Electrogastrogram
An electrogastrogram (EGG) is a graphic produced by an electrogastrograph, which records the electrical signals that travel through the stomach muscles and control the muscles' contractions. An electrogastroenterogram (or gastroenterogram) is a similar procedure, which writes down electric signals not only from the stomach, but also from intestines.
These names are made of different parts: electro, because it is related to electrical activity, gastro, Greek for stomach, entero, Greek for intestines, gram, a Greek root meaning "to write".
An electrogastrogram and a gastroenterogram are similar in principle to an electrocardiogram (ECG) in that sensors on the skin detect electrical signals indicative of muscular activity within. Where the electrocardiogram detects muscular activity in various regions of the heart, the electrogastrogram detects the wave-like contractions of the stomach (peristalsis).
Walter C. Alvarez pioneered early studies of electrogastrography in 1921-22.[1]
Contents |
Physiological basis of electrogastroenterography
Motility of GI tract is results from coordinated contractions of smooth muscle, which in turn derive from two basic patterns of electrical activity across the membranes of smooth muscle cells — slow waves and action potentials.[2] Slow waves are initiated by pacemakers — the interstitial cells of Cajal (ICC). Slow wave frequency varies in the different organs of the GI tract and is characteristic for that organ. They set the maximum frequency at which the muscle can contract:
- stomach — about 3 waves in a minute,
- duodenum — about 12 waves in a minute,
- ileum — about 8 waves in a minute,
- rectum — about 17 waves in a minute.[3]
- jejunum — about 11 waves in a minute.[4]
The electrical activity of the GI tract can be subdivided into two categories: electrical control activity (ECA) and electrical response activity (ERA). ECA is characterized by regularly recurring electrical potentials, originating in the gastric pacemaker located in the body of stomach. The slow waves are not a direct reason of peristalsis of a GI tract, but a correlation between deviations of slow waves from norm and motility abnormalities however is proved.[5]
Cutaneous electrogastrography
Electrogastrogram can be made from the gastrointestinal mucosa, serosa, or skin surface. The cutaneous electrogastrography and provides an indirect representation of the electrical activity but it is much easier and therefore cutaneous electrogastrography has been used most frequently.
Several EGG signals are recorded from various standardized positions on the abdominal wall and to select the one with the highest amplitude for further analysis. For this purpose usually use three or more Ag-AgCl electrodes.[6] Recordings are made both fasting (usually 30 minutes) and after a meal (usually 60 minutes) with the patient lying quietly. Deviations from the normal frequency may be referred to as bradygastria or tachygastria.
In normal individuals the power of the electrical signals increases after the meal. In patients with abnormalities of stomach motility, the rhythm often is irregular or there is no postprandial increase in electrical power.
Bradygastria, normogastria and tachygastria
Terms bradygastria and tachygastria are used at the description of deviations of frequency of an electric signal from slow waves are initiated by pacemaker in the stomach from normal frequency of 3 cycles per minute.
A bradygastria is defined, how decreased rate of electrical activity in the stomach, as less than 2 cycles per minute for at least 1 minute.
A tachygastria is defined, how increased rate of electrical activity in the stomach, as more than 4 cycles per minute for at least 1 minute.
A bradygastria and tachygastria may be associated with nausea, gastroparesis, irritable bowel syndrome, and functional dyspepsia.[7]
CPT and HCPCS codes for electrogastrography
There are following Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) codes (maintained by the American Medical Association) for cutaneous electrogastrography:[8]
| CPT/HCPCS-code | Procedure |
|---|---|
| 91132 | Electrogastrography, diagnostic, transcutaneous |
| 91133 | Electrogastrography, diagnostic, transcutaneous; with provocative testing |
Electrogastroenterography
An electrogastroenterography (EGEG) is based that different organs of a GI tract give different frequency slow wave.
| Organ of gastrointestinal tract | Investigated range (Hz) | Frequency number (i) |
|---|---|---|
| Large intestine | 0.01 – 0.03 | 5 |
| Stomach | 0.03 – 0.07 | 1 |
| Ileum | 0.07 – 0.13 | 4 |
| Jejunum | 0.13 – 0.18 | 3 |
| Duodenum | 0.18 – 0.25 | 2 |
EGEG electrodes are as much as possible removed from a stomach and an intestines — usaually three electrodes are placed on the extremities. It allows to receive stabler and comparable results.
The computer analysis of electrogastroenterograms
An electrogastroenterography analysis program calculate[9]
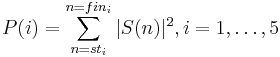
- P(i) — capacities of an electric signal separately from each of organ of GI tract in corresponding range of frequencies:
where S(n) — spectral components in the rank from sti to fini (defined by received investigated range of this organ of GI tract) by Discrete Fourier transform of the electric signal from GI tract.
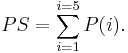
- PS — the general (total) capacity of an electric signal from five parts of GI tract:
- P(i)/PS — the relative electric activity.
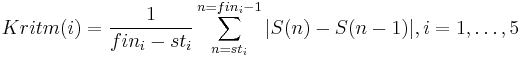
- Kritm(i) — rhythm factor
EGEG parametres for normal patients:[9]
| Organ of gastrointestinal tract | Electric activity P(i)/PS | Rhythm factor Kritm(i) | P(i)/P(i+1) |
|---|---|---|---|
| Stomach | 22.4±11.2 | 4.85±2.1 | 10.4±5.7 |
| Duodenum | 2.1±1.2 | 0.9±0.5 | 0.6±0.3 |
| Jejunum | 3.35±1.65 | 3.43±1.5 | 0.4±0.2 |
| Ileum | 8.08±4.01 | 4.99±2.5 | 0.13±0.08 |
| Large intestine | 64.04±32.01 | 22.85±9.8 | — |
Not solved problems
There are some lacks limiting an electrogastroenterography use in practice:
- an absence of a standard technique of performance peripheral electrogastroenterography,
- an absence of a standard norms of electrophysiological parametres of bioelectric activity GT tract,
- an impossibility of an estimation of change of motility abnormalities during the concrete moments of time on local sites of GI tract.
Other updatings of electrogastrography
- 24-hour electrogastrography and electrogastroenterography.
- The joint electrogastroenterography with 24-hours pH-metry.
- Wavelet analysis of electrogastroenterogram.[10]
- Telemetry capsule for the EGG monitoring in a stomach and an intestines.[11]
Clinical applications of electrogastrography and gastroenterography
Electrogastrography or gastroenterography used when a patient is suspected of having a motility disorder, which can be shown, as recurrent nausea and vomiting, signs that the stomach is not emptying food normally. The clinical use of electrogastrography has been most widely evaluated in patients with gastroparesis and functional dyspepsia.
See also
Sources
- Stern, Robert Mitchell; Koch, Kenneth (2004). Handbook of electrogastrography. Oxford [Oxfordshire]: Oxford University Press. ISBN 0-19-514788-X.
- Mintchev M. Selected Topics on Electrogastrography: Electrical phenomena in the human stomach.
References
- ^ Alvarez W. C. (April 15, 1922). "The electrogastrogram and what it shows". J Am Med Assoc. 78 (15): 1116–19. doi:10.1001/jama.1922.02640680020008. http://jama.ama-assn.org/cgi/content/summary/78/15/1116.
- ^ Bowen R. (November 23, 1996). "Electrophysiology of Gastrointestinal Smooth Muscle". http://www.vivo.colostate.edu/hbooks/pathphys/digestion/basics/slowwaves.html. Retrieved February 12, 2008.
- ^ [Gastrointestinal Physiology. Gastrointestinal Motility "3"]. GI Smooth Muscle Electrophysiology: Slow Waves (Basal Electric Rhythm). p. 5. Gastrointestinal Physiology. Gastrointestinal Motility.
- ^ Waldhausen, JH; Shaffrey, ME; Skenderis Bs, 2nd; Jones, RS; Schirmer, BD (June 1990). "Gastrointestinal myoelectric and clinical patterns of recovery after laparotomy". Ann. Surg. 211 (6): 777–84; discussion 785. doi:10.1097/00000658-199006000-00018. PMC 1358137. PMID 2357140. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1358137.
- ^ Parkman HP, Hasler WL, Barnett JL, Eaker EY (April 2003). "Electrogastrography: a document prepared by the gastric section of the American Motility Society Clinical GI Motility Testing Task Force". Neurogastroenterol. Motil. 15 (2): 89–102. doi:10.1046/j.1365-2982.2003.00396.x. PMID 12680908. http://www3.interscience.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=1350-1925&date=2003&volume=15&issue=2&spage=89.
- ^ Stendal, Charlotte (1997). Practical guide to gastrointestinal function testing. Oxford: Blackwell Science. ISBN 0-632-04918-9.
- ^ MediLexicon. Definisions of "Bradygastria" and "Tachygastria".
- ^ Federal Register. Vol. 72, No. 148 /Thursday, August 2, 2007/ Proposed Rules, 42997.
- ^ a b Stupin V. A., et al. Peripheral Electrogastroenterography in Clinical Practice // Лечащий Врач.-2005.-№ 2.-С. 60-62 (Russian).
- ^ Tokmakçi M (August 2007). "Analysis of the electrogastrogram using discrete wavelet transform and statistical methods to detect gastric dysrhythmia". J Med Syst 31 (4): 295–302. doi:10.1007/s10916-007-9069-9. PMID 17685154. http://www.ingentaconnect.com/content/klu/joms/2007/00000031/00000004/00009069.
- ^ Jung E.S., et al. Design and Implementation of the Telemetry Capsule for Measuring of Electrogastrography. Proceedings of the 24th IASTED international conference on Biomedical engineering. Innsbruck, Austria, pp. 209-213, 2006, ISBN 0-88986-578-7.
|
|||||||||||||||||