Ventilation/perfusion ratio
In respiratory physiology, the ventilation/perfusion ratio (or V/Q ratio) is a measurement used to assess the efficiency and adequacy of the matching of two variables:[1] It is defined as: the ratio of the amount of air reaching the alveoli to the amount of blood reaching the alveoli.
- "V" – ventilation – the air which reaches the alveoli
- "Q" – perfusion – the blood which reaches the alveoli
These two variables constitute the main determinants of the blood oxygen concentration. In fact since V determines the quantity of oxygen mass reaching the alveoli per minute (g/min) and Q expresses the flow of blood in the lungs (l/min), the V/Q ratio refers to a concentration (g/l).
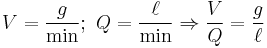
Usually, however, the density of the gas (in g/l) can be used to convert the V/Q into a dimensionless ratio, and this is how it is most often expressed.
The V/Q ratio can be measured with a ventilation/perfusion scan.
Contents |
Physiology
Ideally, the oxygen provided via ventilation would be just enough to saturate the blood fully. In the typical adult, 1 liter of blood can hold about 200 mL of oxygen; 1 liter of dry air has about 210 mL of oxygen. Therefore, under these conditions, the ideal ventilation perfusion ratio would be about 0.95. If one were to consider humidified air (with less oxygen), then the ideal v/q ratio would be in the vicinity of 1.0, thus leading to concept of ventilation-perfusion equality or ventilation-perfusion matching. This matching may be assessed in the lung as a whole, or in individual or in sub-groups of gas-exchanging units in the lung. On the other side Ventilation-perfusion mismatch is the term used when the ventilation and the perfusion of a gas exchanging unit are not matched.
The actual values in the lung vary depending on the position within the lung. If taken as a whole, the typical value is approximately 0.8.[2]
Because the lung is centered vertically around the heart, part of the lung is superior to the heart, and part is inferior. This has a major impact on the V/Q ratio:[3]
- apex of lung – higher
- base of lung – lower
In a subject standing in orthostatic position (upright) the apex of the lung shows higher V/Q ratio, while at the base of the lung the ratio is lower but nearer to the optimal value for reaching adequate blood oxygen concentrations. The main reason for lower V/Q ratios at the base is that both ventilation and perfusion increase when going from the apex to the base, but Q does it more strongly thus lowering the V/Q ratio. The principal factor involved in the genesis of V/Q dishomogeneity between the apex and the base of the lung is gravity (this is why V/Q ratios change in positions other than the orthostatic one).
Ventilation
Gravity and lung’s weight act on ventilation by increasing pleural pressure at the base (making it less negative) and thus reducing the alveolar volume. The lowest part of the lung in relation to gravity is called the dependent region. At the dependent region smaller volumes mean the alveoli are more compliant (more distensible) and so capable of wider oxygen exchanges with the external environment. The apex, though showing a higher oxygen partial pressure, ventilates less efficiently since its compliance is lower and so smaller volumes are exchanged.
Perfusion
The impact of gravity on pulmonary perfusion expresses itself as the hydrostatic pressure of the blood passing through the branches of the pulmonary artery in order to reach the apical and basal district of the lung, acting respectively against or synergistically with the pressure developed by the right ventricle. Thus at the apex of the lung the resulting pressure can be insufficient for developing a flow (which can be sustained only by the negative pressure generated by venous flow towards the left atrium) or even for preventing the collapse of the vascular structures surrounding the alveoli, while the base of the lung shows an intense flow due to the higher resulting pressure.
Pathology
Extreme alterations of V/Q
- An area with no ventilation (and thus a V/Q of zero) is termed "shunt."
- An area with no perfusion (and thus a V/Q undefined though approaching infinity) is termed dead space.[4]
Pathophysiology
- A lower V/Q ratio (with respect to the expected value for a particular lung area in a defined position) impairs pulmonary gas exchange and is a cause of low arterial partial pressure of oxygen (paO2). Excretion of carbon dioxide is also impaired but a rise in arterial partial pressure of carbon dioxide (paCO2) is very uncommon because this leads to respiratory stimulation and the resultant increase in alveolar ventilation returns paCO2 to within the normal range. These abnormal phenomena are usually seen in chronic bronchitis, asthma and acute pulmonary edema.
- A high V/Q ratio increases paO2 and decreases paCO2. This finding is typically associated with pulmonary embolism (where blood circulation is impaired by an embolus). Ventilation is wasted, as it fails to oxygenate any blood. A high V/Q can also be observed in COPD as a maladaptive ventilatory overwork of the undamaged lung parenchyma.
References
External links
- Overview at anaesthesiauk.com
- MeSH ventilation-perfusion+ratio
- Physiology at MCG 4/4ch4/s4ch4_24
- RT Corner (Educational Site for RT's and Nurses) at rtcorner.net
|
|||||||||||||||||||||||||||||