Basophil granulocyte
| Basophil granulocyte | |
|---|---|
 | |
| Basophil granulocyte | |
 | |
| Basophil | |
| Code | TH H2.00.04.1.02022 |
Basophil granulocytes, mostly referred to as basophils, are the least common of the granulocytes, representing about 0.01% to 0.3% of circulating white blood cells[citation needed].
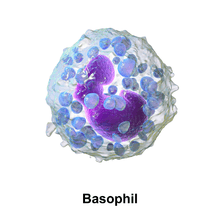
The name comes from the fact that these leukocytes are basophilic, i.e., they are susceptible to staining by basic dyes, as shown in the picture.
Basophils contain large cytoplasmic granules which obscure the cell nucleus under the microscope. However, when unstained, the nucleus is visible and it usually has 2 lobes. The mast cell, a cell in tissues, has many similar characteristics. For example, both cell types store histamine, a chemical that is secreted by the cells when stimulated in certain ways (histamine causes some of the symptoms of an allergic reaction). Like all circulating granulocytes, basophils can be recruited out of the blood into a tissue when needed.
Function

Basophils appear in many specific kinds of inflammatory reactions, particularly those that cause allergic symptoms. Basophils contain anticoagulant heparin, which prevents blood from clotting too quickly. They also contain the vasodilator histamine, which promotes blood flow to tissues. They can be found in unusually high numbers at sites of ectoparasite infection, e.g., ticks. Like eosinophils, basophils play a role in both parasitic infections and allergies.[1] They are found in tissues where allergic reactions are occurring and probably contribute to the severity of these reactions. Basophils have protein receptors on their cell surface that bind IgE, an immunoglobulin involved in macroparasite defense and allergy. It is the bound IgE antibody that confers a selective response of these cells to environmental substances, for example, pollen proteins or helminth antigens. Recent studies in mice suggest that basophils may also regulate the behavior of T cells and mediate the magnitude of the secondary immune response.[2]
Immunophenotyping of basophils
Basophils of mouse and human have consistent immunophenotypes as follows: FcεRI+, CD123, CD49b(DX-5)+, CD69+, Thy-1.2+, 2B4+, CD11bdull, CD117(c-kit)–, CD24–, CD19–, CD80–, CD14–, CD23–, Ly49c–, CD122–, CD11c–, Gr-1–, NK1.1–, B220–, CD3–, γδTCR–, αβTCR–, α4 and β4-integrin negative.[3]
Recently, Heneberg [4] proposed that basophils may be defined as the cellular population positive for CD13, CD44, CD54, CD63, CD69, CD107a, CD123, CD164, CD193/ CCR3, CD203c, TLR-4, and FcεRI. When activated, some additional surface markers are known to be upregulated (CD13, CD107a, CD164), or surface-exposed (CD63, and the ectoenzyme CD203c).[4]
Secretions
When activated, basophils degranulate to release histamine, proteoglycans (e.g. heparin and chondroitin), and proteolytic enzymes (e.g. elastase and lysophospholipase). They also secrete lipid mediators like leukotrienes, and several cytokines. Histamine and proteoglycans are pre-stored in the cell's granules while the other secreted substances are newly generated. Each of these substances contributes to inflammation. Recent evidence suggests that basophils are an important source of the cytokine, interleukin-4, perhaps more important than T cells. Interleukin-4 is considered one of the critical cytokines in the development of allergies and the production of IgE antibody by the immune system. There are other substances that can activate basophils to secrete which suggests that these cells have other roles in inflammation.[5]
The degranulation of basophils can be investigated in vitro by using flow cytometry and the so-called basophil-activation-test (BAT). Especially, in the diagnosis of allergies including of drug reactions (e.g. induced by contrast medium), the BAT of is great impact.[6]
Basopenia (a low basophil count) is difficult to demonstrate as the normal basophil count is so low; it has been reported in association with autoimmune urticaria[7] (a chronic itching condition). Basophilia is also uncommon but may be seen in some forms of leukaemia or lymphoma.
References
- ↑ Voehringer D. 2009. Trends in Parasitology.
- ↑ Nakanishi, Kenji (December 2010). "Basophils as APC in Th2 response in allergic inflammation and parasite infection". Current Opinion in Immunology 22 (6): 814–820. doi:10.1016/j.coi.2010.10.018.
- ↑ Schroeder JT (2009). "Basophils beyond effector cells of allergic inflammation." Adv Immunol 101:123-161, PMID 19231594, doi:10.1016/S0065-2776(08)01004-3.
- ↑ 4.0 4.1 Heneberg, Petr (2011). "Mast cells and basophils: trojan horses of conventional lin- stem/progenitor cell isolates". Current Pharmaceutical Design 17 (34): 3753–3771. PMID 22103846. Retrieved 21 May 2012.
- ↑ Janeway CA, Jr. et al. (2001). Immunobiology. (electronic full text via NCBI Bookshelf) (5th ed.). Garland Publishing. ISBN 0-8153-3642-X.
- ↑ Böhm I et al. Pilot study on basophil activation induced by contrast medium. Fundam Clin Pharmacol 2011;25:267 - 276
- ↑ Grattan CE, Dawn G, Gibbs S, Francis DM (Mar 2003). "Blood basophil numbers in chronic ordinary urticaria and healthy controls: diurnal variation, influence of loratadine and prednisolone and relationship to disease activity". Clin Exp Allergy 33 (3): 337–41. doi:10.1046/j.1365-2222.2003.01589.x. PMID 12614448.
Additional images
-

Blood cell lineage
-

Alternate stain of a basophil
External links
| Wikimedia Commons has media related to basophils. |
| |||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||