafting to the Breast Revisited: Safety and Efficacy (2007) reported successful transferences of body fat to the breast, and proposed the fat-graft injection technique as an alternative (non-implant) augmentation mammoplasty procedure instead of the surgical procedures usual for effecting breast augmentation, breast-defect correction, and breast reconstruction.
In a 17-patient cohort, two women had breast cancer (diagnosed by mammogram) one at 12-months post-procedure, and the other at 92-months post-procedure. In contemporary surgical praxis, to realize the required correction, aside from the breast proper, fat grafts are injected to the pectoralis major muscle, to the postpectoral space and to the prepectoral space, before and behind said muscle. In post-mastectomy breast reconstruction, the grafted fat is used to create a breast mound, by augmenting the extant breast tissues that remained after the surgical removal of the cancerous breast. Structural fat-grafting was performed either to one breast or to both breasts of the 17 women; the age range of the women was 25–55 years, and the mean age was 38.2 years. The women of the study cohort presented clinical indications such as micromastia (10 patients); explantation deformity (one patient); post-augmentation deformity, with breast implants (two patients); tuberous breast deformity (one patient); Poland’s syndrome (one patient); and post-mastectomy reconstruction deformity (two patients).
The pre-procedure mammograms were negative for malignant neoplasms. The types of anaesthesia applied were general (two patients) and epidural analgesia plus sedation, with local infiltration and intercostal nerve blocks (15 patients). The autologous adipocyte tissue was grafted in one-to-three stages; the average volume of a tissue-graft was 278.6 cm3 of fat per operation, per breast. Post-procedure, each patient was instructed to regard any lump in the breasts as unrelated to the fat grafts, until after a complete medical workup of the breast lump had been performed.[110] Moreover, the study Cell-assisted Lipotransfer for Cosmetic Breast Augmentation: Supportive Use of Adipose-Derived Stem/Stromal Cells (2007), about a 40-woman cohort, indicated that the inclusion of adipose stem cells to the grafts of adipocyte fat increased the rate of corrective success of the autologous fat-grafting procedure.[111]
Fat grafting techniques
- Fat harvesting and contouring
The centrifugal refinement of the liposuction-harvested adipocyte tissues removes blood products and free lipids to produce autologous breast filler. The injectable filler-fat is obtained by centrifuging (spinning) the fat-filled syringes for sufficient time to allow the serum, blood, and oil (liquid fat) components to collect, by density, apart from the refined, injection-quality fat.[112] To refine the fat for facial injection quality, the fat-filled syringes are centrifuged for 1.0 minute at 2,000 RPM, which separates the unnecessary solution, leaving refined filler-fat.[113] Moreover, centrifugation at 10,000 RPM for 10 minutes produces a “collagen graft”; the histologic composition of which is cell residues, collagen fibres, and 5.0 per cent intact fat cells. Furthermore, because the patient’s body naturally absorbs some of the fat grafts, the breasts maintain their contours and volumes for 18–24 months.[114][115]

In the study Fat Grafting to the Breast Revisited: Safety and Efficacy (2007), the investigators reported that the autologous fat was harvested by liposuction, using a 10-ml syringe attached to a two-hole Coleman harvesting cannula; after centrifugation, the refined breast-filler fat was transferred to 3-ml syringes. Blunt infiltration cannulas were used to emplace the fat through 2-mm incisions; the blunt cannula injection method allowed greater dispersion of small aliquots (equal measures) of fat, and reduced the possibility of intravascular fat injection; no sharp needles are used for fat-graft injection to the breasts. The 2-mm incisions were positioned to allow the infiltration (emplacement) of fat grafts from at least two directions; a 0.2 ml fat volume was emplaced with each withdrawal of the cannula.[116]
The breasts were contoured by layering the fat grafts into different levels within the breast, until achieving the desired breast form. The fat-graft injection technique allows the plastic surgeon precise control in accurately contouring the breast—from the chest wall to the breast-skin envelope—with subcutaneous fat grafts to the superficial planes of the breast. This greater degree of breast sculpting is unlike the global augmentation realised with a breast implant emplaced below the breast or below the pectoralis major muscle, respectively expanding the retromammary space and the retropectoral space. The greatest proportion of the grafted fat usually is infiltrated to the pectoralis major muscle, then to the retropectoral space, and to the prepectoral space, (before and behind the pectoralis major muscle). Moreover, although fat grafting to the breast parenchyma usually is minimal, it is performed to increase the degree of projection of the bust.[110]
- Fat-graft injection
The biologic survival of autologous fat tissue depends upon the correct handling of the fat graft, of its careful washing (refinement) to remove extraneous blood cells, and of the controlled, blunt-cannula injection (emplacement) of the refined fat-tissue grafts to an adequately vascularized recipient site. Because the body resorbs some of the injected fat grafts (volume loss), compensative over-filling aids in obtaining a satisfactory breast outcome for the patient; thus the transplantation of large-volume fat grafts greater than required, because only 25–50 per cent of the fat graft survives at 1-year post-transplantation.[117]
The correct technique maximizes fat graft survival by minimizing cellular trauma during the liposuction harvesting and the centrifugal refinement, and by injecting the fat in small aliquots (equal measures), not clumps (too-large measures). Injecting minimal-volume aliquots with each pass of the cannula maximizes the surface area contact, between the grafted fat-tissue and the recipient breast-tissue, because proximity to a vascular system (blood supply) encourages histologic survival and minimizes the potential for fat necrosis.[110] Transplanted autologous fat tissue undergoes histologic changes like those undergone by a bone transplant; if the body accepts the fat-tissue graft, it is replaced with new fat tissue, if the fat-graft dies it is replaced by fibrous tissue. New fat tissue is generated by the activity of a large, wandering histocyte-type cell, which ingests fat and then becomes a fat cell.[118] When the breast-filler fat is injected to the breasts in clumps (too-large measures), fat cells emplaced too distant from blood vessels might die, which can lead to fat tissue necrosis, causing lumps, calcifications, and the eventual formation of liponecrotic cysts.

The operating room (OR) time required to harvest, refine, and emplace fat to the breasts is greater than the usual 2-hour OR time; the usual infiltration time was approximately 2-hours for the first 100 cm3 volume, and approximately 45 minutes for injecting each additional 100 cm3 volume of breast-filler fat. The technique for injecting fat grafts for breast augmentation allows the plastic surgeon great control in sculpting the breasts to the required contour, especially in the correction of tuberous breast deformity. In which case, no fat-graft is emplaced beneath the nipple-areola complex (NAC), and the skin envelope of the breast is selectively expanded (contoured) with subcutaneously emplaced body-fat, immediately beneath the skin. Such controlled contouring selectively increased the proportional volume of the breast in relation to the size of the nipple-areola complex, and thus created a breast of natural form and appearance; greater verisimilitude than is achieved solely with breast implants. The fat-corrected, breast-implant deformities, were inadequate soft-tissue coverage of the implant(s) and capsular contracture, achieved with subcutaneous fat-grafts that hid the implant-device edges and wrinkles, and decreased the palpability of the underlying breast implant. Furthermore, grafting autologous fat around the breast implant can result in softening the breast capsule.[119]
- External tissue expansion
The successful outcome of fat-graft breast augmentation is enhanced by achieving a pre-expanded recipient site to create the breast-tissue matrix that will receive grafts of autologous adipocyte fat. The recipient site is expanded with an external vacuum tissue-expander applied upon each breast. The biological effect of negative pressure (vacuum) expansion upon soft tissues derives from the ability of soft tissues to grow when subjected to controlled, distractive, mechanical forces. (see distraction osteogenesis) The study Non-surgical Breast Enlargement using an External Soft Tissue Expansion System (2000) reported the technical effectiveness of recipient-site pre-expansion. In a single-group study, 17 healthy women (aged 18–40 years) wore a brassiere-like vacuum system that applied a 20-mmHg vacuum (controlled, mechanical, distraction force) to each breast for 10–12 hours daily for 10-weeks. Pre- and post-procedure, the breast volume (size) was periodically measured; likewise, a magnetic resonance image (MRI) of the breast-tissue architecture and water density was taken during the same phase of the patient’s menstrual cycle; of the 17-woman study group, 12 completed the study, and 5 withdrew, because of non-compliance with the clinical trial protocol.[120]
The breast volume (size) of all 17 women increased throughout the 10-week treatment period, the greatest increment was at week 10 (final treatment)—the average volume increase was 98+/–67 per cent over the initial breast-size measures. Incidences of partial recoil occurred at 1-week post-procedure, with no further, significant, breast volume decrease afterwards, nor at the follow-up treatment at 30-weeks post-procedure. The stable, long-term increase in breast size was 55 per cent (range 15–115%). The MRI visualizations of the breasts showed no edema, and confirmed the proportionate enlargement of the adipose and glandular components of the breast-tissue matrices. Furthermore, a statistically significant decrease in body weight occurred during the study, and self-esteem questionnaire scores improved from the initial-measure scores.[120]
Because external vacuum expansion of the recipient-site tissues permits injecting large-volume fat grafts (+300cc) to correct defects and enhance the bust, the histologic viability of the breast filler (adipocyte fat) and its volume must be monitored and maintained. The long-term, volume maintenance data reported in Breast Augmentation using Pre-expansion and Autologous Fat Transplantation: a Clinical Radiological Study (2010) indicate the technical effectiveness of external tissue expansion of the recipient site for a 25-patient study group, who had 46 breasts augmented with fat grafts. The indications included micromastia (underdevelopment), explantation deformity (empty implant pocket), and congenital defects (tuberous breast deformity, Poland’s syndrome).[121]
Pre-procedure, every patient used external vacuum expansion of the recipient-site tissues to create a breast-tissue matrix to be injected with autologous fat grafts of adipocyte tissue, refined via low G-force centrifugation. Pre- and post-procedure, the breast volumes were measured; the patients underwent pre-procedure and 6-month post-procedure MRI and 3-D volumetric imaging examinations. At 6-months post-procedure, each woman had a significant increase in breast volume, ranging 60–200 per cent, per the MRI (n=12) examinations. The size, form, and feel of the breasts was natural; post-procedure MRI examinations revealed no oil cysts or abnormality (neoplasm) in the fat-augmented breasts. Moreover, given the sensitive, biologic nature of breast tissue, periodic MRI and 3-D volumetric imaging examinations are required to monitor the breast-tissue viability and the maintenance of the large volume (+ 300cc) fat grafts.[121]
Indications
Non-implant breast augmentation with injections of autologous fat grafts (adipocyte tissue) is indicated for women requiring breast reconstruction, defect correction, and the æsthetic enhancement of the bust.
- breast reconstruction: post-mastectomy re-creation of the breast(s); trauma-damaged tissues (blunt, penetrating), disease (breast cancer), and explantation deformity (empty breast-implant socket).
- congenital defect correction": micromastia, tuberous breast deformity, Poland’s syndrome, et cetera.
- primary augmentation: the aesthetic enhancement (contouring) of the size, form, and feel of the breasts.
The operating room (OR) time of breast reconstruction, congenital defect correction, and primary breast augmentation procedures is determined by the indications to be treated.
Procedures
- Post-mastectomy surgical reconstruction
Surgical post-mastectomy breast reconstruction requires general anaesthesia, cuts the chest muscles, produces new scars, and requires a long post-surgical recovery for the patient. The surgical emplacement of breast implant devices (saline or silicone) introduces a foreign object to the patient’s body (see capsular contracture). The TRAM flap (Transverse Rectus Abdominis Myocutaneous flap) procedure reconstructs the breast using an autologous flap of abdominal, cutaneous, and muscle tissues. The latissimus myocutaneous flap employs skin fat and muscle harvested from the back, and a breast implant. The DIEP flap (Deep Inferior Epigastric Perforators) procedure uses an autologous flap of abdominal skin and fat tissue.[122]
- Post-mastectomy fat graft reconstruction
The reconstruction of the breast(s) with grafts of autologous fat is a non-implant alternative to further surgery after a breast cancer surgery, be it a lumpectomy or a breast removal—simple (total) mastectomy, radical mastectomy, modified radical mastectomy, skin-sparing mastectomy, and subcutaneous (nipple-sparing) mastectomy. The breast is reconstructed by first applying external tissue expansion to the recipient-site tissues (adipose, glandular) to create a breast-tissue matrix that can be injected with autologous fat grafts (adipocyte tissue); the reconstructed breast has a natural form, look, and feel, and is generally sensate throughout and in the nipple-areola complex (NAC).[122] The reconstruction of breasts with fat grafts requires a three-month treatment period—begun after 3–5 weeks of external vacuum expansion of the recipient-site tissues. The autologous breast-filler fat is harvested by liposuction from the patient’s body (buttocks, thighs, abdomen), is refined and then is injected (grafted) to the breast-tissue matrices (recipient sites), where the fat will thrive.
One method of non-implant breast reconstruction is initiated at the concluding steps of the breast cancer surgery, wherein the oncological surgeon is joined by the reconstructive plastic surgeon, who immediately begins harvesting, refining, and seeding (injecting) fat grafts to the post-mastectomy recipient site. After that initial post-mastectomy fat-graft seeding in the operating room, the patient leaves hospital with a slight breast mound that has been seeded to become the foundation tissue matrix for the breast reconstruction. Then, after 3–5 weeks of continual external vacuum expansion of the breast mound (seeded recipient-site)—to promote the histologic regeneration of the extant tissues (fat, glandular) via increased blood circulation to the mastectomy scar (suture site)—the patient formally undergoes the first fat-grafting session for the reconstruction of her breasts. The external vacuum expansion of the breast mound created an adequate, vascularised, breast-tissue matrix to which the autologous fat is injected; and, per the patient, such reconstruction affords almost-normal sensation throughout the breast and the nipple-areola complex. Patient recovery from non-surgical fat graft breast reconstruction permits her to resume normal life activities at 3-days post-procedure.[122]
- Tissue engineering
- I. the breast mound
The breast-tissue matrix consists of engineered tissues of complex, implanted, biocompatible scaffolds seeded with the appropriate cells. The in-situ creation of a tissue matrix in the breast mound is begun with the external vacuum expansion of the mastectomy defect tissues (recipient site), for subsequent seeding (injecting) with autologous fat grafts of adipocyte tissue. A 2010 study reported that serial fat-grafting to a pre-expanded recipient site achieved (with a few 2-mm incisions and minimally invasive blunt-cannula injection procedures), a non-implant outcome equivalent to a surgical breast reconstrcution by autologous-flap procedure. Technically, the external vacuum expansion of the recipient-site tissues created a skin envelope as it stretched the mastectomy scar, and so generated a fertile breast-tissue matrix to which were injected large-volume fat grafts (150–600 ml) to create a breast of natural form, look, and feel.[123]
The fat graft breast reconstructions for 33 women (47 breasts, 14 irradiated), whose clinical statuses ranged from zero days to 30 years post-mastectomy, began with the pre-expansion of the breast mound (recipient site) with an external vacuum tissue-expander for 10 hours daily, for 10–30 days before the first grafting of autologous fat. The breast mound expansion was adequate when the mastectomy scar tissues stretched to create a 200–300 ml recipient matrix (skin envelope), that received a fat-suspension volume of 150–600 ml in each grafting session.[123]
At one week post-procedure, the patients resumed using the external vacuum tissue-expander for 10 hours daily, until the next fat grafting session; 2–5 outpatient procedures, 6–16 weeks apart, were required until the plastic surgeon and the patient were satisfied with the volume, form, and feel of the reconstructed breasts. The follow-up mammogram and MRI examinations found neither defects (necrosis) nor abnormalities (neoplasms). At six months post-procedure, the reconstructed breasts had a natural form, look, and feel, and the stable breast-volumes ranged 300–600 ml per breast. The post-procedure mammographies indicated normal, fatty breasts with well-vascularized fat, and few, scattered, benign oil cysts. The occurred complications included pneumothorax and transient cysts.[123]
- II. Explantation deformity
The autologous fat graft replacement of breast implants (saline and silicone) resolves medical complications such as: capsular contracture, implant shell rupture, filler leakage (silent rupture), device deflation, and silicone-induced granulomas, which are medical conditions usually requiring re-operation and explantation (breast implant removal). The patient then has the option of surgical or non-implant breast corrections, either replacement of the explanted breast implants or fat-graft breast augmentation. Moreover, because fat grafts are biologically sensitive, they cannot survive in the empty implantation pocket, instead, they are injected to and diffused within the breast-tissue matrix (recipient site), replacing approximately 50% of the volume of the removed implant—as permanent breast augmentation. The outcome of the explantation correction is a bust of natural appearance; breasts of volume, form, and feel, that—although approximately 50% smaller than the explanted breast size—are larger than the original breast size, pre-procedure.[124]
- III. Breast augmentation
The outcome of a breast augmentation with fat-graft injections depends upon proper patient selection, preparation, and correct technique for recipient site expansion, and the harvesting, refining, and injecting of the autologous breast-filler fat. Technical success follows the adequate external vacuum expansion of the recipient-site tissues (matrix) before the injection of large-volume grafts (220–650 cc) of autologous fat to the breasts. After harvesting by liposuction, the breast-filler fat was obtained by low G-force syringe centrifugation of the harvested fat to separate it, by density, from the crystalloid component. The refined breast filler then was injected to the pre-expanded recipient site; post-procedure, the patient resumed continual vacuum expansion therapy upon the injected breast, until the next fat grafting session. The mean operating room (OR) time was 2-hours, and there occurred no incidences of infection, cysts, seroma, hematoma, or tissue necrosis.[121]
The breast-volume data reported in Breast Augmentation with Autologous Fat Grafting: A Clinical Radiological Study (2010) indicated a mean increase of 1.2 times the initial breast volume, at six months post-procedure. In a two-year period, 25 patients underwent breast augmentation by fat graft injection; at three weeks pre-procedure, before the fat grafting to the breast-tissue matrix (recipient site), the patients were photographed, and examined via intravenous contrast MRI or 3-D volumetric imaging, or both. The breast-filler fat was harvested by liposuction (abdomen, buttocks, thighs), and yielded fat-graft volumes of 220–650 cm3 per breast. At sex months post-procedure, the follow-up treatment included photographs, intravenous contrast MRI or 3-D volumetric imaging, or both. Each woman had an increased breast volume of 250 cm3 per breast, a mean volume increase confirmed by quantitative MRI analysis. The mean increase in breast volume was 1.2 times the initial breast volume measurements; the statistical difference between the pre-procedure and the six-month post-procedure breast volumes was (P< 00.0000007); the percentage increase basis of the breast volume was 60–80% of the initial, pre-procedure breast volume.[121]
Complications and limitations
- Medical complications
In every surgical and non-surgical procedure, the risk of medical complications exists before, during, and after a procedure, and, given the sensitive biological nature of breast tissues (adipocyte, glandular), this is especially true in the case of fat graft breast augmentation. Despite its relative technical simplicity, the injection (grafting) technique for breast augmentation is accompanied by post-procedure complications—fat necrosis, calcification, and sclerotic nodules—which directly influence the technical efficacy of the procedure, and of achieving a successful outcome. The Chinese study Breast Augmentation by Autologous Fat-injection Grafting: Management and Clinical analysis of Complications (2009), reported that the incidence of medical complications is reduced with strict control of the injection-rate (cm3/min) of the breast-filler volume being administered, and by diffusing the fat-grafts in layers to allow their even distribution within the breast tissue matrix. The complications occurred to the 17-patient group were identified and located with 3-D volumetric and MRI visualizations of the breast tissues and of any sclerotic lesions and abnormal tissue masses (malignant neoplasm). According to the characteristics of the defect or abnormality, the sclerotic lesion was excised and liquefied fat was aspirated; the excised samples indicated biological changes in the intramammary fat grafts—fat necrosis, calcification, hyalinization, and fibroplasia.[125]
The complications associated with injecting fat grafts to augment the breasts are like, but less severe, than the medical complications associated with other types of breast procedure. Technically, the use of minuscule (2-mm) incisions and blunt-cannula injection much reduce the incidence of damaging the underlying breast structures (milk ducts, blood vessels, nerves). Injected fat-tissue grafts that are not perfused among the tissues can die, and result in necrotic cysts and eventual calcifications—medical complications common to breast procedures. Nevertheless, a contoured abdomen for the patient is an additional benefit derived from the liposuction harvesting of the adipocyte tissue injected to the breasts. (see abdominoplasty)
- Technical limitations
When the patient’s body has insufficient adipocyte tissue to harvest as injectable breast filler, a combination of fat grafting and breast implants might provide the desired outcome. Although non-surgical breast augmentation with fat graft injections is not associated with implant-related medical complications (filler leakage, deflation, visibility, palpability, capsular contracture), the achievable breast volumes are physically limited; the large-volume, global bust augmentations realised with breast implants are not possible with the method of structural fat grafting. Global breast augmentation contrasts with the controlled breast augmentation of fat-graft injection, in the degree of control that the plastic surgeon has in achieving the desired breast contour and volume. The controlled augmentation is realised by infiltrating and diffusing the fat grafts throughout the breast; and it is feather-layered into the adjacent pectoral areas until achieving the desired outcome of breast volume and contour. Nonetheless, the physical fullness-of-breast achieved with injected fat-grafts does not visually translate into the type of buxom fullness achieved with breast implants; hence, patients who had plentiful fat-tissue to harvest attained a maximum breast augmentation of one brassiėre cup-size in one session of fat grafting to the breast.[110]
- Breast cancer
- Detection
A contemporary woman’s life-time probability of developing breast cancer is approximately one in seven;[126] yet there is no causal evidence that fat grafting to the breast might be more conducive to breast cancer than are other breast procedures; because incidences of fat tissue necrosis and calcification occur in every such procedure: breast biopsy, implantation, radiation therapy, breast reduction, breast reconstruction, and liposuction of the breast. Nonetheless, detecting breast cancer is primary, and calcification incidence is secondary; thus, the patient is counselled to learn self-palpation of the breast and to undergo periodic mammographic examinations. Although the mammogram is the superior diagnostic technique for distinguishing among cancerous and benign lesions to the breast, any questionable lesion can be visualized ultrasonically and magnetically (MRI); biopsy follows any clinically suspicious lesion or indeterminate abnormality appeared in a radiograph.[110]
- Therapy
Breast augmentation via autologous fat grafts allows the oncological breast surgeon to consider conservative breast surgery procedures that usually are precluded by the presence of alloplastic breast implants, e.g. lumpectomy, if cancer is detected in an implant-augmented breast. In previously augmented patients, aesthetic outcomes cannot be ensured without removing the implant and performing mastectomy.[127][128] Moreover, radiotherapy treatment is critical to reducing cancerous recurrence and to the maximal conservation of breast tissue; yet, ironically, radiotherapy of an implant-augmented breast much increases the incidence of medical complications—capsular contracture, infection, extrusion, and poor cosmetic outcome.[110]
- Post-cancer breast reconstruction
After mastectomy, surgical breast reconstruction with autogenous skin flaps and with breast implants can produce subtle deformities and deficiencies resultant from such global breast augmentation, thus the breast reconstruction is incomplete. In which case, fat graft injection can provide the missing coverage and fullness, and might relax the breast capsule. The fat can be injected as either large grafts or as small grafts, as required to correct difficult axillary deficiencies, improper breast contour, visible implant edges, capsular contracture, and tissue damage consequent to radiation therapy.[110]
Breast auto augmentation
The breast auto augmentation technique is used to provide fullness to the breast where it is needed - above the nipple - without the use of a breast implant. The gland is moved from the lower part of the breast to the upper area. It is kept attached at its lower end to preserve the blood supply. Once the skin is tightened, the finished contour looks like a breast with an implant.
Technique
Breast auto augmentation using the inferior portion of the breast has been described by Graf et al.,[129] using a weaving technique through the pectoralis major muscle. The technique of using a posterior parenchymal pedicle as an auto augmentation combined with a vertical mastopexy has also been described by Botti.[130] In that technique, the periareolar (around the areola) skin excision was designed according to the Lejour [131] pattern. The breast auto augmentation technique described by Kirwan [132] uses a posteriorly based dermoglandular flap as an augmentation of the superior hemisphere of the breast combined with a periareolar mastopexy and vertical mastopexy. The advantages of combining a periareolar mastopexy are the reduction of the length of the vertical scar and the prevention of areolar distortion.[133] The periareolar mastopexy is used so that the vertical excess skin can be captured in the larger periareolar skin excision, limiting the vertical skin excision. In addition, the periareolar suture stabilizes the circular shape of the areola, thereby preventing areolar distortion and traction into the vertical closure, and avoiding tension and compromised vascularity of the areola.
Outcome
Kirwan stated that this new procedure could benefit at least 20% of candidates for breast augmentation.[134] As with most breast surgery, recovery from Breast Auto-Augmentation necessitates undertaking only light chores in the first week and limited activities for another two weeks, with a return to normal lifestyle after four weeks. Compared to breast augmentation with implants, there is no cutting or displacement of the pectoralis major muscle.
Because of the absence of muscle involvement recovery is less painful and more rapid with less limitation on exercises. There is no deformation of the breasts when activating the chest muscles.
Thailand Breast Slap
The Thailand Breast Slap is a non-surgical method of breast augmentation endorsed by the Thai government as an alternative to surgical breast augmentation with breast implants. The Thai government enrolled more than 20 women in publicly funded courses for the teaching of the technique; nonetheless, beyond Thailand, the technique is not endorsed by the mainstream medical community. Despite the promising results of a six-month study of the therapeutic effectiveness of the technique, the research physician recommended to the participant women that they also contribute to augmenting their busts by gaining weight.[135]
References
- ↑ Cell-assisted Lipotransfer for Cosmetic Breast Augmentation: Supportive Use of Adipose-Derived Stem/Stromal Cells (2007) Yoshimura, K.; Sato, K.; Aoi, N.; Kurita, M.; Hirohi, T.; Harii, K. (2007). "Cell-Assisted Lipotransfer for Cosmetic Breast Augmentation: Supportive Use of Adipose-Derived Stem/Stromal Cells". Aesthetic Plastic Surgery 32 (1): 48–55; discussion 56–7. doi:10.1007/s00266-007-9019-4. PMC 2175019. PMID 17763894.
- ↑ Stevens WG, Hirsch EM, Stoker DA, Cohen R. (2006). "In vitro Deflation of Pre-filled Saline Breast Implants". Plastic Reconstruction Surgery 118 (2): 347–349. doi:10.1097/01.prs.0000227674.65284.80. PMID 16874200.
- ↑ Arion HG (1965). "Retromammary Prosthesis". C R Societé Française de Gynécologie 5.
- ↑ Eisenberg, TS (2009). "Silicone Gel Implants Are Back — So What?". American Journal of Cosmetic Surgery 26: 5–7.
- ↑ Cronin TD, Gerow FJ (1963). "Augmentation Mammaplasty: A New "natural feel" Prosthesis". Excerpta Medica International Congress Series 66: 41.
- ↑ Luu HM, Hutter JC, Bushar HF (1998). "A Physiologically based Pharmacokinetic Model for 2,4-toluenediamine Leached from Polyurethane foam-covered Breast Implants". Environ Health Perspect 106 (7): 393–400. doi:10.2307/3434066. JSTOR 3434066. PMC 1533137. PMID 9637796.
- ↑ Hester TR Jr, Tebbetts JB, Maxwell GP (2001). "The Polyurethane-covered Mammary Prosthesis: Facts and Fiction (II): A Look Back and a "peek" Ahead". Clinical Plastic Surgery 28 (3): 579–86. PMID 11471963.
- ↑ Brown, M. H.; Shenker, R.; Silver, S. A. (2005). "Cohesive silicone gel breast implants in aesthetic and reconstructive breast surgery". Plastic and reconstructive surgery 116 (3): 768–779; discussion 779–1. doi:10.1097/01.prs.0000176259.66948.e7. PMID 16141814.
- ↑ Fruhstorfer, B. H.; Hodgson, E. L.; Malata, C. M. (2004). "Early experience with an anatomical soft cohesive silicone gel prosthesis in cosmetic and reconstructive breast implant surgery". Annals of plastic surgery 53 (6): 536–542. doi:10.1097/01.sap.0000134508.43550.6f. PMID 15602249.
- ↑ Hedén, P.; Jernbeck, J.; Hober, M. (2001). "Breast augmentation with anatomical cohesive gel implants: The world's largest current experience". Clinics in plastic surgery 28 (3): 531–552. PMID 11471959.
- ↑ Tortora, Gerard J. Introduction to the Human Body, Fifth Edition. John Wiley & Sons, Inc.: New York, 2001. p. 560.
- ↑ Ramsay DT, Kent JC, Hartmann RA, Hartmann PE (2005). "Anatomy of the Lactating Human Breast Redefined with Ultrasound Imaging". Journal of Anatomy 206 (6): 525–534. doi:10.1111/j.1469-7580.2005.00417.x. PMC 1571528. PMID 15960763.
- ↑ Berlin, C. M. (1994). "Silicone Breast Implants and Breast-feeding". Pediatrics 94 (4 Pt 1): 546–549. PMID 7936870.
- ↑ Berlin, Cheston M., Jr. Silicone Breast Implants and Breastfeeding, Hershey Medical Center, Hershey, Pennsylvania; from Breastfeeding Abstracts. February 1996, Volume 15, Number 3, pp. 17–18.
- ↑ Breastfeeding after Breast Surgery, La Leche League (2009-09-05).
- ↑ Breastfeeding and Breast Implants, Selected Bibliography April 2003, LLLI Center for Breastfeeding Information.
- ↑ 17.0 17.1 Beam, Christopher (2009-12-11). Inorganic Milk: Can Kendra Wilkinson breast-feed her baby even though she has implants?, Slate.com.
- ↑ Brinton L, Brown S, Colton T, Burich M, Lubin J (2000). "Characteristics of a Population of Women with Breast Implants Compared with Women Seeking other Types of Plastic Surgery". Plastic Reconstructive Surgery 105 (3): 919–927. doi:10.1097/00006534-200003000-00014. PMID 10724251.
- ↑ Jacobsen, P. H.; Hölmich, L. R.; McLaughlin, J. K.; Johansen, C.; Olsen, J. H.; Kjøller, K.; Friis, S. (2004). "Mortality and Suicide Among Danish Women with Cosmetic Breast Implants". Archives of Internal Medicine 164 (22): 2450–2455. doi:10.1001/archinte.164.22.2450. PMID 15596635.
- ↑ Young, V. L.; Nemecek, J. R.; Nemecek, D. A. (1994). "The efficacy of breast augmentation: Breast size increase, patient satisfaction, and psychological effects". Plastic and reconstructive surgery 94 (7): 958–969. doi:10.1097/00006534-199412000-00009. PMID 7972484.
- ↑ Crerand, C. E.; Franklin, M. E.; Sarwer, D. B. (2006). "Body Dysmorphic Disorder and Cosmetic Surgery". Plastic and Reconstructive Surgery 118 (7): 167e–180e. doi:10.1097/01.prs.0000242500.28431.24. PMID 17102719.
- ↑ Sarwer, D. B.; Larossa, D.; Bartlett, S. P.; Low, D. W.; Bucky, L. P.; Whitaker, L. A. (2003). "Body Image Concerns of Breast Augmentation Patients". Plastic and Reconstructive Surgery 112 (1): 83–90. doi:10.1097/01.PRS.0000066005.07796.51. PMID 12832880.
- ↑ Chahraoui, K.; Danino, A.; Frachebois, C.; Clerc, A. S.; Malka, G. (2006). "Chirurgie esthétique et qualité de vie subjective avant et quatre mois après l'opération". Annales de Chirurgie Plastique Esthétique 51 (3): 207–210. doi:10.1016/j.anplas.2005.07.010. PMID 16181718.
- ↑ Cash, T. F.; Duel, L. A.; Perkins, L. L. (2002). "Women's psychosocial outcomes of breast augmentation with silicone gel-filled implants: A 2-year prospective study". Plastic and reconstructive surgery 109 (6): 2112–2121; discussion 2121–3. doi:10.1097/00006534-200205000-00049. PMID 11994621.
- ↑ Figueroa-Haas, C. L. (2007). "Effect of breast augmentation mammoplasty on self-esteem and sexuality: A quantitative analysis". Plastic surgical nursing : official journal of the American Society of Plastic and Reconstructive Surgical Nurses 27 (1): 16–36. doi:10.1097/01.PSN.0000264159.30505.c9. PMID 17356451.
- ↑ 26.0 26.1 26.2 "Important Information for Women About Breast Augmentation with Inamed Silicone Gel-Filled Implants" (PDF). 2006.
- ↑ Handel, N.; Cordray, T.; Gutierrez, J.; Jensen, J. A. (2006). "A Long-Term Study of Outcomes, Complications, and Patient Satisfaction with Breast Implants". Plastic and Reconstructive Surgery 117 (3): 757–767; discussion 767–72. doi:10.1097/01.prs.0000201457.00772.1d. PMID 16525261.
- ↑ They Need Bosoms, too – Women Weight Lifters, Cosmeticsurgery.com
- ↑ "Breast Implants Linked with Suicide in Study". Reuters. 2007-08-08.
- ↑ Manning, Anita (2007-08-06). "Breast Implants Linked to Higher Suicide Rates". USA Today. Retrieved 2010-04-26.
- ↑ Brinton, L. A.; Lubin, J. H.; Burich, M. C.; Colton, T.; Hoover, R. N. (2001). "Mortality among augmentation mammoplasty patients". Epidemiology (Cambridge, Mass.) 12 (3): 321–326. PMID 11337605.
- ↑ Koot, V. C. M.; Peeters, P. H.; Granath, F.; Grobbee, D. E.; Nyren, O. (2003). "Total and cause specific mortality among Swedish women with cosmetic breast implants: Prospective study". BMJ 326 (7388): 527–528. doi:10.1136/bmj.326.7388.527. PMC 150462. PMID 12623911.
- ↑ Pukkala, E.; Kulmala, I.; Hovi, S. L.; Hemminki, E.; Keskimäki, I.; Lipworth, L.; Boice, J. D.; McLaughlin, J. K.; McLaughlin, J. K. (2003). "Causes of Death Among Finnish Women with Cosmetic Breast Implants, 1971–2001". Annals of Plastic Surgery 51 (4): 339–342; discussion 342–4. doi:10.1097/01.sap.0000080407.97677.A5. PMID 14520056.
- ↑ 34.0 34.1 Villenueve PJ et al. (June 2006). "Mortality among Canadian Women with Cosmetic Breast Implants". American Journal of Epidemiology 164 (4): 334–341. doi:10.1093/aje/kwj214. PMID 16777929.
- ↑ Brinton, L. A.; Lubin, J. H.; Murray, M. C.; Colton, T.; Hoover, R. N. (2006). "Mortality Rates Among Augmentation Mammoplasty Patients". Epidemiology 17 (2): 162–169. doi:10.1097/01.ede.0000197056.84629.19. PMID 16477256.
- ↑ National Plastic Surgery Procedural Statistics, 2006. Arlington Heights, Illinois, American Society of Plastic Surgeons, 2007
- ↑ Nauert, Rick. (2007-03-23) Plastic Surgery Helps Self-Esteem | Psych Central News. Psychcentral.com. Retrieved on 2012-07-15.
- ↑ Kearney, Robert. "Breast Augmentation". Robert Kearney MD FACS. Retrieved 6 May 2012.
- ↑ Johnson, G. W.; Christ, J. E. (1993). "The endoscopic breast augmentation: The transumbilical insertion of saline-filled breast implants". Plastic and reconstructive surgery 92 (5): 801–808. PMID 8415961.
- ↑ Wallach, S. G. (2004). "Maximizing the Use of the Abdominoplasty Incision". Plastic and Reconstructive Surgery 113 (1): 411–417; discussion 417. doi:10.1097/01.PRS.0000091422.11191.1A. PMID 14707667.
- ↑ Graf RM et al. (2003). "Subfascial Breast Implant: A New Procedure". Plastic Reconstructive Surgery 111 (2): 904–908. doi:10.1097/01.PRS.0000041601.59651.15. PMID 12560720.
- ↑ Tebbetts JB (2004). "Does Fascia Provide Additional, Meaningful Coverage over a Breast Implant?". Plastic Reconstructive Surgery 113 (2): 777–779. doi:10.1097/01.PRS.0000104516.13465.96. PMID 14758271.
- ↑ Tebbetts T (2002). "A System for Breast Implant Selection Based on Patient Tissue Characteristics and Implant-soft tissue Dynamics". Plastic Reconstructive Surgery 109 (4): 1396–1409. doi:10.1097/00006534-200204010-00030. PMID 11964998.
- ↑ Pacik, P.; Nelson, C.; Werner, C. (2008). "Pain Control in Augmentation Mammaplasty: Safety and Efficacy of Indwelling Catheters in 644 Consecutive Patients". Aesthetic Surgery Journal 28 (3): 279–284. doi:10.1016/j.asj.2008.02.001. PMID 19083538.
- ↑ Pacik, P.; Nelson, C.; Werner, C. (2008). "Pain Control in Augmentation Mammaplasty Using Indwelling Catheters in 687 Consecutive Patients: Data Analysis". Aesthetic Surgery Journal 28 (6): 631–641. doi:10.1016/j.asj.2008.09.001. PMID 19083591.
- ↑ "Important Information for Augmentation Patients About Mentor MemoryGel Silicone Gel-Filled Breast Implants" (PDF). fda.gov. 2006-11-03. Retrieved 2007-05-04.
- ↑ "Saline-Filled Breast Implant Surgery: Making An Informed Decision (Mentor Corporation)". FDA Breast Implant Consumer Handbook – 2004. 2004-01-13. Retrieved 2007-05-04.
- ↑ FDA provides updated safety data on silicone gel-filled breast implants. Fda.gov (2011-06-22). Retrieved on 2012-07-15.
- ↑ Brown SL, Middleton MS, Berg WA, Soo MS, Pennello G (2000). "Prevalence of Rupture of Silicone gel Breast Implants Revealed on MR Imaging in a Population of Women in Birmingham, Alabama". American Journal of Roentgenology 175 (4): 1057–1064. PMID 11000165.
- ↑ Walker PS et al. (2009). "Natrelle Saline-filled Breast Implants: a Prospective 10-year Study". Aesthetic Surgery Journal 29 (1): 19–25. doi:10.1016/j.asj.2008.10.001. PMID 19233001.
- ↑ Holmich LR et al. (2004). "Untreated Silicone Breast Implant Rupture". Plastic Reconstructive Surgery. 114 (1): 204–214. doi:10.1097/01.PRS.0000128821.87939.B5. PMID 15220594.
- ↑ Katzin, William E, Ceneno, Jose A, Feng, Lu-Jean (2001). "Pathology of Lymph Nodes From Patients With Breast Implants: A Histologic and Spectroscopic Evaluation" (—Scholar search). American Journal of Surgical Pathology 29 (4): 506–11. PMID 15767806.
- ↑ "Study of Rupture of Silicone Gel-filled Breast Implants (MRI Component)". FDA Breast Implant Consumer Handbook - 2004. 2000-05-22. Retrieved 2007-05-04.
- ↑ 54.0 54.1 54.2 "Local Complications". FDA Breast Implant Consumer Handbook - 2004. 2004-06-08. Retrieved 2007-05-04.
- ↑ MRI of a ruptured silicone breast implant 2013-04-05
- ↑ Holmich LR et al. (2003). "Incidence of Silicone Breast Implant Rupture". Arch Surg. 138 (7): 801–806. doi:10.1001/archsurg.138.7.801. PMID 12860765.
- ↑ Heden P et al. (2006). "Prevalence of Rupture in Inamed Silicone Breast Implants". Plastic Reconstructive Surgery 118 (2): 303–308. doi:10.1097/01.prs.0000233471.58039.30. PMID 16874191.
- ↑ "FDA summary of clinical issues (MS Word document)".
- ↑ Cunningham, B et al. (2009). "Safety and effectiveness of Mentor's MemoryGel implants at 6 years". Plastic Reconstructive Surgery 33 (3): 440–444. doi:10.1007/s00266-009-9364-6. PMID 19437068.
- ↑ Heden P et al. (2006). "Style 410 Cohesive Silicone Breast Implants: Safety and Effectiveness at 5 to 9 years after Implantation". Plastic Reconstructive Surgery 118 (6): 1281–1287. doi:10.1097/01.prs.0000239457.17721.5d. PMID 17051096.
- ↑ Holmich LR, Fryzek JP, Kjoller K, Breiting VB, Jorgensen A, Krag C, McLaughlin JK (2005). "The Diagnosis of Silicone Breast-implant Rupture: Clinical Findings Compared with Findings at Magnetic Resonance Imaging". Annals of Plastic Surgery 54 (6): 583–589. doi:10.1097/01.sap.0000164470.76432.4f. PMID 15900139.
- ↑ 62.0 62.1 "Expert Advisory Panel on Breast Implants: Record of Proceedings". HealthCanada. 2005-09-29. Retrieved 2007-05-04.
- ↑ Song JW, Kim HM, Bellfi LT, Chung KC (2011). "The Effect of Study design Biases on the Diagnostic Accuracy of Magnetic Resonance Imaging for Detecting Silicone Breast Implant Ruptures: a Meta-analysis". Plastic and Reconstructive Surgery 127 (3): 1029–1044. doi:10.1097/PRS.0b013e3182043630. PMC 3080104. PMID 21364405.
- ↑ independent.co.uk - Breast implants safe, but not for life: US experts
- ↑ Barnsley GP; Sigurdson, LJ; Barnsley, SE (2006). "Textured surface Breast Implants in the Prevention of Capsular Contracture among Breast Augmentation Patients: a Meta-analysis of Randomized Controlled Trials". Plastic Reconstructive Surgery 117 (7): 2182–2190. doi:10.1097/01.prs.0000218184.47372.d5. PMID 16772915.
- ↑ Wong CH, Samuel M, Tan BK, Song C. (2006). "Capsular Contracture in Subglandular Breast Augmentation with Textured versus Sooth Breast Implants: a Systematic Review". Plastic Reconstructive Surgery 118 (5): 1224–1236. doi:10.1097/01.prs.0000237013.50283.d2. PMID 17016195.
- ↑ Handel N et al. (may 2006). "Long-term safety and efficacy of polyurethane foam-covered breast implants". Journal of Aesthetic Surgery 26 (3): 265–274. doi:10.1016/j.asj.2006.04.001. PMID 19338905.
- ↑ Mladick RA (1993). ""No-touch" submuscular saline breast augmentation technique". Journal of Aesthetic Surgery 17 (3): 183–192. doi:10.1007/BF00636260. PMID 8213311.
- ↑ Adams WP jr.; Rios, Jose L.; Smith, Sharon J. (2006). "Enhancing Patient Outcomes in Aesthetic and Reconstructive Breast Surgery using Triple Antibiotic Breast Irrigation: Six-year Prospective Clinical Study". Plastic Reconstructive Surgery 117 (1): 30–6. doi:10.1097/01.prs.0000185671.51993.7e. PMID 16404244.
- ↑ Planas J; Cervelli, V; Planas, G (2001). "Five-year experience on ultrasonic treatment of breast contractures". Aesthetic Plastic Surgery 25 (2): 89–93. doi:10.1007/s002660010102. PMID 11349308.
- ↑ Schlesinger SL, wt al (2002). "Zafirlukast (Accolate): A new treatment for capsular contracture". Aesthetic Plast Surg. 22 (4): 329–36.
- ↑ Scuderi N et al. (2006). "The effects of zafirlukast on capsular contracture: preliminary report". Aesthetic Plast Surg. 30 (5): 513–520. doi:10.1007/s00266-006-0038-3. PMID 16977359.
- ↑ Silver H (1982). "Reduction of capsular contracture with two-stage augmentation mammaplasty and pulsed electromagnetic energy (Diapulse therapy)". Plastic Reconstructive Surgery 69 (5): 802–805. doi:10.1097/00006534-198205000-00013. PMID 7071225.
- ↑ Tebbetts, J. B. (2004). ""Out points" criteria for breast implant removal without replacement and criteria to minimize reoperations following breast augmentation". Plastic and reconstructive surgery 114 (5): 1258–1262. PMID 15457046.
- ↑ Tebbetts, J. B. (2006). "Achieving a Zero Percent Reoperation Rate at 3 Years in a 50-Consecutive-Case Augmentation Mammaplasty Premarket Approval Study". Plastic and Reconstructive Surgery 118 (6): 1453–1457. doi:10.1097/01.prs.0000239602.99867.07. PMID 17051118.
- ↑ Therapeutic Goods Administration (2001). Breast Implant Information Booklet (PDF) (4th ed.). Australian Government. ISBN 0-642-73579-4.
- ↑ European Committee on Quality Assurance and Medical Devices in Plastic Surgery (2000-06-23). "Consensus Declaration on Breast Implants" (PDF). Archived from the original on December 30, 2006. Retrieved 2007-05-04.
- ↑ "Silicone Gel Breast Implant Report Launched - No Epidemiological Evidence For Link With Connective Tissue Disease - Independent Review Group". 1998-07-13. Retrieved 2007-05-04.
- ↑ Breiting VB, Holmich LR, Brandt B, Fryzek JP, Wolthers MS, Kjoller K, McLaughlin JK, Wiik A, Friis S (2004). "Long-term Health Status of Danish Women with Silicone Breast Implants". Plastic and Reconstructive Surgery 114 (1): 217–226. doi:10.1097/01.PRS.0000128823.77637.8A. PMID 15220596.
- ↑ Kjoller K, Holmich LR, Fryzek JP, Jacobsen PH, Friis S, McLaughlin JK, Lipworth L, Henriksen TF, Hoier-Madsen M, Wiik A, Olsen JH (2004). "Self-reported musculoskeletal symptoms among Danish women with cosmetic breast implants". Annals of Plastic Surgery 52 (1): 1–7. doi:10.1097/01.sap.0000101930.75241.55. PMID 14676691.
- ↑ Fryzek JP, Holmich L, McLaughlin JK, Lipworth L, Tarone RE, Henriksen T, Kjoller K, Friis S (2007). "A Nationwide Study of Connective Tissue Disease and Other Rheumatic Conditions Among Danish Women With Long-Term Cosmetic Breast Implantation". Annals of Epidemiology 17 (5): 374–379. doi:10.1016/j.annepidem.2006.11.001. PMID 17321754.
- ↑ Brinton LA, Lubin JH, Murray MC, Colton T, Hoover RN (2006). "Mortality Rates Among Augmentation Mammoplasty patients: an update". Epidemiology 17 (2): 162–9. doi:10.1097/01.ede.0000197056.84629.19. PMID 16477256.
- ↑ McLaughlin JK, Lipworth L, Fryzek JP, Ye W, Tarone RE, Nyren O (2006). "Long-term Cancer Risk Among Swedish Women with Cosmetic Breast Implants: an Update of a Nationwide Study". J Natl Cancer Inst. 98 (8): 557–60. doi:10.1093/jnci/djj134. PMID 16622125.
- ↑ Brown SL, Pennello G, Berg WA, Soo MS, Middleton MS (2001). "Silicone gel Breast Implant Rupture, Extracapsular Silicone, and Health Status in a Population of Women". Journal of Rheumatology 28 (5): 996–1003. PMID 11361228.
- ↑ Lipworth L, Tarone RE, McLaughlin JK. (2004). "Breast Implants and Fibromyalgia: a Review of the Epidemiologic Evidence". Annals of Plastic Surgery 52 (3): 284–287. doi:10.1097/01.sap.0000116024.18713.28. PMID 15156983.
- ↑ "Diseases". FDA Breast Implant Consumer Handbook - 2004. 2004-06-08. Retrieved 2007-05-04.
- ↑ Lipworth L, Holmich LR, McLaughlin JK. (2011). "Silicone Breast implants and Connective tissue Disease: No Association". Semin Immunopathol 33 (3): 287–294. doi:10.1007/s00281-010-0238-4. PMID 21369953.
- ↑ 88.0 88.1 Rinzler, Carol Ann (2009) The encyclopedia of Cosmetic and Plastic Surgery New York:Facts on File, p.23.
- ↑ Arepelli S et al. (2002). "Allergic reactions to platinum in silicone breast implants". J Long-Term Effects Medical Implants 12 (4): 299–306. PMID 12627791.
- ↑ Lykissa E.D. and Maharaj S.V.M. (April 2006). "Total Platinum Concentration and Platinum Oxidation States in Body Fluids, Tissue, and Explants from Women Exposed to Silicone and Saline Breast Implants by IC-ICPMS". Analytical Chemistry 78 (9): 2925–2933. doi:10.1021/ac0514016. PMID 16642977. (due publication May 2006). Retrieved 2006-04-06.
- ↑ "Dubious Breast Implant Study: Doubts now surround study claiming to have found high levels of platinum in women with silicone breast". July 31, 2006.
- ↑ "FDA Backgrounder on Platinum in Silicone Breast Implants". Food and Drug Administration.
- ↑ Fischer G. Surgical Treatment of Cellulitis (presentation) Third Congress of the International Academy of Cosmetic Surgery, Rome, 31 May 1975
- ↑ Fischer G. First Surgical Treatment for Modelling the Body’s Cellulite with Three 5-mm incisions. Bulletin of the International Academy of Cosmetic Surgery 1976; 2:35–37
- ↑ Fischer A., Fischer G. (1977). "Revised Technique for Cellulite fat reduction in Riding Breeches deformity". Bulletin of the International Academy of Cosmetic Surgery 2 (4): 40–43.
- ↑ Schiffman, p. 3.
- ↑ Bircoll M. Autologous Fat Transplantation (presentation) The Asian Congress of Plastic Surgery, February 1982
- ↑ Bircoll MJ (1984) New Frontiers in Suction Lipectomy (presentation) Second Asian Congress of Plastic Surgery, Pattiya, Thailand, February
- ↑ Krulig E. (1987). "Lipo-injection". American Journal of Cosmetic Surgery 4 (2): 123–129.
- ↑ Schiffman, p. 4.
- ↑ Newman J, Levin J. (1987). "Facial Lipo-transplant Surgery". American Journal of Cosmetic Surgery 4 (2): 131–140.
- ↑ Agris J. (1987). "Autologous Fat Transplantation: A Three-year Study". American Journal of Cosmetic Surgery 4 (2): 95–102.
- ↑ Schiffman, p. 226.
- ↑ Pierrefeu-Lagrange, A. C., Delay, E., Guerin, N., et al. Radiological Evaluation of Breasts Reconstructed with Lipo-modeling (in French). Annales de Chirurgie Plastique Esthétique 51:18, 2005
- ↑ Zocchi, M. L., Zuliani, F., Nava, M., et al. Bicompartmental Breast Lipostructuring, presentation to the 7th International Congress of Aesthetic Medicine, Milan, 13–15 October 2005.
- ↑ Rigotti, G., Marchi, A., Galiè, M., et al. Clinical Treatment of Radiotherapy Tissue Damages by Lipoaspirates Transplant: A Healing Process Mediated by Adipose-derived Stem cells (ASCS). Plastic and Reconstructive Surgery (accepted for publication)
- ↑ Holle, J. Lipofilling in Rhinoplasty and Breast Augmentation, a presentation to the American Alpine Workshop in Plastic Surgery, at the 17th Annual Meeting, Sun Valley, Idaho, 12–17 February 2006
- ↑ Massiha, H. Scar-tissue Flaps for the Correction of Post-implant Breast Rippling. Annals of Plastic Surgery 48:505, 2002
- ↑ Baruffaldi-Preis, F. La correzione delle depressioni: Esiti cicatriziali e rippling (presentatio) 30th Anniversary Course of the Foundation of G. Sanvenero Rosselli, Milan, Italy, 16 September 2005
- ↑ 110.0 110.1 110.2 110.3 110.4 110.5 110.6 Coleman, S. R.; Saboeiro, A. P. (2007). "Fat Grafting to the Breast Revisited: Safety and Efficacy". Plastic and Reconstructive Surgery 119 (3): 775–785; discussion 785–7. doi:10.1097/01.prs.0000252001.59162.c9. PMID 17312477.
- ↑ Yoshimura, K.; Sato, K.; Aoi, N.; Kurita, M.; Hirohi, T.; Harii, K. (2007). "Cell-Assisted Lipotransfer for Cosmetic Breast Augmentation: Supportive Use of Adipose-Derived Stem/Stromal Cells". Aesthetic Plastic Surgery 32 (1): 48–55; discussion 56–7. doi:10.1007/s00266-007-9019-4. PMC 2175019. PMID 17763894.
- ↑ Asken, S. (1987). "Autologous Fat Transplantation: Micro and Macro Techniques". American Journal of Cosmetic Surgery 4 (2): 111–121.
- ↑ Toledo, L. S. (1991). "Syringe liposculpture: A two-year experience". Aesthetic plastic surgery 15 (4): 321–326. PMID 1950806.
- ↑ Uebel, C.O. (1992) "Facial Sculpture with Centrifuged fat Collagen", pp. 749–752 in Hinder, V.T. (Ed.) Plastic Surgery Vol. II. Amsterdam Excerpta Medica
- ↑ Schiffman, p. 5.
- ↑ Coleman, S. (2002). "Avoidance of arterial occlusion from injection of soft tissue fillers". Aesthetic Surgery Journal 22 (6): 555–557. doi:10.1067/maj.2002.129625. PMID 19332014.
- ↑ Guerney, C.E. Experimental Study of the Behavior of Free fat Transplants. Surgery 1938, 3:679–692
- ↑ Neuhof H. (1923) The Transplantation of Tissues New York:D. Appleton p. 74
- ↑ Rigotti G, Marchi A, Galiè M. et al. Clinical Treatment of Radiotherapy Tissue Damages by Lipoaspirates Transplant: a Healing Process Mediated by Adipose-derived stem cells (ASCS). Plastic and Reconstructive Surgery (accepted for publication).
- ↑ 120.0 120.1 Khouri, R. K.; Schlenz, I.; Murphy, B. J.; Baker, T. J. (2000). "Nonsurgical breast enlargement using an external soft-tissue expansion system". Plastic and reconstructive surgery 105 (7): 2500–2512; discussion 2512–4. PMID 10845308.
- ↑ 121.0 121.1 121.2 121.3 Del Vecchio, D. A.; Bucky, L. P. (2011). "Breast Augmentation Using Preexpansion and Autologous Fat Transplantation: A Clinical Radiographic Study". Plastic and Reconstructive Surgery 127 (6): 2441–2450. doi:10.1097/PRS.0b013e3182050a64. PMID 21311393.
- ↑ 122.0 122.1 122.2 Khouri RK (2010) Non-surgical breast reconstruction with autologous fat-grafts
- ↑ 123.0 123.1 123.2 Khouri RK, Cardoso E, Marchi A, Rigotti G. (2010) Tissue Engineering a Breast Mound by External expansion & Autologous fat Grafting. miamibreastcenter.com
- ↑ Khouri, R.K. (2010) Breast Implant Removal. miamibreastcenter.com
- ↑ Mu, D. L.; Luan, J.; Mu, L.; Xin, M. Q. (2009). "Breast Augmentation by Autologous Fat Injection Grafting". Annals of Plastic Surgery 63 (2): 124–127. doi:10.1097/SAP.0b013e318189a98a. PMID 19574890.
- ↑ Gloeckler Ries, L. A.; Reichman, M. E.; Lewis, D. R.; Hankey, B. F.; Edwards, B. K. (2003). "Cancer survival and incidence from the Surveillance, Epidemiology, and End Results (SEER) program". The oncologist 8 (6): 541–552. doi:10.1634/theoncologist.8-6-541. PMID 14657533.
- ↑ Karanas, Y. L.; Leong, D. S.; Da Lio, A.; Waldron, K.; Watson, J. P.; Chang, H.; Shaw, W. W. (2003). "Surgical Treatment of Breast Cancer in Previously Augmented Patients". Plastic and Reconstructive Surgery 111 (3): 1078–1083; discussion 1083–6. doi:10.1097/01.PRS.0000046667.56931.E1. PMID 12621177.
- ↑ Handel, N.; Lewinsky, B.; Jensen, J. A.; Silverstein, M. J. (1996). "Breast conservation therapy after augmentation mammaplasty: Is it appropriate?". Plastic and reconstructive surgery 98 (7): 1216–1224. PMID 8942907.
- ↑ Graf R, Reis de Araujo LR, Rippel R, Neto LG, Pace DT, Biggs T. Reduction mammaplasty and mastopexy using the vertical scar and thoracic wall flap technique. Aesthetic Plast Surg. 2003;27:6–12. [PubMed]
- ↑ Botti G. Vertical scar mammaplasty: Stable padding of the superior pole by means of posteriorly based pedicle autoprosthesis. Aesthetic Surg J. 1999;19:116–23.
- ↑ Lejour M. Vertical mammaplasty: Early complications after 250 personal consecutive cases. Plast Reconstr Surg. 1999;104:764–70. [PubMed]
- ↑ Kirwan L. Breast autoaugmentation, US National Library of Medicine National Institutes of Health
- ↑ Kirwan L (2009-12-18). "Breast autoaugmentation". Pulsus.com. Retrieved 2013-11-23.
- ↑ Posted by Dorene 12.05.10. "Laurence Kirwan MD, FRCS and FACS in the US and UK". Beautyinthebag.com. Retrieved 2013-11-23.
- ↑ McGirk, Jan (2003-02-22). "Thailand sponsors slapping to enhance breast size". The Independent (London).
Bibliography
- Schiffman MA (2010). Autologous Fat Transfer: Art, Science, and Clinical Practice. Berlin, Heidelberg: Springer. ISBN 3642004725.
