Bipolar disorder
| Bipolar disorder | |
|---|---|
| Classification and external resources | |
 Bipolar disorder is characterized by transitions between depression and mania | |
| ICD-10 | F31 |
| ICD-9 | 296.0, 296.1, 296.4, 296.5, 296.6, 296.7, 296.8 |
| OMIM | 125480 309200 |
| DiseasesDB | 7812 |
| MedlinePlus | 000926 |
| eMedicine | med/229 |
| MeSH | D001714 |
Bipolar disorder (also known as bipolar affective disorder, manic-depressive disorder, or manic depression) is a mental illness characterized by episodes of an elevated or agitated mood known as mania, alternating with episodes of depression.
Mania can occur with different levels of severity. At milder levels of mania, known as hypomania, individuals appear energetic, excitable, and may be highly productive. As mania becomes more severe, individuals begin to behave erratically and impulsively, often making poor decisions due to unrealistic ideas about the future, and sleep very little. At the most severe level, individuals can experience very distorted beliefs about the world known as psychosis.
Individuals who experience manic episodes also commonly experience depressive episodes; some experience a mixed state in which features of both mania and depression are present at the same time. Manic and depressive episodes last from a few days to several months.
About 4% of people suffer from bipolar disorder. Prevalence is similar in men and women and, broadly, across different cultures and ethnic groups. Genetic factors contribute substantially to the likelihood of developing bipolar disorder, and environmental factors are also implicated. Bipolar disorder is often treated with mood stabilizing medications and psychotherapy. In serious cases, in which there is a risk of harm to oneself or others, involuntary commitment may be used. These cases generally involve severe manic episodes with dangerous behavior or depressive episodes with suicidal ideation. There are widespread problems with social stigma, stereotypes, and prejudice against individuals with a diagnosis of bipolar disorder. People with bipolar disorder exhibiting psychotic symptoms can sometimes be misdiagnosed as having schizophrenia.
The current term bipolar disorder is of fairly recent origin and refers to the cycling between high and low episodes (poles). The term "manic–depressive illness" or psychosis was coined by German psychiatrist Emil Kraepelin in the late nineteenth century, originally referring to all kinds of mood disorder. German psychiatrist Karl Leonhard split the classification in 1957, employing the terms unipolar disorder (major depressive disorder) and bipolar disorder.
Signs and symptoms
In bipolar disorder, people experience abnormally elevated (manic or hypomanic) mood states which interfere with the functions of ordinary life. Many people with bipolar disorder also experience periods of depressed mood, but this is not universal. There is no simple physiological test to confirm the disorder. Diagnosing bipolar disorder is often difficult, even for mental health professionals. In particular, it can be difficult to distinguish depression caused by bipolar disorder from pure unipolar depression.
The earlier the age of onset, the more likely the first few episodes are to be depressive.[1] Because a bipolar diagnosis requires a manic or hypomanic episode, many patients are initially diagnosed and treated as having major depression.[2]
Manic episodes
Mania is the defining feature of bipolar disorder. Mania is a distinct period of elevated or irritable mood, which can take the form of euphoria, and lasts for at least a week (less if hospitalization is required).[3] People with mania commonly experience an increase in energy and a decreased need for sleep, with many often getting as little as three or four hours of sleep per night. Some can go days without sleeping.[4] A manic person may exhibit pressured speech, with thoughts experienced as racing.[5] Attention span is low, and a person in a manic state may be easily distracted. Judgment may be impaired, and sufferers may go on spending sprees or engage in risky behavior that is not normal for them. Substance abuse is often engaged in. Their behavior may become aggressive, intolerant, or intrusive. They may feel out of control or unstoppable, or as if they have been "chosen" and are "on a special mission", or have other grandiose or delusional ideas. Sexual drive may increase. At more extreme levels, a person in a manic state can experience psychosis, or a break with reality, where thinking is affected along with mood.[6] This can occasionally lead to violent behaviors.[7] Some people in a manic state experience severe anxiety and are irritable (to the point of rage), while others are euphoric and grandiose. The severity of manic symptoms can be measured by rating scales such as the Altman Self-Rating Mania Scale[8] and clinician-based Young Mania Rating Scale.[9][10]
The onset of a manic episode is often foreshadowed by sleep disturbances. Mood changes, psychomotor and appetite changes, and an increase in anxiety can also occur up to three weeks before a manic episode develops.[11]
Hypomanic episodes
Hypomania is a mild to moderate level of elevated mood, characterized by optimism, pressure of speech and activity, and decreased need for sleep. Generally, hypomania does not inhibit functioning as mania does.[12] Many people with hypomania are actually more productive than usual, while manic individuals have difficulty completing tasks due to a shortened attention span. Some hypomanic people show increased creativity, although others demonstrate poor judgment and irritability. Many experience hypersexuality. Hypomanic people generally have increased energy and increased activity levels. They do not, however, have delusions or hallucinations.
Hypomania may feel good to the person who experiences it. Thus, even when family and friends recognize mood swings, the individual often will deny that anything is wrong.[13] What might be called a "hypomanic event", if not accompanied by depressive episodes, is often not deemed as problematic, unless the mood changes are uncontrollable, volatile or mercurial. If left untreated, an episode of hypomania can last anywhere from a few days to several years. Most commonly, symptoms continue for a few weeks to a few months.[14]
Depressive episodes
Signs and symptoms of the depressive phase of bipolar disorder include persistent feelings of sadness, anxiety, guilt, anger, isolation, or hopelessness; disturbances in sleep and appetite; fatigue and loss of interest in usually enjoyable activities; problems concentrating; loneliness, self-loathing, apathy or indifference; depersonalization; loss of interest in sexual activity; shyness or social anxiety; irritability, chronic pain (with or without a known cause); lack of motivation; and morbid suicidal thoughts. In severe cases, the individual may become psychotic, a condition also known as severe bipolar depression with psychotic features. These symptoms include delusions or, less commonly, hallucinations, usually unpleasant. A major depressive episode persists for at least two weeks, and may continue for over six months if left untreated.[15]
Mixed affective episodes
In the context of bipolar disorder, a mixed state is a condition during which symptoms of mania and depression occur simultaneously. Typical examples include weeping during a manic episode or racing thoughts during a depressive episode. Individuals may also feel very frustrated in this state, for example thinking grandiose thoughts while at the same time feeling like a failure. Mixed states are often the most dangerous period of mood disorders, during which the risks of substance abuse, panic disorder, suicide attempts, and other complications increase greatly.[16]
Associated features
Associated features are clinical phenomena that often accompany the disorder but are not part of the diagnostic criteria. In adults with the condition, bipolar disorder is often accompanied by changes in cognitive processes and abilities. These include reduced attentional and executive capabilities and impaired memory. How the individual processes the world also depends on the phase of the disorder, with differential characteristics between the manic, hypomanic and depressive states.[11] Some studies have found a significant association between bipolar disorder and creativity.[17] Some patients may have difficulty in maintaining relationships.[18]
There are several common childhood precursors seen in children who later receive a diagnosis of bipolar disorder. These include mood abnormalities, full major depressive episodes, and ADHD.[19]
Causes
The causes of bipolar disorder likely vary between individuals. Twin studies have been limited by relatively small sample sizes but have indicated a substantial genetic contribution, as well as environmental influence. For bipolar I, the (probandwise) concordance rates in modern studies have been consistently put at around 40% in monozygotic twins (same genes), compared to 0 to 10% in dizygotic twins.[20] A combination of bipolar I, II and cyclothymia produced concordance rates of 42% vs 11%, with a relatively lower ratio for bipolar II that likely reflects heterogeneity. The overall heritability of the bipolar spectrum has been put at 0.71.[21] There is overlap with unipolar depression and if this is also counted in the co-twin the concordance with bipolar disorder rises to 67% in monozygotic twins and 19% in dizigotic.[22] The relatively low concordance between dizygotic twins brought up together suggests that shared family environmental effects are limited, although the ability to detect them has been limited by small sample sizes.[21]
Genetic
Genetic studies have suggested many chromosomal regions and candidate genes appearing to relate to bipolar disorder's development, but the results are not consistent and often not replicated.[23]
Although the first genetic linkage finding for mania was in 1969,[24] the linkage studies have been inconsistent.[25] Meta-analyses of linkage studies detected either no significant genome-wide findings or, using a different methodology, only two genome-wide significant peaks, on chromosome 6q and on 8q21.[citation needed] Neither have genome-wide association studies brought a consistent focus—each has identified new loci.[25] Nonparametric linkage analysis using rank based methods did not detect genome-wide significant linkage findings[26] whereas joint analysis of all linkage data sets identified two genome wide significant peaks on chromosome 6q and on 8q21. [27]
Findings point strongly to heterogeneity, with different genes being implicated in different families.[28] Individual genes are likely to have only a small effect and to be involved in some aspect related to the disorder (and a broad range of "normal" human behavior) rather than the disorder per se.[29] Robust and replicable genome-wide significant associations showed several common polymorphisms, including variants within the genes CACNA1C, ODZ4, and NCAN.[30]
Advanced paternal age has been linked to a somewhat increased chance of bipolar disorder in offspring, consistent with a hypothesis of increased new genetic mutations.[31]
Physiological
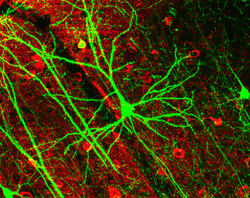
Abnormalities in the structure and/or function of certain brain circuits could underlie bipolar. Meta-analyses of structural MRI studies in bipolar disorder report an increase in the volume of the lateral ventricles, globus pallidus and increase in the rates of deep white matter hyperintensities.[32][33][34] Functional MRI findings suggest that abnormal modulation between ventral prefrontal and limbic regions, especially the amygdala, likely contribute to poor emotional regulation and mood symptoms.[35]
According to the "kindling" hypothesis, when people who are genetically predisposed toward bipolar disorder experience stressful events, the stress threshold at which mood changes occur becomes progressively lower, until the episodes eventually start (and recur) spontaneously. There is evidence of hypothalamic-pituitary-adrenal axis (HPA axis) abnormalities in bipolar disorder due to stress.[36][37][38][39]
Other brain components which have been proposed to play a role are the mitochondria,[40] and a sodium ATPase pump,[41] causing cyclical periods of poor neuron firing (depression) and hypersensitive neuron firing (mania). This may only apply for type one, but type two apparently results from a large confluence of factors.[citation needed] Circadian rhythms and melatonin activity also seem to be altered.[42]
Environmental
Evidence suggests that environmental factors play a significant role in the development and course of bipolar disorder, and that individual psychosocial variables may interact with genetic dispositions.[29] There is fairly consistent evidence from prospective studies that recent life events and interpersonal relationships contribute to the likelihood of onsets and recurrences of bipolar mood episodes, as they do for onsets and recurrences of unipolar depression.[43] There have been repeated findings that between a third and a half of adults diagnosed with bipolar disorder report traumatic/abusive experiences in childhood, which is associated on average with earlier onset, a worse course, and more co-occurring disorders such as PTSD.[44] The total number of reported stressful events in childhood is higher in those with an adult diagnosis of bipolar spectrum disorder compared to those without, particularly events stemming from a harsh environment rather than from the child's own behavior.[45]
Neurological
Less commonly bipolar disorder or a bipolar-like disorder may occur as a result of or in association with a neurological condition or injury. Such conditions and injuries may include (but are not limited to) stroke, traumatic brain injury, HIV infection, multiple sclerosis, porphyria and rarely temporal lobe epilepsy.[46]
Neuroendocrinological
Dopamine, a known neurotransmitter responsible for mood cycling, has been shown to have increased transmission during the manic phase. The dopamine hypothesis states that the increase in dopamine results in secondary homeostatic down regulation of key systems and receptors such as an increase in dopamine mediated G protein-coupled receptors. This results in decreased dopamine transmission characteristic of the depressive phase. The depressive phase ends with homeostatic up regulation potentially restarting the cycle over again.[47]
Two additional neurotransmitters, gamma-Aminobutyric acid (GABA) and glutamate, have been found to cause elevated mood states. Glutamate is significantly increased within the left dorsolateral prefrontal cortex during the manic phase of bipolar disorder, and returns to normal levels once the phase is over.[48] GABA is found in higher concentrations in people with bipolar disorder, overall leading to a decrease in GABA (B) receptors.[49][50] The increase in GABA is possibly caused by a disturbance in early development causing a disturbance of cell migration and the formation of normal lamination, the layering of brain structures commonly associated with the cerebral cortex.[51]
Research shows that a dysregulated hypothalamic-pituitary-adrenal axis (HPA axis) plays a role in the pathology of major depression.[52] Recently, there has been additional research showing that the HPA axis also contributes to the pathology of bipolar disorder. One study found an increase in cortisol in major depression patients and in bipolar patients in both manic and depressed phases.[53] An additional study found that there were increases in cortisol in both active bipolar patients and remissive bipolar patients indicating an overall deficit in HPA axis functioning in people with bipolar disorder.[54]
Evolutionary
Because bipolar disorder affects an individual’s ability to function in society and has a high morbidity rate, evolutionary theory would suggest that the genes responsible would have been naturally selected against, effectively culling the disorder. Yet there continue to be high rates of bipolar disorder in many populations, suggesting an evolutionary benefit to the genes responsible.
Proponents of evolutionary medicine hypothesize that the genes that cause severe bipolar disorder when inherited in large doses may actually increase fitness when inherited in small doses.[55] High rates of bipolar disorder throughout history suggest that the ability to switch between depressive and manic moods conveyed some evolutionary advantage on ancestral humans. Theories put forward to explain the evolutionary advantages of major depressive disorder may also explain the adaptiveness of the depressive episodes of bipolar disorder. For example, in individuals under increased stress, depressive mood may serve as a defensive strategy that causes the individual to retreat from the external stressor, increase sleep, and preserve resources and energy for better times.[56] Additionally, manic moods may convey advantage in some situations. Creativity, confidence, and high energy have all been linked to mania and hypomania.[57][58] The ability to utilize mild manic symptoms to be more productive and think more creatively during stress-free times may have increased the fitness of ancestral humans. Being able to employ both hypomania and mild depression convey advantages that benefit individuals in a variable environment. However, if the genes enabling the manipulation of both of these moods are over activated, the manic and/or severe depressive moods of full bipolar disorder may be triggered instead.
Evolutionary biologists have hypothesized that bipolar disorder could have come from an adaptation to extreme climactic conditions in the northern temperate zone during the Pleistocene. The Evolutionary Origin of Bipolar Disorder (EOBD) hypothesis states that during the short summers of extreme climactic zones, hypomania would be adaptive, allowing the completion of many tasks necessary for survival within a short period of time. During long winters the lethargy, hypersomnia, lack of interest in social activities, and overeating of depression would be adaptive to group cohesion and survival.[59] Evidence for the EOBD hypothesis include an association between bipolar disorder and a cold-adapted build, correlation between seasonality and mood changes in those with bipolar disorder, and low rates of bipolar disorder in African Americans.[60] The EOBD hypothesis suggests that in the absence of the extreme climactic conditions that fostered the success of bipolar disorder genes, many bipolar disorder behaviors are maladaptive and can often severely impair normal functioning.
Prevention
Prevention of bipolar has focused on stress (such as childhood adversity or highly conflictual families) which, although not a diagnostically specific causal agent for bipolar, does place genetically and biologically vulnerable individuals at risk for a more pernicious course of illness.[61] There has been debate regarding the causal relationship between usage of cannabis and bipolar disorder.[62]
Diagnosis
Diagnosis is based on the self-reported experiences of an individual as well as abnormalities in behavior reported by family members, friends or co-workers, followed by secondary signs observed by a psychiatrist, nurse, social worker, clinical psychologist or other clinician in a clinical assessment. There are lists of criteria for someone to be so diagnosed. These depend on both the presence and duration of certain signs and symptoms. Assessment is usually done on an outpatient basis; admission to an inpatient facility is considered if there is a risk to oneself or others. The most widely used criteria for diagnosing bipolar disorder are from the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, the current version being DSM-IV-TR, and the World Health Organization's International Statistical Classification of Diseases and Related Health Problems, currently the ICD-10. The latter criteria are typically used in Europe and other regions while the DSM criteria are used in the USA and other regions, as well as prevailing in research studies. The DSM-V, to be published in 2013, will likely include further and more accurate sub-typing.[63]
An initial assessment may include a physical exam by a physician. Although there are no biological tests which confirm bipolar disorder, tests may be carried out to exclude medical illnesses such as hypo- or hyperthyroidism, metabolic disturbance, a systemic infection or chronic disease, and syphilis or HIV infection. An EEG may be used to exclude epilepsy, and a CT scan of the head to exclude brain lesions. Investigations are not generally repeated for relapse unless there is a specific medical indication.
Several rating scales for the screening and evaluation of bipolar disorder exist, such as the Bipolar spectrum diagnostic scale.[64] The use of evaluation scales can not substitute a full clinical interview but they serve to systematize the recollection of symptoms.[64] On the other hand instruments for the screening of bipolar disorder have low sensitivity and limited diagnostic validity.[64]
Bipolar spectrum
Bipolar spectrum refers to a category of mood disorders that feature abnormally elevated or depressed mood. These disorders range from bipolar I disorder, featuring full-blown manic episodes, to cyclothymia, featuring less prominent hypomanic episodes, to "subsyndromal" conditions where only some of the criteria for mania or hypomania are met. These disorders typically also involve depressive symptoms or episodes that alternate with the elevated mood states, or with mixed episodes that feature symptoms of both.[65] The concept of the bipolar spectrum is similar to that of Emil Kraepelin's original concept of manic depressive illness.[66] Currently, manic depressive illness is usually referred to as bipolar disorder or simply bipolar. A simple nomenclature system was introduced in 1978 to classify more easily individuals' affectedness within the spectrum.[67]
Points on the spectrum using this nomenclature are denoted using the following codes:
- M—severe mania
- D—severe depression (unipolar depression)
- m—less severe mania (hypomania)
- d—less severe depression
Thus, mD represents a case with hypomania and major depression. A further distinction is sometimes made in the ordering of the letters, to represent the order of the episodes, where the patient's normal state is euthymic, interrupted by episodes of mania followed by depression (MD) or vice versa (DM).
Employing this schema, major depression would be denoted D. Unipolar mania (M) is, depending on the authority cited, either very rare,[68] or nonexistent with such cases actually being Md.
Unipolar hypomania (m) without accompanying depression has been noted in the medical literature.[69] There is speculation as to whether this condition may occur with greater frequency in the general, untreated population; successful social function of these potentially high-achieving individuals may lead to being labeled as normal, rather than as individuals with substantial dysregulation.
Criteria and subtypes
There is no clear consensus as to how many types of bipolar disorder exist.[70] In DSM-IV-TR and ICD-10, bipolar disorder is conceptualized as a spectrum of disorders occurring on a continuum. The DSM-IV-TR lists three specific subtypes and one for non-specified:[71][72]
Bipolar I disorder: One or more manic episodes. Subcategories specify whether there has been more than one episode, and the type of the most recent episode.[73] A depressive or hypomanic episode is not required for diagnosis, but it frequently occurs.
Bipolar II disorder: No manic episodes, but one or more hypomanic episodes and one or more major depressive episode.[74] Hypomanic episodes do not go to the full extremes of mania (i.e., do not usually cause severe social or occupational impairment, and are without psychosis), and this can make bipolar II more difficult to diagnose, since the hypomanic episodes may simply appear as a period of successful high productivity and is reported less frequently than a distressing, crippling depression.
Cyclothymia: A history of hypomanic episodes with periods of depression that do not meet criteria for major depressive episodes.[75] There is a low-grade cycling of mood which appears to the observer as a personality trait, and interferes with functioning.
Bipolar disorder NOS (not otherwise specified): This is a catchall category, diagnosed when the disorder does not fall within a specific subtype.[76] Bipolar NOS can still significantly impair and adversely affect the quality of life of the patient.
The bipolar I and II categories have specifiers that indicate the presentation and course of the disorder. For example, the "with full interepisode recovery" specifier applies if there was full remission between the two most recent episodes.[77]
Rapid cycling
Most people who meet criteria for bipolar disorder experience a number of episodes, on average 0.4 to 0.7 per year, lasting three to six months.[78] Rapid cycling, however, is a course specifier that may be applied to any of the above subtypes. It is defined as having four or more episodes per year and is found in a significant proportion of individuals with bipolar disorder. The definition of rapid cycling most frequently cited in the literature (including the DSM) is that of Dunner and Fieve: at least four major depressive, manic, hypomanic or mixed episodes are required to have occurred during a 12-month period.[79] Ultra-rapid (days) and ultra-ultra rapid or ultradian (within a day) cycling have also been described.[80] The literature examining the pharmacological treatment of rapid cycling is sparse and there is no clear consensus with respect to its optimal pharmacological management.[81]
Differential diagnosis
There are several other mental disorders which may involve similar symptoms to bipolar disorder. These include schizophrenia, attention deficit hyperactivity disorder (ADHD), and some personality disorders, including borderline personality.[82][83][84]
It has been noted that the bipolar disorder diagnosis is officially characterised in historical terms such that, technically, anyone with a history of (hypo)mania and depression has bipolar disorder whatever their current or future functioning and vulnerability. This has been described as "an ethical and methodological issue", as it means no one can be considered as being recovered (only "in remission") from bipolar disorder according to the official criteria. This is considered especially problematic given that brief hypomanic episodes are widespread among people generally and not necessarily associated with dysfunction.[11]
Comorbid conditions
The diagnosis of bipolar disorder can be complicated by coexisting (comorbid) psychiatric conditions such as obsessive-compulsive disorder, social phobia, panic disorder and attention-deficit hyperactivity disorder. Substance abuse may predate the appearance of bipolar symptoms, further complicating the diagnosis. A careful longitudinal analysis of symptoms and episodes, enriched if possible by discussions with friends and family members, is crucial to establishing a treatment plan where these comorbidities exist.[85]
Management

There are a number of pharmacological and psychotherapeutic techniques used to treat bipolar disorder. Individuals may use self-help and pursue recovery.
Hospitalization may be required especially with the manic episodes present in bipolar I. This can be voluntary or (if mental health legislation allows and varying state-to-state regulations in the USA) involuntary (called civil or involuntary commitment). Long-term inpatient stays are now less common due to deinstitutionalization, although these can still occur.[86] Following (or in lieu of) a hospital admission, support services available can include drop-in centers, visits from members of a community mental health team or Assertive Community Treatment team, supported employment and patient-led support groups, intensive outpatient programs. These are sometimes referred to partial-inpatient programs.[87]
Psychosocial
Psychotherapy is aimed at alleviating core symptoms, recognizing episode triggers, reducing negative expressed emotion in relationships, recognizing prodromal symptoms before full-blown recurrence, and, practicing the factors that lead to maintenance of remission[88][89][90] Cognitive behavioural therapy, family-focused therapy, and psychoeducation have the most evidence for efficacy in regard to relapse prevention, while interpersonal and social rhythm therapy and cognitive-behavioural therapy appear the most effective in regard to residual depressive symptoms. Most studies have been based only on bipolar I, however, and treatment during the acute phase can be a particular challenge.[91] Some clinicians emphasize the need to talk with individuals experiencing mania, to develop a therapeutic alliance in support of recovery.[92]
Medication

A number of medications are used to treat bipolar disorder.[93] The medication with the best evidence is lithium, which is effective in treating acute manic episodes,[94] and preventing relapses, more so for manic than for depressive episodes.[95] Lithium reduces the risk of suicide, self-harm, and death in people with bipolar disorder.[96]
Four anticonvulsants are used in the treatment of bipolar disorder. Carbamazepine is effective in treating manic episodes, with some evidence it has greater benefit in rapid-cycling bipolar disorder, or those with more psychotic symptoms or a more schizoaffective clinical picture. It is less effective in preventing relapse than lithium.[97] Carbamazepine became a popular treatment option for bipolar in the late 1980s and early 1990s, but was displaced by sodium valproate in the 1990s,[citation needed] which has become a commonly prescribed treatment, and is effective in treating manic episodes.[98] Lamotrigine has some efficacy in treating bipolar depression, and this benefit is greatest in more severe depression.[99] It has also been shown to have some benefit in preventing further episodes, though there are concerns about the studies done, and is of no benefit in rapid cycling disorder.[100] The effectiveness of topiramate is unknown.[101] Depending on the severity of the case, anti-convulsants may be used in combination with lithium or on their own.[102]
Antipsychotics have been found to be useful in managing mania associated with bipolar disorder however the long term effects are not clear.[103] Olanzapine is effective in preventing relapses, although the evidence is not as solid as for lithium.[104] Antidepressants have not been found to be of any benefit over that found with mood stabilizers.[105]
Short courses of benzodiazepines may be used as adjunct to medications until mood stabilizing become effective.[106]
Omega 3 fatty acids, in addition to normal pharmacological treatment, may have beneficial effects on depressive symptoms, although studies have been scarce and of variable quality.[107]
Prognosis
For many individuals with bipolar disorder a good prognosis results from good treatment, which, in turn, results from an accurate diagnosis. Because bipolar disorder can have a high rate of both under-diagnosis and misdiagnosis,[1] it is often difficult for individuals with the condition to receive timely and competent treatment.
Bipolar disorder can be a severely disabling medical condition. However, many individuals with bipolar disorder can live full and satisfying lives. Quite often, medication is needed to enable this. Persons with bipolar disorder may have periods of normal or near normal functioning between episodes.[108]
Functioning
A recent 20-year prospective study on bipolar I and II found that functioning varied over time along a spectrum from good to fair to poor. During periods of major depression or mania (in BPI), functioning was on average poor, with depression being more persistently associated with disability than mania. Functioning between episodes was on average good — more or less normal. Subthreshold symptoms were generally still substantially impairing, however, except for hypomania (below or above threshold) which was associated with improved functioning.[109]
Another study confirmed the seriousness of the disorder as "the standardized all-cause mortality ratio among patients with bipolar disorder is increased approximately two-fold." Bipolar disorder is currently regarded "as possibly the most costly category of mental disorders in the United States." Episodes of abnormality are associated with distress and disruption, and an elevated risk of suicide, especially during depressive episodes.[110]
Recovery and recurrence
A naturalistic study from first admission for mania or mixed episode (representing the hospitalized and therefore most severe cases) found that 50% achieved syndromal recovery (no longer meeting criteria for the diagnosis) within six weeks and 98% within two years. Within two years, 72% achieved symptomatic recovery (no symptoms at all) and 43% achieved functional recovery (regaining of prior occupational and residential status). However, 40% went on to experience a new episode of mania or depression within 2 years of syndromal recovery, and 19% switched phases without recovery.[111]
Symptoms preceding a relapse (prodromal), specially those related to mania, can be reliably identified by people with bipolar disorder.[112] There have been intents to teach patients coping strategies when noticing such symptoms with encouraging results.[113]
Mortality
Bipolar disorder can cause suicidal ideation that leads to suicidal attempts. One out of three people with bipolar disorder report past attempts of suicide or complete it,[114] and the annual average suicide rate is 0.4%, which is 10 to 20 times that of the general population.[115] The standardized mortality ratio from suicide in bipolar disorder is between 18 and 25.[116]
Epidemiology

no data
<180
180–186
186–190
190–195
195–200
200–205
|
205–210
210–215
215–220
220–225
225–230
230–235
|
Lifetime prevalence of bipolar disorder type I, which includes at least one manic episode during a lifetime, has generally been estimated at 2%.[117] However, a reanalysis of data from the National Epidemiological Catchment Area survey in the United States suggested that 0.8% of the population experience a manic episode at least once (the diagnostic threshold for bipolar I) and a further 0.5% have a hypomanic episode (the diagnostic threshold for bipolar II or cyclothymia). Including sub-threshold diagnostic criteria, such as one or two symptoms over a short time-period, an additional 5.1% of the population, adding up to a total of 6.4%, were classified as having a bipolar spectrum disorder.[118] A more recent analysis of data from a second US National Comorbidity Survey found that 1% met lifetime prevalence criteria for bipolar I, 1.1% for bipolar II, and 2.4% for subthreshold symptoms.[119] There are conceptual and methodological limitations and variations in the findings. Prevalence studies of bipolar disorder are typically carried out by lay interviewers who follow fully structured/fixed interview schemes; responses to single items from such interviews may suffer limited validity. In addition, diagnoses (and therefore estimates of prevalence) vary depending on whether a categorical or spectrum approach is used. This consideration has led to concerns about the potential for both underdiagnosis and overdiagnosis.[120]
Rates are similar in men and women and, broadly, across different cultures and ethnic groups.[121] A 2000 study by the World Health Organization found that prevalence and incidence of bipolar disorder are very similar across the world. Age-standardized prevalence per 100,000 ranged from 421.0 in South Asia to 481.7 in Africa and Europe for men and from 450.3 in Africa and Europe to 491.6 in Oceania for women.[122] However, severity may differ widely across the globe. Disability-adjusted life year rates, for example, appear to be higher in developing countries, where medical coverage may be poorer and medication less available.
Within the United States, African and European Americans have similar rates of bipolar disorder, while Asian Americans have lower rates.[123]
Late adolescence and early adulthood are peak years for the onset of bipolar disorder.[124][125] One study also found that in 10% of bipolar cases, the onset of mania had happened after the patient had turned 50.[126]
History

Variations in moods and energy levels have been observed as part of the human experience since time immemorial. The words "melancholia" (an old word for depression) and "mania" originated in Ancient Greek. The word melancholia is derived from melas/μελας, meaning "black", and chole/χολη, meaning "bile" or "gall",[127] indicative of the term's origins in pre-Hippocratic humoral theories. Within the humoral theories, mania was viewed as arising from an excess of yellow bile, or a mixture of black and yellow bile. The linguistic origins of mania, however, are not so clear-cut. Several etymologies are proposed by the Roman physician Caelius Aurelianus, including the Greek word ania, meaning "to produce great mental anguish", and manos, meaning "relaxed" or "loose", which would contextually approximate to an excessive relaxing of the mind or soul.[128] There are at least five other candidates, and part of the confusion surrounding the exact etymology of the word mania is its varied usage in the pre-Hippocratic poetry and mythologies.[128]
In the early 1800s, French psychiatrist Jean-Étienne Dominique Esquirol's lypemania, one of his affective monomanias, was the first elaboration on what was to become modern depression.[129] The basis of the current conceptualisation of manic–depressive illness can be traced back to the 1850s; on January 31, 1854, Jules Baillarger described to the French Imperial Academy of Medicine a biphasic mental illness causing recurrent oscillations between mania and depression, which he termed folie à double forme ("dual-form insanity").[130] Two weeks later, on February 14, 1854, Jean-Pierre Falret presented a description to the Academy on what was essentially the same disorder, and designated folie circulaire ("circular insanity") by him.[131]
These concepts were developed by the German psychiatrist Emil Kraepelin (1856–1926), who, using Kahlbaum's concept of cyclothymia,[132] categorized and studied the natural course of untreated bipolar patients. He coined the term manic depressive psychosis, after noting that periods of acute illness, manic or depressive, were generally punctuated by relatively symptom-free intervals where the patient was able to function normally.[133]
The term "manic–depressive reaction" appeared in the first American Psychiatric Association Diagnostic Manual in 1952, influenced by the legacy of Adolf Meyer who had introduced the paradigm illness as a reaction of biogenetic factors to psychological and social influences.[134] Subclassification of bipolar disorder was first proposed by German psychiatrist Karl Leonhard in 1957; he was also the first to introduce the terms bipolar (for those with mania) and unipolar (for those with depressive episodes only).[135]
Society and culture

There are widespread problems with social stigma, stereotypes, and prejudice against individuals with a diagnosis of bipolar disorder.[136]
Kay Redfield Jamison, a clinical psychologist and Professor of Psychiatry at the Johns Hopkins University School of Medicine, profiled her own bipolar disorder in her memoir An Unquiet Mind (1995).[137] In his autobiography Manicdotes: There's Madness in His Method (2008) Chris Joseph describes his struggle between the creative dynamism which allowed the creation of his multi-million pound advertising agency Hook Advertising, and the money-squandering dark despair of his bipolar illness.[138]
Several dramatic works have portrayed characters with traits suggestive of the diagnosis that has been the subject of discussion by psychiatrists and film experts alike. A notable example is Mr. Jones (1993), in which Mr. Jones (Richard Gere) swings from a manic episode into a depressive phase and back again, spending time in a psychiatric hospital and displaying many of the features of the syndrome.[139] In The Mosquito Coast (1986), Allie Fox (Harrison Ford) displays some features including recklessness, grandiosity, increased goal-directed activity and mood lability, as well as some paranoia.[140] Psychiatrists have suggested that Willy Loman, the main character in Arthur Miller's classic play Death of a Salesman, suffers from bipolar disorder,[141] though that specific term for the condition did not exist when the play was written.
TV specials, for example the BBC's The Secret Life of the Manic Depressive,[142] MTV's True Life: I'm Bipolar, talk shows, and public radio shows, and the greater willingness of public figures to discuss their own bipolar disorder, have focused on psychiatric conditions, thereby, raising public awareness.
On April 7, 2009, the nighttime drama 90210 on the CW network, aired a special episode where the character Silver was diagnosed with bipolar disorder.[143] Stacey Slater, a character from the BBC soap EastEnders, has been diagnosed with the disorder. The storyline was developed as part of the BBC's Headroom campaign.[144] The Channel 4 soap Brookside had earlier featured a story about bipolar disorder when the character Jimmy Corkhill was diagnosed with the condition.[145]
Specific populations
Children

In the 1920s, Emil Kraepelin noted that manic episodes are rare before puberty.[146] In general, bipolar disorder in children was not recognized in the first half of the twentieth century. This issue diminished with an increased following of the DSM criteria in the last part of the twentieth century.[146][147]
While in adults the course of bipolar disorder is characterized by discrete episodes of depression and mania with no clear symptomatology between them, in children and adolescents very fast mood changes or even chronic symptoms are the norm.[148] On the other hand, pediatric bipolar disorder, instead of euphoric mania, commonly develops with outbursts of anger, irritability and psychosis, less common in adults.[146][148]
The diagnosis of childhood bipolar disorder is controversial,[148] although it is not under discussion that the typical symptoms of bipolar disorder have negative consequences for minors suffering them.[146] The debate is mainly centered on whether what is called bipolar disorder in children refers to the same disorder as when diagnosing adults,[146] and the related question of whether the criteria for diagnosis for adults are useful and accurate when applied to children.[148] Regarding diagnosis of children, some experts recommend following the DSM criteria.[148] Others believe that these criteria do not correctly separate children with bipolar disorder from other problems such as ADHD, and emphasize fast mood cycles.[148] Still others argue that what accurately differentiates children with bipolar disorder is irritability.[148] The practice parameters of the AACAP encourage the first strategy.[146][148] American children and adolescents diagnosed with bipolar disorder in community hospitals increased 4-fold reaching rates of up to 40% in 10 years around the beginning of the 21st century, while in outpatient clinics it doubled reaching 6%.[148] Studies using DSM criteria show that up to 1% of youth may have bipolar disorder.[146]
Treatment involves medication and psychotherapy.[148] Drug prescription usually consists in mood stabilizers and atypical antipsychotics.[148] Among the former, lithium is the only compound approved by the FDA for children.[146] Psychological treatment combines normally education on the disease, group therapy and cognitive behavioral therapy.[148] Chronic medication is often needed.[148]
Current research directions for bipolar disorder in children include optimizing treatments, increasing the knowledge of the genetic and neurobiological basis of the pediatric disorder and improving diagnostic criteria.[148] The DSM-V has proposed a new diagnosis which is considered to cover some presentations currently thought of as childhood-onset bipolar.[149]
Elderly
There is a relative lack of knowledge about bipolar disorder in late life. There is evidence that it becomes less prevalent with age but nevertheless accounts for a similar percentage of psychiatric admissions; that older bipolar patients had first experienced symptoms at a later age; that later onset of mania is associated with more neurologic impairment; that substance abuse is considerably less common in older groups; and that there is probably a greater degree of variation in presentation and course, for instance individuals may develop new-onset mania associated with vascular changes, or become manic only after recurrent depressive episodes, or may have been diagnosed with bipolar disorder at an early age and still meet criteria. There is also some weak evidence that mania is less intense and there is a higher prevalence of mixed episodes, although there may be a reduced response to treatment. Overall, there are likely more similarities than differences from younger adults.[150][151] In the elderly, recognition and treatment of bipolar disorder may be complicated by the presence of dementia or the side effects of medications being taken for other conditions.[152]
See also
- Bipolar disorders research
- Bipolar Disorders (journal)
References
- ↑ 1.0 1.1 Bowden, C. L. (2001). "Strategies to reduce misdiagnosis of bipolar depression". Psychiatric services (Washington, D.C.) 52 (1): 51–55. doi:10.1176/appi.ps.52.1.51. PMID 11141528.
- ↑ Muzina, DJ; Kemp, DE; McIntyre, RS (2007 Oct–Dec). "Differentiating bipolar disorders from major depressive disorders: treatment implications". Annals of Clinical Psychiatry 19 (4): 305–12. doi:10.1080/10401230701653591. PMID 18058287.
- ↑ Mayo Clinic staff. "Bipolar disorder: Tests and diagnosis". MayoClinic.com. Retrieved 2010-07-19.
- ↑ DSM-IV 1994, p. 357.
- ↑ Read, Kimberly (2010-02-27). "Warning Signs of Mania". About.com. Retrieved 2010-12-06.
- ↑ "Bipolar Disorder". National Institute of Mental Health (NIMH). Revised 2012. Retrieved 6 July 2012.
- ↑ Dean, k; Walsh E, Morgan C, et al. (2007). "Aggressive behaviour at first contact with services: findings from the AESOP First Episode Psychosis Study". Psychological Medicine 37 (4): 547–57. doi:10.1017/S003329170600892. PMID 17018170.
- ↑ Altman, E. G.; Hedeker, D.; Peterson, J. L.; Davis, J. M. (1997). "The Altman Self-Rating Mania Scale". Biological Psychiatry 42 (10): 948–955. doi:10.1016/S0006-3223(96)00548-3. PMID 9359982.
- ↑ Young, R. C.; Biggs, J. T.; Ziegler, V. E.; Meyer, D. A. (1978). "A rating scale for mania: Reliability, validity and sensitivity". The British journal of psychiatry : the journal of mental science 133: 429–435. doi:10.1192/bjp.133.5.429. PMID 728692.
- ↑ Furukawa, T. A. (2010). "Assessment of mood: Guides for clinicians". Journal of Psychosomatic Research 68 (6): 581–589. doi:10.1016/j.jpsychores.2009.05.003. PMID 20488276.
- ↑ 11.0 11.1 11.2 Mansell, W.; Pedley, R. (2008). "The ascent into mania: A review of psychological processes associated with the development of manic symptoms". Clinical Psychology Review 28 (3): 494–520. doi:10.1016/j.cpr.2007.07.010. PMID 17825463.
- ↑ "Hypomania and Mania Symptoms in Bipolar Disorder". WebMD.com. January 10, 2010.
- ↑ "Bipolar Disorder: NIH Publication No. 95-3679". U.S. National Institutes of Health. September 1995. Archived from the original on 2008-04-29.
- ↑ "Bipolar II Disorder Symptoms and Signs". Web M.D. Retrieved 2010-12-06.
- ↑ "Practice Guideline for the Treatment of Patients With Bipolar Disorder Second Edition". APA Practice Guidelines for the Treatment of Psychiatric Disorders: Comprehensive Guidelines and Guideline Watches 1. 2006. doi:10.1176/appi.books.9780890423363.50051. ISBN 978-0-89042-336-3.
- ↑ Goldman E (1999). "Severe Anxiety, Agitation are Warning Signals of Suicide in Bipolar Patients". Clin Psychiatr News: 25.
- ↑ Srivastava, S.; Ketter, T. A. (2010). "The Link Between Bipolar Disorders and Creativity: Evidence from Personality and Temperament Studies". Current Psychiatry Reports 12 (6): 522–530. doi:10.1007/s11920-010-0159-x. PMID 20936438.
- ↑ Jamison & Goodwin 2007, p. 338.
- ↑ Andreoli, T. E. (1989). "Molecular aspects of endocrinology". Hospital practice (Office ed.) 24 (8): 11–12. PMID 2504732.
- ↑ Kieseppa, T.; Partonen, T.; Haukka, J.; Kaprio, J.; Lönnqvist, J. (2004). "High Concordance of Bipolar I Disorder in a Nationwide Sample of Twins". American Journal of Psychiatry 161 (10): 1814–1821. doi:10.1176/appi.ajp.161.10.1814. PMID 15465978.
- ↑ 21.0 21.1 Edvardsen, J.; Torgersen, S.; Røysamb, E.; Lygren, S.; Skre, I.; Onstad, S.; Øien, P. A. (2008). "Heritability of bipolar spectrum disorders. Unity or heterogeneity?". Journal of Affective Disorders 106 (3): 229–240. doi:10.1016/j.jad.2007.07.001. PMID 17692389.
- ↑ McGuffin, P.; Rijsdijk, F.; Andrew, M.; Sham, P.; Katz, R.; Cardno, A. (2003). "The Heritability of Bipolar Affective Disorder and the Genetic Relationship to Unipolar Depression". Archives of General Psychiatry 60 (5): 497–502. doi:10.1001/archpsyc.60.5.497. PMID 12742871.
- ↑ Kato, T. (2007). "Molecular genetics of bipolar disorder and depression". Psychiatry and Clinical Neurosciences 61 (1): 3–19. doi:10.1111/j.1440-1819.2007.01604.x. PMID 17239033.
- ↑ Reich, T.; Clayton, P. J.; Winokur, G. (1969). "Family history studies: V. The genetics of mania". The American Journal of Psychiatry 125 (10): 1358–1369. PMID 5304735.
- ↑ 25.0 25.1 Burmeister, M.; McInnis, M. G.; Zöllner, S. (2008). "Psychiatric genetics: Progress amid controversy". Nature Reviews Genetics 9 (7): 527–540. doi:10.1038/nrg2381. PMID 18560438.
- ↑ Segurado, R; Detera-Wadleigh, SD; Levinson, DF; Lewis, CM; Gill, M; Nurnberger JI, Jr; Craddock, N; DePaulo, JR; Baron, M; Gershon, ES; Ekholm, J; Cichon, S; Turecki, G; Claes, S; Kelsoe, JR; Schofield, PR; Badenhop, RF; Morissette, J; Coon, H; Blackwood, D; McInnes, LA; Foroud, T; Edenberg, HJ; Reich, T; Rice, JP; Goate, A; McInnis, MG; McMahon, FJ; Badner, JA; Goldin, LR; Bennett, P; Willour, VL; Zandi, PP; Liu, J; Gilliam, C; Juo, SH; Berrettini, WH; Yoshikawa, T; Peltonen, L; Lönnqvist, J; Nöthen, MM; Schumacher, J; Windemuth, C; Rietschel, M; Propping, P; Maier, W; Alda, M; Grof, P; Rouleau, GA; Del-Favero, J; Van Broeckhoven, C; Mendlewicz, J; Adolfsson, R; Spence, MA; Luebbert, H; Adams, LJ; Donald, JA; Mitchell, PB; Barden, N; Shink, E; Byerley, W; Muir, W; Visscher, PM; Macgregor, S; Gurling, H; Kalsi, G; McQuillin, A; Escamilla, MA; Reus, VI; Leon, P; Freimer, NB; Ewald, H; Kruse, TA; Mors, O; Radhakrishna, U; Blouin, JL; Antonarakis, SE; Akarsu, N (July 2003). "Genome scan meta-analysis of schizophrenia and bipolar disorder, part III: Bipolar disorder.". American Journal of Human Genetics 73 (1): 49–62. doi:10.1086/376547. PMC 1180589. PMID 12802785.
- ↑ McQueen, MB; Devlin, B; Faraone, SV; Nimgaonkar, VL; Sklar, P; Smoller, JW; Abou Jamra, R; Albus, M et al. (2005). "Combigned analysis from eleven linkage studies of bipolar disorder provides strong evidence of susceptibility loci on chromosomes 6q and 8q". Am. J. Hum. Genet. 77 (4): 582–595. doi:10.1086/491603. PMC 1275607. PMID 16175504.
- ↑ Segurado, R.; Deterawadleigh, S.; Levinson, D.; Lewis, C.; Gill, M.; Nurnbergerjr, J.; Craddock, N.; Depaulo, J.; Baron, M.; Gershon, E.; Ekholm, J.; Cichon, S.; Turecki, G.; Claes, S.; Kelsoe, J. R.; Schofield, P. R.; Badenhop, R. F.; Morissette, J.; Coon, H.; Blackwood, D.; McInnes, L. A.; Foroud, T.; Edenberg, H. J.; Reich, T.; Rice, J. P.; Goate, A.; McInnis, M. G.; McMahon, F. J.; Badner, J. A.; Goldin, L. R. (2003). "Genome Scan Meta-Analysis of Schizophrenia and Bipolar Disorder, Part III: Bipolar Disorder". The American Journal of Human Genetics 73 (1): 49–62. doi:10.1086/376547. PMC 1180589. PMID 12802785.
- ↑ 29.0 29.1 Serretti, A.; Mandelli, L. (2008). "The genetics of bipolar disorder: Genome 'hot regions,' genes, new potential candidates and future directions". Molecular Psychiatry 13 (8): 742–771. doi:10.1038/mp.2008.29. PMID 18332878.
- ↑ Craddock, N.; Sklar, P. (2013). "Genetics of bipolar disorder". The Lancet 381 (9878): 1654. doi:10.1016/S0140-6736(13)60855-7.
- ↑ Frans, E. M.; Sandin, S.; Reichenberg, A.; Lichtenstein, P.; Langstrom, N.; Hultman, C. M. (2008). "Advancing Paternal Age and Bipolar Disorder". Archives of General Psychiatry 65 (9): 1034–1040. doi:10.1001/archpsyc.65.9.1034. PMID 18762589.
- ↑ Kempton, M. J.; Geddes, J. R.; Ettinger, U.; Williams, S. C. R.; Grasby, P. M. (2008). "Meta-analysis, Database, and Meta-regression of 98 Structural Imaging Studies in Bipolar Disorder". Archives of General Psychiatry 65 (9): 1017–1032. doi:10.1001/archpsyc.65.9.1017. PMID 18762588.
- ↑ Arnone, D.; Cavanagh, J.; Gerber, D.; Lawrie, S. M.; Ebmeier, K. P.; McIntosh, A. M. (2009). "Magnetic resonance imaging studies in bipolar disorder and schizophrenia: Meta-analysis". The British Journal of Psychiatry 195 (3): 194–201. doi:10.1192/bjp.bp.108.059717. PMID 19721106.
- ↑ "Bipolar MRI Database". Bipolar Disorder Neuroimaging Database (BiND).
- ↑ Strakowski, S. M.; Adler, C. M.; Almeida, J.; Altshuler, L. L.; Blumberg, H. P.; Chang, K. D.; Delbello, M. P.; Frangou, S.; McIntosh, A.; Phillips, M. L.; Sussman, J. E.; Townsend, J. D. (2012). "The functional neuroanatomy of bipolar disorder: A consensus model". Bipolar Disorders 14 (4): 313–325. doi:10.1111/j.1399-5618.2012.01022.x. PMID 22631617.
- ↑ Post, R. M. (1992). "Transduction of psychosocial stress into the neurobiology of recurrent affective disorder". The American journal of psychiatry 149 (8): 999–1010. PMID 1353322.
- ↑ Monroe, S. M.; Harkness, K. L. (2005). "Life Stress, the "Kindling" Hypothesis, and the Recurrence of Depression: Considerations from a Life Stress Perspective". Psychological Review 112 (2): 417–445. doi:10.1037/0033-295X.112.2.417. PMID 15783292.
- ↑ Daban, C.; Vieta, E.; MacKin, P.; Young, A. H. (2005). "Hypothalamic-pituitary-adrenal Axis and Bipolar Disorder". Psychiatric Clinics of North America 28 (2): 469–480. doi:10.1016/j.psc.2005.01.005. PMID 15826743.
- ↑ Bender, R. E.; Alloy, L. B. (2011). "Life stress and kindling in bipolar disorder: Review of the evidence and integration with emerging biopsychosocial theories". Clinical Psychology Review 31 (3): 383–398. doi:10.1016/j.cpr.2011.01.004. PMC 3072804. PMID 21334286.
- ↑ Stork, C.; Renshaw, P. F. (2005). "Mitochondrial dysfunction in bipolar disorder: Evidence from magnetic resonance spectroscopy research". Molecular Psychiatry 10 (10): 900–919. doi:10.1038/sj.mp.4001711. PMID 16027739.
- ↑ Brown & Basso 2004, p. 16.
- ↑ Dallaspezia, S.; Benedetti, F. (2009). "Melatonin, circadian rhythms, and the clock genes in bipolar disorder". Current psychiatry reports 11 (6): 488–493. PMID 19909672.
- ↑ Alloy, L. B.; Abramson, L. Y.; Urosevic, S.; Walshaw, P. D.; Nusslock, R.; Neeren, A. M. (2005). "The psychosocial context of bipolar disorder: Environmental, cognitive, and developmental risk factors". Clinical Psychology Review 25 (8): 1043–1075. doi:10.1016/j.cpr.2005.06.006. PMID 16140445.
- ↑ Leverich, G. S.; Post, R. M. (2006). "Course of bipolar illness after history of childhood trauma". The Lancet 367 (9516): 1040–1042. doi:10.1016/S0140-6736(06)68450-X. PMID 16581389.
- ↑ Miklowitz, D. J.; Chang, K. D. (2008). "Prevention of bipolar disorder in at-risk children: Theoretical assumptions and empirical foundations". Development and Psychopathology 20 (3): 881–897. doi:10.1017/S0954579408000424. PMC 2504732. PMID 18606036.
- ↑ Murray ED, Buttner N, Price BH. (2012) Depression and Psychosis in Neurological Practice. In: Neurology in Clinical Practice, 6th Edition. Bradley WG, Daroff RB, Fenichel GM, Jankovic J (eds.) Butterworth Heinemann. April 12, 2012. ISBN 1437704344 | ISBN 978-1437704341
- ↑ Berk, M.; Dodd, S., Kauer-Sant'Anna, M., Malhi, G. S., Bourin, M., Kapczinski, F., & Norman, T. (2007). "Dopamine dysregulation syndrome: implications for a dopamine hypothesis of bipolar disorder. Acta Psychiatrica Scandinavica". Acta Psychiatrica Scandinavica 116: 41–49. doi:10.1111/j.1600-0447.2007.01058.x.
- ↑ Michael, N.; Erfurth, A., Ohrmann, P., Gossling, M., Arolt, V., Heindel, W., & Pfleiderer, B. (2003). "Acute mania is accompanied by elevated glutamate/glutamine levels within the left dorsolateral prefrontal cortex". Psychopharmacology 168 (3): 344–346. doi:10.1007/s00213-003-1440-z.
- ↑ Brady, R. O.; McCarthy, J. M., Prescot, A. P., Jensen, J. E., Cooper, A. J., Cohen, B. M., . . . Ongur, D. (2013). "Brain gamma-aminobutyric acid (GABA) abnormalities in bipolar disorder". Bipolar Disorders 15 (4): 434–439. doi:10.1111/bdi.12074.
- ↑ Fatemi, S. H.; Folsom, T. D., & Thuras, P. D. (2011). Schizophrenia Research 128 (1-3): 37–43. doi:10.1016/j.schres.2010.12.025.
- ↑ Benes, F. M.; Berretta, S. (2001). "GABAergic interneurons: implications for understanding schizophrenia and bipolar disorder". Neuropsychopharmacology 25 (1): 1–27.
- ↑ Vreeburg, S. A.; Hoogendijk, W. J., van Pelt, J., Derijk, R. H., Verhagen, J. C., van Dyck, R., . . . Penninx, B. W. (2009). "Major depressive disorder and hypothalamic-pituitary-adrenal axis activity: results from a large cohort study". Arch Gen Psychiatry 66 (6): 617–626. doi:10.1001/archgenpsychiatry.2009.50.
- ↑ Cervantes, P.; Gelber, S., Kin, F., Nair, V. N. P., & Schwartz, G. (2001). "Circadian secretion of cortisol in bipolar disorder". Journal of Psychiatry & Neuroscience 26 (5): 411–416.
- ↑ Watson, S.; Gallagher, P., Ritchie, J. C., Ferrier, I. N., & Young, A. H. (2004). "). Hypothalamic-pituitary-adrenal axis function in patients with bipolar disorder". British Journal of Psychiatry 184 (496-502).
- ↑ Phelps, J. "Chapter 5: The Big Picture--There Must Be Some Evolutionary Advantage?" The Biological Basis of Bipolar Disorder. Retrieved from http://www.psycheducation.org/BipolarMechanism/5BigPicture.htm
- ↑ Gilbert, P. (2005). "Evolution and depression: Issues and implications". Psychological Medicine 36 (3): 287–297. doi:10.1017/S0033291705006112. PMID 16236231.
- ↑ Jamison, K. R. (1993). Touched With Fire: Manic-depressive illness and the artistic temperament. New York, NY: The Free Press.
- ↑ Carey, B. (2005, April 6). "Hypomania's up side distinct but linked to bipolar disorder." New York Times News Service. Retrieved from http://www.utsandiego.com/uniontrib/20050406/news_1c06hypo.html
- ↑ Sherman, J. (2001). "Evolutionary Origin of Bipolar Disorder (EOBD)". Psycoloquy, 12(028), Retrieved from http://www.cogsci.ecs.soton.ac.uk/cgi/psyc/newpsy?12.028
- ↑ Sherman, J. A. (2012). "Evolutionary origin of bipolar disorder-revised: EOBD-R". Medical Hypotheses 78 (1): 113–122. doi:10.1016/j.mehy.2011.10.005. PMID 22036090.
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/18606036
- ↑ Khan, MA; Akella, S. "Cannabis-Induced Bipolar Disorder with Psychotic Features: A Case Report". Psychiatry (Edgmont) 6 (12): 44–48. PMC 2811144.
- ↑ Perugi, G.; Ghaemi, S. N.; Akiskal, H. (2006). "Diagnostic and Clinical Management Approaches to Bipolar Depression, Bipolar II and Their Comorbidities". Bipolar Psychopharmacotherapy. p. 193. doi:10.1002/0470017953.ch11. ISBN 9780470017951.
- ↑ 64.0 64.1 64.2 Picardi, A. (2009). "Rating scales in bipolar disorder". Current Opinion in Psychiatry 22 (1): 42–49. doi:10.1097/YCO.0b013e328315a4d2. PMID 19122534.
- ↑ Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (Text Revision). American Psychiatric Association. p. 2000.
- ↑ Across the Bipolar Spectrum: From Practice to Research
- ↑ Angst, J; Felder, W; Frey, R; Stassen, HH (1978). "The course of affective disorders. I. Change of diagnosis of monopolar, unipolar, and bipolar illness". Archiv fur Psychiatrie und Nervenkrankheiten 226 (1): 57–64. doi:10.1007/BF00344124. PMID 708227.
- ↑ Why No "Unipolar Mania" Listing in DSM-IV? | Serendip's Exchange
- ↑ Mood episodes and mood disorders: patterns of incidence and conversion in the first three decades of life, Katja Beesdo et al.,Bipolar Disorders Volume 11 Issue 6, Pages 637 - 64http://www3.interscience.wiley.com.ezp-prod1.hul.harvard.edu/journal/122542146/abstract
- ↑ Akiskal, H. S.; Benazzi, F. (2006). "The DSM-IV and ICD-10 categories of recurrent [major] depressive and bipolar II disorders: Evidence that they lie on a dimensional spectrum". Journal of Affective Disorders 92 (1): 45–54. doi:10.1016/j.jad.2005.12.035. PMID 16488021.
- ↑ DSM-IV 2000.
- ↑ "Bipolar Disorder". BehaveNet.
- ↑ "Bipolar I Disorder". BehaveNet.
- ↑ "Bipolar II Disorder". BehaveNet.
- ↑ "Cyclothymic Disorder". BehaveNet.
- ↑ "Not Otherwise Specified". BehaveNet.
- ↑ "Longitudinal Course Specifiers for Mood Disorders". BehaveNet.
- ↑ Angst, J.; Sellaro, R. (2000). "Historical perspectives and natural history of bipolar disorder". Biological Psychiatry 48 (6): 445–457. PMID 11018218.
- ↑ Bauer, M; Beaulieu, S; Dunner, DL; Lafer, B; Kupka, R (February 2008). "Rapid cycling bipolar disorder – diagnostic concepts". Bipolar Disorders 10 (1 Pt 2): 153–62. doi:10.1111/j.1399-5618.2007.00560.x. PMID 18199234.
- ↑ Tillman, R.; Geller, B. (2003). "Definitions of Rapid, Ultrarapid, and Ultradian Cycling and of Episode Duration in Pediatric and Adult Bipolar Disorders: A Proposal to Distinguish Episodes from Cycles". Journal of Child and Adolescent Psychopharmacology 13 (3): 267–271. doi:10.1089/104454603322572598. PMID 14642014.
- ↑ Fountoulakis, KN; Kontis, D; Gonda, X; Yatham, LN (March 2013). "A systematic review of the evidence on the treatment of rapid cycling bipolar disorder". Bipolar Disorders 15 (2): 115–227. doi:10.1111/bdi.12045.
- ↑ Sood, A. B.; Razdan, A.; Weller, E. B.; Weller, R. A. (2005). "How to differentiate bipolar disorder from attention deficit hyperactivity disorder and other common psychiatric disorders: A guide for clinicians". Current psychiatry reports 7 (2): 98–103. PMID 15802085.
- ↑ Magill, C. A. (2004). "The boundary between borderline personality disorder and bipolar disorder: Current concepts and challenges". Canadian journal of psychiatry. Revue canadienne de psychiatrie 49 (8): 551–556. PMID 15453104.
- ↑ Bassett, D. (2012). "Borderline personality disorder and bipolar affective disorder. Spectra or spectre? A review". Australian and New Zealand Journal of Psychiatry 46 (4): 327–339. doi:10.1177/0004867411435289. PMID 22508593.
- ↑ Sagman D and Tohen M (2009). "Comorbidity in Bipolar Disorder: The Complexity of Diagnosis and Treatment". Psychiatric Times.
- ↑ Becker, T.; Kilian, R. (2006). "Psychiatric services for people with severe mental illness across western Europe: What can be generalized from current knowledge about differences in provision, costs and outcomes of mental health care?". Acta Psychiatrica Scandinavica 113 (429): 9–16. doi:10.1111/j.1600-0447.2005.00711.x. PMID 16445476.
- ↑ McGurk, S. R.; Mueser, K. T.; Feldman, K.; Wolfe, R.; Pascaris, A. (2007). "Cognitive Training for Supported Employment: 2-3 Year Outcomes of a Randomized Controlled Trial". American Journal of Psychiatry 164 (3): 437–441. doi:10.1176/appi.ajp.164.3.437. PMID 17329468.
- ↑ Lam et al., 1999; Miklowitz & Goldstein, 1997; Frank, 2005.
- ↑ Leahy & Johnson 2003.
- ↑ Basco & Rush 2005.
- ↑ Zaretsky, A. E.; Rizvi, S.; Parikh, S. V. (2007). "How well do psychosocial interventions work in bipolar disorder?". Canadian journal of psychiatry. Revue canadienne de psychiatrie 52 (1): 14–21. PMID 17444074.
- ↑ Havens, L. L.; Ghaemi, S. N. (2005). "Existential despair and bipolar disorder: The therapeutic alliance as a mood stabilizer". American journal of psychotherapy 59 (2): 137–147. PMID 16170918.
- ↑ Bauer, MS; Mitchner, L (January 2004). "What is a "mood stabilizer"? An evidence-based response.". The American Journal of Psychiatry 161 (1): 3–18. doi:10.1176/appi.ajp.161.1.3. PMID 14702242.
- ↑ Poolsup, N; Li Wan Po, A; de Oliveira, IR (April 2000). "Systematic overview of lithium treatment in acute mania.". Journal of clinical pharmacy and therapeutics 25 (2): 139–56. doi:10.1046/j.1365-2710.2000.00278.x. PMID 10849192.
- ↑ Geddes, JR; Burgess, S; Hawton, K; Jamison, K; Goodwin, GM (February 2004). "Long-term lithium therapy for bipolar disorder: systematic review and meta-analysis of randomized controlled trials.". The American Journal of Psychiatry 161 (2): 217–22. doi:10.1176/appi.ajp.161.2.217. PMID 14754766.
- ↑ Cipriani, A.; Hawton, K.; Stockton, S.; Geddes, J. R. (27 June 2013). "Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis". BMJ 346 (jun27 4): f3646–f3646. doi:10.1136/bmj.f3646.
- ↑ Post, R. M.; Ketter, T. A.; Uhde, T.; Ballenger, J. C. (2007). "Thirty years of clinical experience with carbamazepine in the treatment of bipolar illness: Principles and practice". CNS Drugs 21 (1): 47–71. PMID 17190529.
- ↑ MacRitchie, K.; Geddes, J.; Scott, J.; Haslam, D. R.; Silva De Lima, M.; Goodwin, G. (2003). Valproate for acute mood episodes in bipolar disorder. In Reid, Keith. "Cochrane Database of Systematic Reviews". Cochrane database of systematic reviews (Online) (1): CD004052. doi:10.1002/14651858.CD004052. PMID 12535506.
- ↑ Geddes, J. R.; Calabrese, J. R.; Goodwin, G. M. (2008). "Lamotrigine for treatment of bipolar depression: Independent meta-analysis and meta-regression of individual patient data from five randomised trials". The British Journal of Psychiatry 194 (1): 4–9. doi:10.1192/bjp.bp.107.048504. PMID 19118318.
- ↑ Van Der Loos, M. L.; Kölling, P.; Knoppert-Van Der Klein, E. A.; Nolen, W. A. (2007). "Lamotrigine in the treatment of bipolar disorder, a review". Tijdschrift voor psychiatrie 49 (2): 95–103. PMID 17290338.
- ↑ Vasudev, K.; MacRitchie, K.; Geddes, J.; Watson, S.; Young, A. H. (2006). Topiramate for acute affective episodes in bipolar disorder. In Young, Allan H. "Cochrane Database of Systematic Reviews". Cochrane database of systematic reviews (Online) (1): CD003384. doi:10.1002/14651858.CD003384.pub2. PMID 16437453.
- ↑ Barker 2003, pp. 284–85.
- ↑ Geddes, JR; Miklowitz, DJ (May 11, 2013). "Treatment of bipolar disorder". Lancet 381 (9878): 1672–82. doi:10.1016/S0140-6736(13)60857-0. PMID 23663953.
- ↑ Cipriani, A.; Rendell, J. M.; Geddes, J. (2009). Olanzapine in long-term treatment for bipolar disorder. In Cipriani, Andrea. "Cochrane Database of Systematic Reviews". Cochrane database of systematic reviews (Online) (1): CD004367. doi:10.1002/14651858.CD004367.pub2. PMID 19160237.
- ↑ El-Mallakh, RS; Elmaadawi, AZ; Loganathan, M; Lohano, K; Gao, Y (July 2010). "Bipolar disorder: an update". Postgraduate Medicine 122 (4): 24–31. doi:10.3810/pgm.2010.07.2172. PMID 20675968.
- ↑ "Benzodiazepines for Bipolar Disorder". WebMD.com. Retrieved 13 February 2013.
- ↑ Montgomery, P; Richardson, AJ (Apr 16, 2008). "Omega-3 fatty acids for bipolar disorder". In Montgomery, Paul. The Cochrane database of systematic reviews (2): CD005169. doi:10.1002/14651858.CD005169.pub2. PMID 18425912.
- ↑ Bergen 1999.
- ↑ Judd, L. L.; Akiskal, H. S.; Schettler, P. J.; Endicott, J.; Leon, A. C.; Solomon, D. A.; Coryell, W.; Maser, J. D.; Keller, M. B. (2005). "Psychosocial Disability in the Course of Bipolar I and II Disorders: A Prospective, Comparative, Longitudinal Study". Archives of General Psychiatry 62 (12): 1322–1330. doi:10.1001/archpsyc.62.12.1322. PMID 16330720.
- ↑ Osby, U.; Brandt, L.; Correia, N.; Ekbom, A.; Sparén, P. (2001). "Excess mortality in bipolar and unipolar disorder in Sweden". Archives of General Psychiatry 58 (9): 844–850. PMID 11545667.
- ↑ Tohen, M.; Zarate Jr, C. A.; Hennen, J.; Khalsa, H. M.; Strakowski, S. M.; Gebre-Medhin, P.; Salvatore, P.; Baldessarini, R. J. (2003). "The McLean-Harvard First-Episode Mania Study: Prediction of recovery and first recurrence". The American Journal of Psychiatry 160 (12): 2099–2107. doi:10.1176/appi.ajp.160.12.2099. PMID 14638578.
- ↑ Jackson, A.; Cavanagh, J.; Scott, J. (2003). "A systematic review of manic and depressive prodromes". Journal of Affective Disorders 74 (3): 209–217. PMID 12738039.
- ↑ Lam, D.; Wong, G. (2005). "Prodromes, coping strategies and psychological interventions in bipolar disorders". Clinical Psychology Review 25 (8): 1028–1042. doi:10.1016/j.cpr.2005.06.005. PMID 16125292.
- ↑ Novick, D. M.; Swartz, H. A.; Frank, E. (2010). "Suicide attempts in bipolar I and bipolar II disorder: A review and meta-analysis of the evidence". Bipolar Disorders 12 (1): 1–9. doi:10.1111/j.1399-5618.2009.00786.x. PMID 20148862.
- ↑ Sadock, Kaplan & Sadock 2007, p. 388.
- ↑ Roger S. McIntyre, MD, Joanna K. Soczynska, and Jakub Konarski. "Bipolar Disorder: Defining Remission and Selecting Treatment". Psychiatric Times, October 2006, Vol. XXIII, No. 11.
- ↑ Soldani, F.; Sullivan, P. F.; Pedersen, N. L. (2005). "Mania in the Swedish Twin Registry: Criterion validity and prevalence". Australian and New Zealand Journal of Psychiatry 39 (4): 235–243. doi:10.1111/j.1440-1614.2005.01559.x. PMID 15777359.
- ↑ Judd, L. L.; Akiskal, H. S. (2003). "The prevalence and disability of bipolar spectrum disorders in the US population: Re-analysis of the ECA database taking into account subthreshold cases". Journal of Affective Disorders 73 (1–2): 123–131. PMID 12507745.
- ↑ Merikangas, K. R.; Akiskal, H. S.; Angst, J.; Greenberg, P. E.; Hirschfeld, R. M. A.; Petukhova, M.; Kessler, R. C. (2007). "Lifetime and 12-Month Prevalence of Bipolar Spectrum Disorder in the National Comorbidity Survey Replication". Archives of General Psychiatry 64 (5): 543–552. doi:10.1001/archpsyc.64.5.543. PMC 1931566. PMID 17485606.
- ↑ Phelps J (2006). "Bipolar Disorder: Particle or Wave? DSM Categories or Spectrum Dimensions?". Psychiatric Times.
- ↑ Goodwin & Jamison 1990, Chapter 7.
- ↑ Ayuso-Mateos, Jose Luis. "Global burden of bipolar disorder in the year 2000". World Health Organization. Retrieved December 9, 2012.
- ↑ Kurasaki, Karen S. (2002). Asian American Mental Health: Assessment Theories and Methods. pp. 14–15.
- ↑ Christie, K. A.; Burke Jr, J. D.; Regier, D. A.; Rae, D. S.; Boyd, J. H.; Locke, B. Z. (1988). "Epidemiologic evidence for early onset of mental disorders and higher risk of drug abuse in young adults". The American Journal of Psychiatry 145 (8): 971–975. PMID 3394882.
- ↑ Goodwin & Jamison 2007, p. 1945.
- ↑ Monczor, M. (2010). "Bipolar disorder in the elderly". Vertex (Buenos Aires, Argentina) 21 (92): 275–283. PMID 21188315.
- ↑ Liddell & Scott 1980.
- ↑ 128.0 128.1 Angst, J.; Marneros, A. (2001). "Bipolarity from ancient to modern times: Conception, birth and rebirth". Journal of Affective Disorders 67 (1–3): 3–19. doi:10.1016/S0165-0327(01)00429-3. PMID 11869749.
- ↑ "at the beginning of the 19th century with Esquirol’s ‘affective monomanias’ (notably ‘lypemania’, the first elaboration of what was to become our modern depression)", Which came first, the condition or the drug?, London Review of Books, Vol. 32 No. 19, 7 October 2010, pages 31–33,
- ↑ Pichot, P. (2004). "Circular insanity, 150 years on". Bulletin de l'Academie nationale de medecine 188 (2): 275–284. PMID 15506718. (French).
- ↑ Sedler, M. J. (1983). "Falret's discovery: The origin of the concept of bipolar affective illness. Translated by M. J. Sedler and Eric C. Dessain". The American journal of psychiatry 140 (9): 1127–1133. PMID 6351641.
- ↑ Millon 1996, p. 290.
- ↑ Kraepelin, Emil (1921) Manic–depressive Insanity and Paranoia ISBN 0-405-07441-7
- ↑ Goodwin & Jamison 2007, Chapter 1.
- ↑ Goodwin & Jamison 2007, Introduction.
- ↑ Elgie, R; Morselli, PL (2007 Feb–Mar). "Social functioning in bipolar patients: the perception and perspective of patients, relatives and advocacy organizations – a review". Bipolar disorders 9 (1–2): 144–57. doi:10.1111/j.1399-5618.2007.00339.x. PMID 17391357.
- ↑ Jamison 1995.
- ↑ Joseph 2008.
- ↑ Robinson 2003, pp. 78–81.
- ↑ Robinson 2003, pp. 84–85.
- ↑ McKinley, Jesse (February 28, 1999). "Get That Man Some Prozac; If the Dramatic Tension Is All in His Head". The New York Times. Retrieved 3 March 2012.
- ↑ "The Secret Life of the Manic Depressive". BBC. 2006. Retrieved February 20, 2007.
- ↑ "Child and Adolescent Bipolar Foundation special 90210 website". CABF. 2009. Retrieved April 7, 2009.
- ↑ "EastEnders' Stacey faces bipolar disorder". BBC Press Office. May 14, 2009. Retrieved May 28, 2009.
- ↑ Tinniswood, Rachael (May 14, 2003). "The Brookie boys who shone at soap awards show". Liverpool Echo (Mirror Group Newspapers).
- ↑ 146.0 146.1 146.2 146.3 146.4 146.5 146.6 146.7 McClellan, J.; Kowatch, R.; Findling, R. L.; Work Group on Quality Issues (2007). "Practice Parameter for the Assessment and Treatment of Children and Adolescents with Bipolar Disorder". Journal of the American Academy of Child & Adolescent Psychiatry 46 (1): 107–125. doi:10.1097/01.chi.0000242240.69678.c4. PMID 17195735.
- ↑ Anthony, J.; Scott, P. (1960). "Manic–depressive Psychosis in Childhood". Journal of Child Psychology and Psychiatry 1: 53. doi:10.1111/j.1469-7610.1960.tb01979.x.
- ↑ 148.0 148.1 148.2 148.3 148.4 148.5 148.6 148.7 148.8 148.9 148.10 148.11 148.12 148.13 Leibenluft, E.; Rich, B. A. (2008). "Pediatric Bipolar Disorder". Annual Review of Clinical Psychology 4: 163–187. doi:10.1146/annurev.clinpsy.4.022007.141216. PMID 17716034.
- ↑ DSM-5 Childhood and Adolescent Disorders Work Group (2010-01-28). "Proposed change: ...to the Mood Disorders Section of DSM-V". American Psychiatric Association. Retrieved 2012-02-18.
• "APA Announces Draft Diagnostic Criteria for DSM-5" (Press release). American Psychiatric Association. 10 February 2010. Retrieved 2012-02-18. - ↑ Vasudev, A; Thomas, A (July 2010). "'Bipolar disorder' in the elderly: what's in a name?". Maturitas 66 (3): 231–5. doi:10.1016/j.maturitas.2010.02.013. PMID 20307944.
- ↑ Depp, C. A.; Jeste, D. V. (2004). "Bipolar disorder in older adults: A critical review". Bipolar Disorders 6 (5): 343–367. doi:10.1111/j.1399-5618.2004.00139.x. PMID 15383127.
- ↑ Trinh NH, Forester B (2007). "Bipolar Disorder in the Elderly: Differential Diagnosis and Treatment". Psychiatric Times 24 (14).
- Citations
- Barker, P., ed. (2003). Psychiatric and mental health nursing: the craft and caring. London: Arnold.
- Basco, Monica Ramírez (2005). The bipolar workbook: tools for controlling your mood swings. Guilford Press. ISBN 978-1-59385-162-0.
- Basco, Monica Ramirez; Rush, A. John (2005). Cognitive-Behavioral Therapy for Bipolar Disorder (Second ed.). New York: The Guilford Press. ISBN 978-1-59385-168-2. OCLC 300306925.
- Bergen, M. (1999). Riding the Roller Coaster: Living with Mood Disorders. Wood Lake Publishing. ISBN 978-1-896836-31-7.
- Brown, Malcomb R.; Basso, Michael R. (2004). Focus on Bipolar Disorder Research. Nova Science Publishers. ISBN 978-1-59454-059-2.
- Diagnostic and statistical manual of mental disorders: DSM-IV. Washington, DC: American Psychiatric Association. 1994. ISBN 978-0-89042-061-4. OCLC 29953039.
- Diagnostic and statistical manual of mental disorders: DSM-IV (4th, text revision ed.). Washington, DC: American Psychiatric Association. 2000. ISBN 978-0-89042-025-6. OCLC 742067027.
- Joseph, Chris (2008). Manicdotes: There's Madness in His Method. London: Austin & Macauley. ISBN 978-1-905609-07-9. Amazon review.
- Goodwin, F. K.; Jamison, K. R. (1990). Manic–Depressive Illness. New York: Oxford University Press. ISBN 978-0-19-503934-4.
- Goodwin, F. K.; Jamison, K. R. (2007). Manic–depressive illness: bipolar disorders and recurrent depression. Oxford University Press. ISBN 978-0-19-513579-4.
- Jamison, Kay Redfield (1995). An Unquiet Mind: A Memoir of Moods and Madness. New York: Knopf. ISBN 978-0-330-34651-1.
- Jamison, Kay R.; Goodwin, Frederick Joseph (2007). Manic–depressive illness: bipolar disorders and recurrent depression. Oxford: Oxford University Press. ISBN 978-0-19-513579-4. OCLC 70929267.
- Leahy, Robert L.; Johnson, Sheri L. (2003). Psychological Treatment of Bipolar Disorder. New York: The Guilford Press. ISBN 978-1-57230-924-1. OCLC 52714775.
- Liddell, Henry George; Scott, Robert (1980). A Greek-English Lexicon (Abridged ed.). Oxford University Press. ISBN 978-0-19-910207-5.
- Millon, Theordore (1996). Disorders of Personality: DSM-IV-TM and Beyond. New York: John Wiley and Sons. ISBN 978-0-471-01186-6.
- Robinson, D. J. (2003). Reel Psychiatry: Movie Portrayals of Psychiatric Conditions. Port Huron, Michigan: Rapid Psychler Press. ISBN 978-1-894328-07-4.
- Sadock, Benjamin J.; Kaplan, Harold I.; Sadock, Virginia A. (2007). Kaplan & Sadock's synopsis of psychiatry: behavioral sciences/clinical .... ISBN 978-0-7817-7327-0.
- Yatham, Lakshmi (2010). Bipolar Disorder. New York: Wiley. ISBN 978-0-470-72198-8.
External links
| Find more about Bipolar disorder at Wikipedia's sister projects | |
| |
Definitions and translations from Wiktionary |
| |
Media from Commons |
| |
Textbooks from Wikibooks |
| |
Database entry Q131755 on Wikidata |
- Bipolar Disorder on the Open Directory Project
- Bipolar Disorder overview from the U.S. National Institute of Mental Health website
- NICE Bipolar Disorder clinical guidelines from the U.K. National Institute for Health and Clinical Excellence website
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||