Differential diagnosis
| Differential diagnosis | |
|---|---|
| Intervention | |
| MeSH | D003937 |
A differential diagnosis (sometimes abbreviated DDx, ddx, DD, D/Dx, or ΔΔ) is a systematic diagnostic method used to identify the presence of an entity where multiple alternatives are possible (and the process may be termed differential diagnostic procedure), and may also refer to any of the included candidate alternatives (which may also be termed candidate condition). This method is essentially a process of elimination, or at least, rendering of the probabilities of candidate conditions to negligible levels. In this sense, probabilities are, in fact, imaginative parameters in the mind or hardware of the diagnostician or system, while in reality the target (such as a patient) either has a condition or not with an actual probability of either 0 or 100%.
Differential diagnostic procedures are used by physicians, psychiatrists, and other trained medical professionals to diagnose the specific disease in a patient, or, at least, to eliminate any imminently life-threatening conditions.
Differential diagnosis can be regarded as implementing aspects of the hypothetico-deductive method in the sense that the potential presence of candidate diseases or conditions can be viewed as hypotheses which are further processed as being true or false.
Contents |
General components
There are various methods of performing a differential diagnostic procedure, but in general, it is based on the idea that one begins by considering the most common diagnosis first: a head cold versus meningitis, for example. As a reminder, medical students are taught the adage, "When you hear hoofbeats, look for horses, not zebras," which means look for the simplest, most common explanation first. Only after the simplest diagnosis has been ruled out should the clinician consider more complex or exotic diagnoses.
A differential diagnostic procedure can be performed by that the doctor first gathers all information about the patient and create a symptoms list. The list can be in writing or in the doctor's head, as long as he or she makes a list. Second, the doctor should make a list of all possible causes (also termed "candidate conditions") of the symptoms. Again, this can be in writing or in the doctor's head but it must be done. Third, the doctor should prioritize the list by placing the most urgently dangerous possible cause of the symptoms at the top of the list. Fourth, the doctor should rule out or treat the possible causes beginning with the most urgently dangerous condition and working his or her way down the list. "Rule out" practically means to use tests and other scientific methods to render a condition of clinically negligible probability of being the cause.
In some cases, there will remain no diagnosis; this suggests the physician has made an error, or that the true diagnosis is unknown to medicine. Removing diagnoses from the list is done by making observations and using tests that should have different results, depending on which diagnosis is correct.
Mnemonics are routinely taught to medical students to ensure that all possible pathological processes are considered, for example VINDICATE: Vascular, Inflammatory, Neoplastic, Degenerative/Deficiency, Idiopathic/Intoxication, Congenital, Autoimmune/Allergic, Traumatic, Endocrine[1]
Specific methods
There are several methods for performing a differential diagnostic procedure, and several variants among those in turn. Furthermore, a differential diagnostic procedure can be used concomitantly or switchingly with protocols, guidelines or other diagnostic procedures (such as pattern-recognition or using medical algorithms).
For example, in case of medical emergency, there may not be enough time to do any detailed calculations or estimations of different probabilities, in which case the ABC protocol may be more appropriate. At a later, less acute, situation, there may be a switch to a more comprehensive differential diagnostic procedure.
The differential diagnostic procedure may be easier in the finding of a pathognomonic sign or symptom, in which it is almost certain that the target condition is present, and in the absence of finding a sine qua non sign or symptom, in which case it is almost certain that the target condition is absent. In reality, however, the subjective probability of the presence of a condition is never exactly 100% or 0%, so in reality the procedure is usually aimed at specifying the various probabilities in order to form indications for further actions.
By epidemiology
One method of performing a differential diagnosis by epidemiology aims to estimate the probability of each candidate condition by comparing their probabilities to have occurred in the first place in the individual. It is based on probabilities related both to the presentation (such as pain) and probabilities of the various candidate conditions (such as diseases).
Theory
The probability that a presentation or condition would have occurred in the first place in an individual is not same as the probability that the presentation or condition has occurred in the individual, because the presentation has occurred by 100% certainty in the individual. Yet, the contributive probability fractions of each condition are assumed to be the same, relatively:
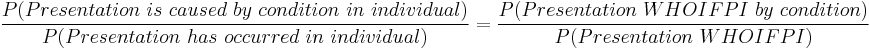
, where:
- P(Presentation is caused by condition in individual) is the probability that the presentation is caused by condition in the individual
- condition without further specification refers to any candidate condition
- P(Presentation has occurred in individual) is the probability that the presentation has occurred in the individual, which is 100%
- P(Presentation WHOIFPI by condition) is the probability that the presentation Would Have Occurred In the First Place in the Individual by condition
- P(Presentation WHOIFPI) is the probability that the presentation Would Have Occurred In the First Place in the Individual
P(Presentation has occurred in individual) is 100% and can therefore be replaced by 1, and can be ignored since division by 1 does not make any difference:
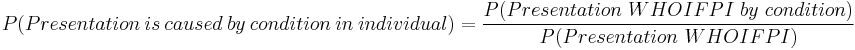
The total probability of the presentation to have occurred in the individual can be approximated as the sum of the individual candidate conditions:
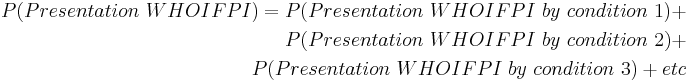
Also, the probability of the presentation to have been caused by any candidate condition is proportional to the probability of the condition, depending on what rate it causes the presentation:

, where:
- P(Presentation WHOIFPI by condition) is the probability that the presentation Would Have Occurred In the First Place in the Individual by condition
- P(Condition WHOIFPI) is the probability that the condition Would Have Occurred In the First Place in the Individual
- rCondition→presentation is the rate for which condition causes the presentation, that is, the fraction of people with condition that manifest with the presentation
The probability that a condition would have occurred in the first place in an individual is approximately equal to that of a population that is as similar to the individual as possible except for the current presentation, compensated where possible by relative risks given by known risk factor that distinguish the individual from the population:
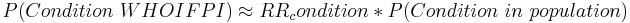
, where:
- P(Condition WHOIFPI) is the probability that the condition Would Have Occurred In the First Place in the Individual
- RRcondition is the relative risk for condition conferred by known risk factors in the individual that are not present in the population
- P(Condition in population) is the probability that the condition occurs in a population that is as similar to the individual as possible except for the presentation
The following table demonstrates how these relations can be made for a series of candidate conditions:
| Candidate condition 1 | Candidate condition 2 | Candidate condition 3 | |
| P(Condition in population) | P(Condition 1 in population) | P(Condition 2 in population) | P(Condition 3 in population) |
| RRcondition | RR 1 | RR 2 | RR 3 |
| P(Condition WHOIFPI) | P(Condition 1 WHOIFPI) | P(Condition 2 WHOIFPI) | P(Condition 3 WHOIFPI) |
| rCondition→presentation | rCondition 1→presentation | rCondition 2→presentation | rCondition 3→presentation |
| P(Presentation WHOIFPI by condition) | P(Presentation WHOIFPI by condition 1) | P(Presentation WHOIFPI by condition 2) | P(Presentation WHOIFPI by condition 3) |
| P(Presentation WHOIFPI) = the sum of the probabilities in row just above | |||
| P(Presentation is caused by condition in individual) | P(Presentation is caused by condition 1 in individual) | P(Presentation is caused by condition 2 in individual) | P(Presentation is caused by condition 3 in individual) |
One additional "candidate condition" is the instance of there being no abnormality, and the presentation is only a (usually relatively unlikely) appearance of a basically normal state. Its probability in the population (P(No abnormality in population)) is complementary to the sum of probabilities of "abnormal" candidate conditions.
Example
This example case is made to demonstrate how this method may be applied, but does not intend to be a guideline for handling similar cases in reality. Also, the example uses relatively specified numbers with sometimes several decimals, while in reality there are often simply rough estimations, such as of likelihoods being "very high", "high", "low" or "very low", but still using the general principles of the method.
For an individual (who becomes the "patient" in this example), a blood test of, for example, serum calcium shows a result just above the standard reference range, which, by most definitions, classifies as hypercalcemia, which becomes the "presentation" in this case. A physician (who becomes the "diagnostician" in this example), who does not currently see the patient, gets to know about his finding.
By practical reasons, the physician considers that there is enough test indication to have a look at the patient’s medical records. For simplicity, let’s say that the only information given in the medical records is a family history of primary hyperparathyroidism (here abbreviated as PH), which may explain the finding of hypercalcemia. For this patient, let’s say that the resultant hereditary risk factor is estimated to confer a relative risk of 10 (RRPH = 10).
The physician considers that there is enough motivation to perform a differential diagnostic procedure for the finding of hypercalcemia. The main causes of hypercalcemia are primary hyperparathyroidism (PH) and cancer, so for simplicity, the list of candidate conditions that the physician could think of can be given as:
- Primary hyperparathyroidism (PH)
- Cancer
- Other diseases that the physician could think of (which is simply termed "other conditions" for the rest of this example)
- No disease (or no abnormality), and the finding is caused entirely by statistical variability
The the probability that primary hyperparathyroidism (PH) would have occurred in the first place in the individual (P(PH WHOIFPI)) can be calculated as follows:
Let’s say that the last blood test taken by the patient was half a year ago and was normal, and that the incidence of primary hyperparathyroidism in a general population that appropriately matches the individual (except for the presentation and mentioned heredity) is 1 in 4000 per year. Ignoring more detailed retrospective analyses (such as including speed of disease progress and lag time of medical diagnosis), the time-at-risk for having developed primary hyperparathyroidism can roughly be regarded as being the last half year, because a previously developed hypercalcemia would probably have been caught up by the previous blood test. This corresponds to a probability of primary hyperparathyroidism (PH) in the population of:
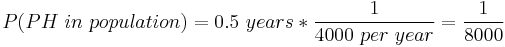
With the relative risk conferred from the family history, the probability that primary hyperparathyroidism (PH) would have occurred in the first place in the individual given from the currently available information becomes:
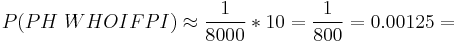
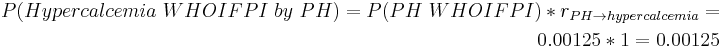
Primary hyperparathyroidism can be assumed to cause hypercalcemia in essentially 100% of the time (rPH &rarr hypercalcemia = 1), so this independently calculated probability of primary hyperparathyroidism (PH) can be assumed to be the same as the probability of being a cause of the presentation:
For cancer, the same time-at-risk is assumed for simplicity, and let’s say that the incidence of cancer in the area is estimated at 1 in 250 per year, giving an population probability of cancer of:
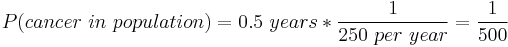
For simplicity, let’s say that any association between a family history of primary hyperparathyroidism and risk of cancer is ignored, so the relative risk for the individual to have contracted cancer in the first place is similar to that of the population (RRcancer = 1):
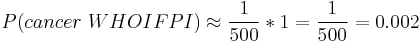
However, hypercalcemia only occurs in, very approximately, 10% of cancers,[2] (rcancer &rarr hypercalcemia = 0.1), so:
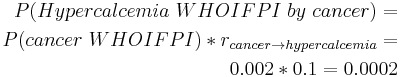
The probabilities that hypercalcemia would have occurred in the first place by other candidate conditions can be calculated in a similar manner. However, for simplicity, let’s say that that the probability that any of these would have occurred in the first place is calculated to be 0.0005 in this example.
For the instance of there being no disease, the corresponding probability in the population is complementary to the sum of probabilities for other conditions:
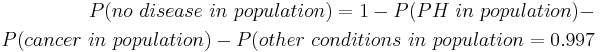
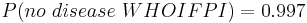
The probability that the individual would be healthy in the first place can be assumed to be the same:
The rate at which the case of no abnormal condition still ends up in a measurement of serum calcium of being above the standard reference range (thereby classifying as hypercalcemia) is, by the definition of standard reference range, less than 2.5%. However, this probability can be further specified by considering how much the measurement deviates from the mean in the standard reference range. Let’s say that the serum calcium measurement was 1.30 mmol/L, which, with a standard reference range established at 1.05 to 1.25 mmol/L, corresponds to a standard score of 3 and a corresponding probability of 0.14% that such degree of hypercalcemia would have occurred in the first place in the case of no abnormality:
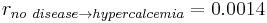
Subsequently, the probability that hypercalemia would have resulted from no disease can be calculated as:
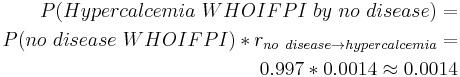
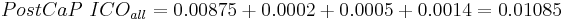
The probability that hypercalcemia would have occurred in the first place in the individual can thus be calculated as:
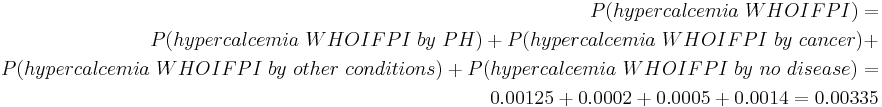
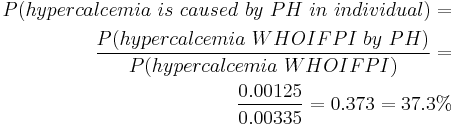
Subsequently, the probability that hypercalcemia is caused by primary hyperparathyroidism (PH) in the individual can be calculated as:
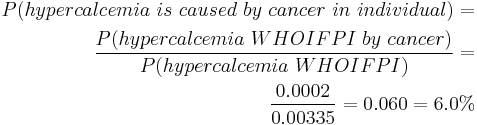
Similarly, the probability that hypercalcemia is caused by cancer in the individual can be calculated as:
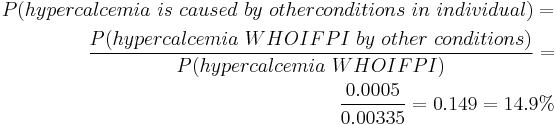
, and for other candidate conditions:
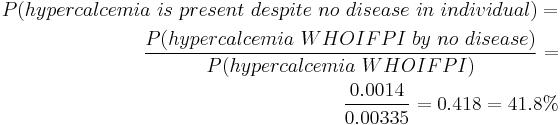
, and the probability that there actually is no disease:
For clarification, these calculations are given as the table in the method description:
| PH | Cancer | Other conditions | No disease | |
| P(Condition in population) | 0.000125 | 0.002 | - | 0.997 |
| RRx | 10 | 1 | - | - |
| P(Condition WHOIFPI) | 0.00125 | 0.002 | - | - |
| rCondition →hypercalcemia | 1 | 0.1 | - | 0.0014 |
| P(hypercalcemia WHOIFPI by condition) | 0.00125 | 0.0002 | 0.0005 | 0.0014 |
| P(hypercalcemia WHOIFPI) = 0.00335 | ||||
| P(hypercalcemia is caused by condition in individual) | 37.3% | 6.0% | 14.9% | 41.8% |
Thus, this method estimates that the probabilities that the hypercalcemia is caused by primary hyperparathyroidism, cancer, other conditions or no disease at all are 37.3%, 6.0%, 14.9% and 41.8%, respectively, which may be used in estimating further test indications.
This case is continued in the example of the method described in the next section.
By independently and profile-relative probabilities
The procedure of differential diagnosis can become extremely complex if it would fully take additional tests and treatments into consideration. One method that is somewhat a tradeoff between being clinically perfect and being relatively simple to calculate is one that assigns two kinds of likelihood parameters for each disease or other condition that is included in the list of differential diagnoses; one independently calculated odds in favor of the condition, and one probability that is relative to the entire profile of conditions and their odds respectively.
Theory
For each candidate condition, this method first estimates an independently calculated odds in favor, which initially corresponds to the probability that the individual would have developed the condition in the first place, as used in the previously mentioned method using epidemiology. If previously calculated as a probability, it can be converted to odds in favor by:
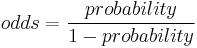
These independently calculated odds in favor, in the format of their value to one, are summed together in this method, and the resultant value is be used to estimate a profile-relative probability for each candidate condition, as follows:
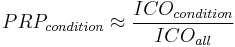
, where:
- PRPcondition is the profile-relative probability of a condition
- ICOcondition is the independently calculated odds in favor of a condition as a cause of the presentation
- ICOall is the sum of all independently calculated odds in favor, of all candidate conditions
The profile-relative probabilities correspond to the probabilities of each condition of causing the presentation (P(Presentation is caused by condition in individual)), and are more clinically useful than the individually calculated odds, similarly to that the probabilities of conditions having occurred are more clinically useful than that the conditions would have occurred in the first place as mentioned in the epidemiology-based method. Therefore, it is the profile-relative probabilities that are used for estimating the indications for further medical tests, treatments or other actions in this method.
If there is an indication for a test, and it returns with a result, then the procedure is repeated by making new estimations of independently calculated odds for candidate conditions where they have likely changed, in turn likely resulting in a different sum of all independently calculated odds, and thereby different profile-relative probabilities. With different profile-relative probabilities, the indications for further tests, treatments or other actions have changed as well, and are therefore estimated anew, and so the procedure can be repeated until an end point where there no longer is any indication for currently performing further actions. Such an end point mainly occurs when one candidate condition becomes so certain that no test can be found that is powerful enough to change the relative probability-profile enough to motivate any current change in further actions. Tactics for reaching such an end point with as few tests as possible includes making tests with high specificity for conditions of already outstandingly high profile-relative probability, because the high likelihood ratio positive for such tests is very high, bringing all less likely conditions to relatively lower probabilities. Alternatively, tests with high sensitivity for competing candidate conditions, such tests have a high likelihood ratio negative, potentially bringing the probabilities for competing candidate conditions to negligible levels. If such negligible probabilities are achieved, these conditions can be decided to be ruled out, and the differential diagnostic procedure continues with only the remaining candidate conditions.
Comparing to the previously mentioned epidemiology-based method, this method can be used with much more ease for including additional tests. However, this method is not so good at establishing initial probabilities, but can, on the other hand, be a good complementing method upon which to continue previously calculated probabilities from, for example, an epidemiology-based method.
Example
This example continues for the same patient as in the example for the epidemiology-based method. As with the previous example of epidemiology-based method, this example case is made to demonstrate how this method may be applied, but does not intend to be a guideline for handling similar cases in reality. Also, the example uses relatively specified numbers, while in reality there are often just rough estimations.
The probabilities that the presentation would have occurred in the first place for each condition ("P(Presentation WHOIFPI by condition) can initially be set as the individually calculated probabilities, and the resultant probabilities of each condition of causing the presentation can initially be set as the profile relative probabilities:
| PH | Cancer | Other conditions | No disease | |
| Independently calculated probability (ICP) | 0.00125 | 0.0002 | 0.0005 | 0.0014 |
| Profile-relative probability (PRP) | 37.3% | 6.0% | 14.9% | 41.8% |
The condition of highest profile-relative probability (except “no disease”) is primary hyperparathyroidism (PH), but cancer is still of major concern, because if it is the actual causative condition for the hypercalcemia, then the choice of whether to treat or not likely means life or death for the patient, in effect potentially putting the indication at a similar level for further tests for both of these conditions. Because the
Here, let’s say that the physician considers the profile-relative probabilities of being of enough concern to indicate to send the patient a call for a doctor's visit, with an additional visit to the medical laboratory for an additional blood test complemented with further analyses, including parathyroid hormone for the suspicion of primary hyperparathyroidism.
For simplicity, let’s say that the doctor first receives the result for the parathyroid hormone analysis, and that it showed a parathyroid hormone level that is elevated relatively to what would be expected by the calcium level.
Such a constellation can be estimated to have a sensitivity of approximately 70% and a specificity of approximately 90% for primary hyperparathyroidism. [3] This confers a likelihood ratio positive of 7 for primary hyperparathyroidism.
The target value in this method is the independently calculated odds in favor of primary hyperparathyroidism, denoted Pre-CaP because it corresponds to before (Latin preposition prae means before) the calcium- and parathyroid hormone related test.
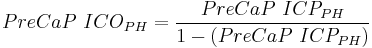
, where:
- PreCaP ICOPH is the independently calculated odds in favor of primary hyperparathyroidism before the calcium and parathyroid hormone related test
- ICPPH is the independently calculated probability for primary hyperparathyroidism before the calcium and parathyroid hormone related test, previously given as 0.00125, resulting in:
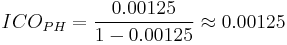
Here, the difference between odds and probability is negligible because the value is very low.
The same can be done for the other candidate conditions, also resulting in negligible differences between odds and probabilities (although such differences can be substantial at higher values):
| PH | Cancer | Other conditions | No disease | |
| Independently calculated probability (ICP) | 0.00125 | 0.0002 | 0.0005 | 0.0014 |
| Pre-CaP ICO | 0.00125 | 0.0002 | 0.0005 | 0.0014 |
With the likelihood ratio positive of 7 for the calcium- and parathyroid hormone related test, the post-test odds is calculated as:
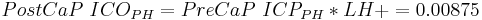
, where:
- PostCaP ICOPH is the independently calculated odds for primary hyperparathyroidism after the calcium and parathyroid hormone related test, given at 0.00125
- PreCaP ICOPH is the independently calculated odds in favor of primary hyperparathyroidism before the calcium and parathyroid hormone related test
- LH+ is the likelihood ratio positive for the test
Subsequently, the sum of all independently calculated odds after the calcium- and parathyroid hormone related test becomes:
The profile-relative probability for primary hyperparathyroidism (PH) after this test is calculated as:
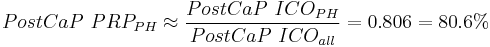
, where:
- PostCaP PRPPH is the profile-relative probability for primary hyperparathyroidism after the calcium and parathyroid hormone related test
- PostCaP ICOall is the sum of all independently calculated odds after the calcium- and parathyroid hormone related test
- PostCaP ICOPH is the independently calculated odds for primary hyperparathyroidism after the calcium and parathyroid hormone related test
These are calculated similarly for the other conditions, but in this case with independently calculated post-test odds being same as pre-test odds, resulting as:
| PH | Cancer | Other conditions | No disease | |
| PostCaP ICO | 0.00875 | 0.0002 | 0.0005 | 0.0014 |
| PostCaP PRP | 80.6% | 1.8% | 4.6% | 12.9% |
These “new” percentages, including a profile-relative probability of 80% for primary hyperparathyroidism, underlie any indications for further tests, treatments or other actions. In this case, let's say that the physician continues the plan for the patient to attend a doctor's visit for further checkup, especially focused at primary hyperparathyroidism.
A doctor's visit can, theoretically, be regarded as a series of tests, including both questions in a medical history and components of a physical examination, where the post-test probability of a previous test can be used as the pre-test probability of the next. The indications for choosing the next test is dynamically influenced by the results of previous tests.
Let's say that the patient in this example is revealed to have depression, bone pain, joint pain and constipation of more severerity than what would be expected by the hypercalcemia itself, supporting the suspicion of primary hyperparathyroidism,[4] and let's say that the likelihood ratios for the tests, when multiplied together, roughly results in a product of 10 for primary hyperparathyroidism.
All the tests of the history and examination can concomitantly be used to estimate likelihood ratios for the presence of cancer, and let's say that the product of the likelihood ratios is estimated to be 3.
Tests for other conditions were basically all negative, and let's say that the resultant probability after the history and examination becomes 0.0005.
Continuing from the calcium- and parathyroid hormone related test, its post-test independently calculated odds are used as pre-test independently calculated odds for the medical history and physical examination (here abbreviated as H&E), with the ensuing calculations following the same overall pattern as the previous calcium- and parathyroid hormone related test:
| PH | Cancer | Other conditions | No disease | |
| PreH&E ICO | 0.00875 | 0.0002 | 0.0005 | 0.0014 |
| Likelihood ratio by H&E | 10 | 3 | - | - |
| PostH&E ICO | 0.0875 | 0.0006 | 0.0005 | 0.0014 |
| PostH&E ICOall | 0.09 | |||
| PostH&E PRP | 97.2% | 0.7% | 0.6% | 1.6% |
These profile relative probabilities after the history and examination may make the physician confident enough to plan the patient for surgery for a parathyroidectomy to resect the affected tissue.
At this point, the profile-relative probability of "other conditions" is so low that the physician cannot think of any test for them that could make a difference that would be substantial enough to form an indication for such a test, and the physician thereby regards "other conditions" as ruled out, in this case not primarily by specific test for such other conditions that were negative, but rather by the absence of positive tests so far.
For "cancer", the cutoff at which to confidently regard it as ruled out may be more stringent because of severe consequences of missing it, so the physician may consider that at least a histopathologic examination of the resected tissue is indicated.
This case is continued in the example of Combinations in corresponding section below.
Finding candidate conditions
The validity of both methods described above are dependent of inclusion of candidate conditions that are responsible for as large part as possible of the probability of having developed the condition, and it's clinically important to include those where relatively fast initiation of therapy is most likely to result in greatest benefit. The need to find more candidate conditions for inclusion increases with increasing severity of the presentation itself. For example, if the only presentation is a deviating laboratory parameter and all common harmful underlying conditions have been ruled out, then it may be acceptable to stop finding more candidate conditions, but this would much more likely be unacceptable if the presentation would have been severe pain.
Combinations
If two conditions appear as certain by their independently calculated probabilities, then there is a strong indication that the condition is a combination of the two, which can be added to the list of candidate conditions and be calculated independently for further evaluation.
To continue the example used in independently and profile-relative probabilities, let's say that the ensuing surgery and histopathologic examination of the resected tissue confirms primary hyperparathyroidism, having a very high specificity, and let's say that it gives a likelihood ratio of 1000 in this case. However, let's also say that the histopathologic examination also showed a malignant pattern, and let's say that this pattern gives a likelihood ratio for cancer of 1000 as well. The resultant independently calculated odds in favor of primary hyperparathyroidism and cancer become 87.5 and 0.6, respectively, with profile-relative probabilities of 99.3% and 0.7%, respectively. However, at this point, the individually calculated odds in favor of cancer of 0.6, corresponding to an individually calculated probability of 37.5%, are high enough to consider that the patient actually has a combination of primary hyperparathyroidism and cancer, that is, in this case, parathyroid carcinoma. To evaluate its possibility by this method, the combination can be added to the list of candidate conditions, followed by processing by every relevant test performed so far. By an initial method by epidemiology, the incidence of parathyroid carcinoma is estimated at about 1 in 6 million people per year,[5] giving a very low probability before taking any tests into consideration. Still, the probability that a non-malignant primary hyperparathyroidism would have occurred at the same time as an unrelated non-carcinoma cancer that presents with malignant cells in the parathyroid gland is calculated by multiplying the probabilities of the two, resulting in a negligible probability in comparison. So, focusing on parathyroid carcinoma, let's say that a review in regard to the subsequent blood tests, medical history, physical examination, surgery observations and histopathological examination result in rather high likelihood ratios, in turn resulting in a profile-relative probability high enough for an indication for making a confirmatory test for parathyroid cancer. In reality, the histopathologist may have recognized parathyroid carcinoma by pattern-recognition directly and, with or without specific tissue processing, may have given a certain diagnostic opinion of parathyroid carcinoma.
Let's finally say that the diagnosis of parathyroid carcinoma resulted in an extended surgery that removed remaining malignant tissue before it had metastasized, and the patient lived happily ever after.
Machine differential diagnosis
Machine differential diagnosis is the use of computer software to partly or fully make a differential diagnosis. It may be regarded as an application of artificial intelligence.
Many studies demonstrate improvement of quality of care and reduction of medical errors by using such decision support systems. Some of these systems are designed for a specific medical problem such as schizophrenia,[6] Lyme disease[7] or ventilator-associated pneumonia.[8] Others such as Iliad, QMR, DiagnosisPro,[9] and VisualDx [10] are designed to cover all major clinical and diagnostic findings to assist physicians with faster and more accurate diagnosis.
However, these tools all still require advanced medical skills in order to rate the symptoms and choose additional tests to deduce the probabilities of different diagnoses. Thus, non-professionals still need to see a health care provider in order to get a proper diagnosis.
History
The method of differential diagnosis was first suggested for use in the diagnosis of mental disorders by Emil Kraepelin. It is more systematic than the old-fashioned method of diagnosis by gestalt (impression).
Alternative medical meanings
Differential diagnosis is also used more loosely, to refer simply to a list of the most common causes of a given symptom, to a list of disorders similar to a given disorder, or to such lists when they are annotated with advice on how to narrow the list down (the book French's Index of Differential Diagnosis, ISBN 0340810475, is an example). Thus, a differential diagnosis in this sense is medical information specially organized to aid in diagnosis.
Usage apart from in medicine
Methods similar to those of differential diagnostic processes in medicine are also is used by biological taxonomists to identify and classify organisms, living and extinct. For example, after finding an unknown species, there can first be a listing of all potential species, followed by ruling out of one by one until, optimally, only one potential choice remains.
See also
References
- ^ VINDICATE – Mnemonic for differential diagnosis at PG Blazer.com.
- ^ Seccareccia, D. (Mar 2010). "Cancer-related hypercalcemia.". Can Fam Physician 56 (3): 244–6, e90-2. PMID 20228307. [1] [2]
- ^ [3] Lepage, R.; d'Amour, P.; Boucher, A.; Hamel, L.; Demontigny, C.; Labelle, F. (1988). "Clinical performance of a parathyrin immunoassay with dynamically determined reference values". Clinical chemistry 34 (12): 2439–2443. PMID 3058363.
- ^ Bargren, A. E.; Repplinger, D.; Chen, H.; Sippel, R. S. (2011). "Can Biochemical Abnormalities Predict Symptomatology in Patients with Primary Hyperparathyroidism?". Journal of the American College of Surgeons 213 (3): 410–414. doi:10.1016/j.jamcollsurg.2011.06.401. PMID 21723154.
- ^ Parathyroid Cancer Treatment at National Cancer Institute. Last Modified: 03/11/2009
- ^ Razzouk, D.; Mari, J. J.; Shirakawa, I.; Wainer, J.; Sigulem, D. (January 2006). "Decision support system for the diagnosis of schizophrenia disorders". Brazilian Journal of Medical and Biological Research 39 (1): 119–28. doi:/S0100-879X2006000100014. PMID 16400472.
- ^ Hejlesen OK, Olesen KG, Dessau R, Beltoft I, Trangeled M (2005). "Decision support for diagnosis of lyme disease". Studies in Health Technology and Informatics 116: 205–10. PMID 16160260. http://booksonline.iospress.nl/Extern/EnterMedLine.aspx?ISSN=0926-9630&Volume=116&SPage=205.
- ^ "Evaluation of a Computer Assisted Decision Support System (DSS) for Diagnosis and Treatment of Ventilator Associated Pneumonia (VAP) in Intensive Care Unit (ICU).". nih.gov. http://gateway.nlm.nih.gov/MeetingAbstracts/ma?f=102248792.html. Retrieved 2008-10-03.
- ^ "DiagnosisPro differential diagnosis reminder tool". diagnosispro.com. http://en.diagnosispro.com/. Retrieved 2008-10-03.
- ^ http://www.visualdx.com
Further reading
- The Merck Manual of Diagnosis and Therapy has 11 index entries describing the topic as differential diagnosis.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||