Spinal cord injury
| Spinal cord injuries | |
|---|---|
| Classification and external resources | |
| ICD-10 | G95.9, T09.3 |
| DiseasesDB | 12327 29466 |
| eMedicine | emerg/553 neuro/711 pmr/182 pmr/183 orthoped/425 |
| MeSH | D013119 |
Spinal cord injuries cause myelopathy or damage to nerve roots or myelinated fiber tracts that carry signals to and from the brain.[1][2] Depending on its classification and severity, this type of traumatic injury could also damage the grey matter in the central part of the cord, causing segmental losses of interneurons and motorneurons. Spinal cord injury can occur from many causes, including:
- Trauma such as automobile crashes, falls, gunshots, diving accidents, war injuries, etc.
- Tumor such as meningiomas, ependymomas, astrocytomas, and metastatic cancer.
- Ischemia resulting from occlusion of spinal blood vessels, including dissecting aortic aneurysms, emboli, arteriosclerosis.
- Developmental disorders, such as spina bifida, meningomyolcoele, and others
- Neurodegenerative diseases, such as Friedreich's ataxia, spinocerebellar ataxia, etc.
- Demyelinative diseases, such as Multiple Sclerosis.
- Transverse myelitis, resulting from stroke, inflammation, or other causes.
- Vascular malformations, such as arteriovenous malformation (AVM), dural arteriovenous fistula (AVF), spinal hemangioma, cavernous angioma and aneurysm.
Contents |
Classification
The American Spinal Injury Association (ASIA) defined an international classification based on neurological responses, touch and pinprick sensations tested in each dermatome, and strength of ten key muscles on each side of the body, e.g. shoulder shrug (C4), elbow flexion (C5), wrist extension (C6), elbow extension (C7), hip flexion (L2). Traumatic spinal cord injury is classified into five categories by the American Spinal Injury Association and the International Spinal Cord Injury Classification System:
- A indicates a "complete" spinal cord injury where no motor or sensory function is preserved in the sacral segments S4-S5.
- B indicates an "incomplete" spinal cord injury where sensory but not motor function is preserved below the neurological level and includes the sacral segments S4-S5. This is typically a transient phase and if the person recovers any motor function below the neurological level, that person essentially becomes a motor incomplete, i.e. ASIA C or D.
- C indicates an "incomplete" spinal cord injury where motor function is preserved below the neurological level and more than half of key muscles below the neurological level have a muscle grade of less than 3, which indicates active movement with full range of motion against gravity.
- D indicates an "incomplete" spinal cord injury where motor function is preserved below the neurological level and at least half of the key muscles below the neurological level have a muscle grade of 3 or more.
- E indicates "normal" where motor and sensory scores are normal. Note that it is possible to have spinal cord injury and neurological deficits with completely normal motor and sensory scores.
In addition, there are several clinical syndromes associated with incomplete spinal cord injuries.
- The Central cord syndrome is associated with greater loss of upper limb function compared to lower limbs.
- The Brown-Séquard syndrome results from injury to one side with the spinal cord, causing weakness and loss of proprioception on the side of the injury and loss of pain and thermal sensation of the other side.
- The Anterior cord syndrome results from injury to the anterior part of the spinal cord, causing weakness and loss of pain and thermal sensations below the injury site but preservation of proprioception that is usually carried in the posterior part of the spinal cord.
- Tabes Dorsalis results from injury to the posterior part of the spinal cord, usually from infection diseases such as syphilis, causing loss of touch and proprioceptive sensation.
- Conus medullaris syndrome results from injury to the tip of the spinal cord, located at L1 vertebra.
- Cauda equina syndrome is, strictly speaking, not really spinal cord injury but injury to the spinal roots below the L1 vertebra.
Facts and Figures
One can have spine injury without spinal cord injury. Many people suffer transient loss of function ("stingers") in sports accidents or pain in "whiplash" of the neck without neurological loss and relatively few of these suffer spinal cord injury sufficient to warrant hospitalization. In the United States, the incidence of spinal cord injury has been estimated to be about 40 cases (per 1 million people) per year or 12,000 cases per year .[3] In China, the incidence of spinal cord injury is approximately 60,000 per year.[4]
The prevalence of spinal cord injury is not well known in many large countries. In some countries, such as Sweden and Iceland, registries are available. According to new data collected by the Christopher and Dana Reeve Foundation, in the US, there are currently 1.3 million individuals living with spinal cord injuries- a number five times that previously estimated in 2007. 61% of spinal cord injuries occur in males, and 39% in females. The average age for spinal cord injuries is 48 years old. There are many causes leading to spinal cord injuries. These include motor vehicle accidents (24%), work-related accidents (28%), sporting/recreation accidents (16%), and falls (9%).
Effects
 |
|
| Segmental Spinal Cord Level and Function | |
|---|---|
| Level | Function |
| C1-C6 | Neck flexors |
| C1-T1 | Neck extensors |
| C3, C4, C5 | Supply diaphragm (mostly C4) |
| C5, C6 | Shoulder movement, raise arm (deltoid); flexion of elbow (biceps); C6 externally rotates the arm (supinates) |
| C6, C7 | Extends elbow and wrist (triceps and wrist extensors); pronates wrist |
| C7, T1 | Flexes wrist |
| C7, T1 | Supply small muscles of the hand |
| T1 -T6 | Intercostals and trunk above the waist |
| T7-L1 | Abdominal muscles |
| L1, L2, L3, L4 | Thigh flexion |
| L2, L3, L4 | Thigh adduction |
| L4, L5, S1 | Thigh abduction |
| L5, S1, S2 | Extension of leg at the hip (gluteus maximus) |
| L2, L3, L4 | Extension of leg at the knee (quadriceps femoris) |
| L4, L5, S1, S2 | Flexion of leg at the knee (hamstrings) |
| L4, L5, S1 | Dorsiflexion of foot (tibialis anterior) |
| L4, L5, S1 | Extension of toes |
| L5, S1, S2 | Plantar flexion of foot |
| L5, S1, S2 | Flexion of toes |
The effects of a spinal cord injury may vary depending on the type, level, and severity of injury, but can be classified into two general categories:
- In a complete injury, function below the "neurological" level is lost. Absence of motor and sensory function below a specific spinal level is considered a "complete injury". Recent evidence suggests that less than 5% of people with "complete" spinal cord injuries recover locomotion.
- In an incomplete injury, some sensation and/or movement below the level of the injury is retained. The lowest spinal segment in humans is located at vertebral levels S4-5, corresponding to the anal sphincter and peri-anal sensation. The ability to contract the anal sphincter voluntarily or to feel peri-anal pinprick or touch, the injury is considered to be "incomplete". Recent evidence suggests that over 95% of people with "incomplete" spinal cord injuries recover some locomotor function.
In addition to loss of sensation and motor function below the level of injury, individuals with spinal cord injuries will also often experience other complications:
- Bowel and bladder function is regulated by the sacral region of the spine. In that regard, it is very common to experience dysfunction of the bowel and bladder, including infections of the bladder and anal incontinence, after traumatic injury.
- Sexual function is also associated with the sacral spinal segments, and is often affected after injury. During a psychogenic sexual experience, signals from the brain are sent to spinal levels T10-L2 and in case of men, are then relayed to the penis where they trigger an erection. A reflex erection, on the other hand, occurs as a result of direct physical contact to the penis or other erotic areas such as the ears, nipples or neck. A reflex erection is involuntary and can occur without sexually stimulating thoughts. The nerves that control a man’s ability to have a reflex erection are located in the sacral nerves (S2-S4) of the spinal cord and could be affected after a spinal cord injury.[5]
- Injuries at the C-1/C-2 levels will often result in loss of breathing, necessitating mechanical ventilators or phrenic nerve pacing.
- Inability or reduced ability to regulate heart rate, blood pressure, sweating and hence body temperature.
- Spasticity (increased reflexes and stiffness of the limbs).
- Neuropathic pain.
- Autonomic dysreflexia or abnormal increases in blood pressure, sweating, and other autonomic responses to pain or sensory disturbances.
- Atrophy of muscle.
- Superior Mesenteric Artery Syndrome.
- Osteoporosis (loss of calcium) and bone degeneration.
- Gallbladder and renal stones.
The Location of the Injury
Determining the exact level of injury is critical in making accurate predictions about the specific parts of the body that may be affected by paralysis and loss of function.
The symptoms observed after a spinal cord injury differ by location (refer to the spinal cord map on the right to determine location). Notably, while the prognosis of complete injuries are generally predictable, the symptoms of incomplete injuries span a variable range. Accordingly, it is difficult to make an accurate prognosis for these types of injuries.
Cervical injuries
Cervical (neck) injuries usually result in full or partial tetraplegia (Quadriplegia). However, depending on the specific location and severity of trauma, limited function may be retained.
- C3 vertebrae and above : Typically results in loss of diaphragm function, necessitating the use of a ventilator for breathing.
- C4 : Results in significant loss of function at the biceps and shoulders.
- C5 : Results in potential loss of function at the shoulders and biceps, and complete loss of function at the wrists and hands.
- C6 : Results in limited wrist control, and complete loss of hand function.
- C7 and T1 : Results in lack of dexterity in the hands and fingers, but allows for limited use of arms. C7 is generally the threshold level for retaining functional independence.
Thoracic injuries
Injuries at or below the thoracic spinal levels result in paraplegia. Function of the hands, arms, neck, and breathing is usually not affected.
- T1 to T8 : Results in the inability to control the abdominal muscles. Accordingly, trunk stability is affected. The lower the level of injury, the less severe the effects.
- T9 to T12 : Results in partial loss of trunk and abdominal muscle control.
Lumbar and Sacral injuries
The effects of injuries to the lumbar or sacral regions of the spinal cord are decreased control of the legs and hips, urinary system, and anus.
Central Cord and Other Syndromes
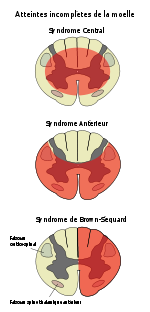
Central cord syndrome (picture 1) is a form of incomplete spinal cord injury characterized by impairment in the arms and hands and, to a lesser extent, in the legs. This is also referred to as inverse paraplegia, because the hands and arms are paralyzed while the legs and lower extremities work correctly.
Most often the damage is to the cervical or upper thoracic regions of the spinal cord, and characterized by weakness in the arms with relative sparing of the legs with variable sensory loss.
This condition is associated with ischemia, hemorrhage, or necrosis involving the central portions of the spinal cord (the large nerve fibers that carry information directly from the cerebral cortex). Corticospinal fibers destined for the legs are spared due to their more external location in the spinal cord.
This clinical pattern may emerge during recovery from spinal shock due to prolonged swelling around or near the vertebrae, causing pressures on the cord. The symptoms may be transient or permanent.
Anterior cord syndrome (picture 2) is also an incomplete spinal cord injury. Below the injury, motor function, pain sensation, and temperature sensation is lost; touch, proprioception (sense of position in space), and vibration sense remain intact. Posterior cord syndrome (not pictured) can also occur, but is very rare.
Brown-Séquard syndrome (picture 3) usually occurs when the spinal cord is hemisectioned or injured on the lateral side. On the ipsilateral side of the injury (same side), there is a loss of motor function, proprioception, vibration, and light touch. Contralaterally (opposite side of injury), there is a loss of pain, temperature, and deep touch sensations
Treatment
Treatment options for acute, traumatic non-penetrating spinal cord injuries include the administration of a high dose of an anti-inflammatory agent, methylprednisolone, within 8 hours of injury. This recommendation is primarily based on the National Acute Spinal Cord Injury Studies (NASCIS) I and II. However, in a third study, methylprednisolone failed to demonstrate an effect in comparison to placebo. Additionally, due to increased risk of infections, the use of this anti-inflammatory drug after spinal cord injuries is no longer recommended [6][7]. Presently, administration of cold saline acutely after injury is gaining popularity, but there is a paucity of empirical evidence for the beneficial effects of therapeutic hypothermia.
Scientists are investigating many promising avenues for treatment of spinal cord injury. Numerous articles in the medical literature describe research, mostly in animal models, aimed at reducing the paralyzing effects of injury and promoting regrowth of functional nerve fibers. Despite the devastating effects of the condition, commercial funding for research investigating a cure after spinal cord injury is limited, partially due to the small size of the population of potential beneficiaries. Despite this limitation, a number of experimental treatments have reached controlled human trials . In addition, therapeutic strategies involving neuronal protection and regeneration are also being investigated in other neurodegenerative diseases such as Alzheimer's Disease, Parkinson's Disease, Amyotrophic Lateral Sclerosis and Multiple sclerosis. There are many similarities between these conditions of the CNS and spinal cord injuries, thus increasing the potential for discovery of a treatment after spinal cord injuries.
Advances in identification of an effective therapeutic target after spinal cord injury have been newsworthy, and considerable media attention is often drawn towards new developments in this area. However, aside from methylprednisolone, none of these developments have reached even limited use in the clinical care of human spinal cord injury in the U.S. . Around the world, proprietary centers offering stem cell transplants and treatment with neuroregenerative substances are fueled by glowing testimonial reports of neurological improvement. It is also evident that when stem cells when injected in the area of damage in the spinal cord, they secrete neurotrophic factors and these neurotrophic factors help neurons and vessels grow to thus helping repair the damage [8] [9] [10]. Independent validation of the results of these treatments is lacking.[11]
Spinal Cord Injury Implications and Occupational Therapy
The signs and symptoms of spinal cord injury (SCI) significantly impact everyday activities. Occupational therapy plays an important role in the rehabilitation and management of SCI at all levels. An important therapeutic goal is to assist the client to restore function, enabling clients' to participate in the activities and tasks that are important to them. The ability to participate in meaningful, everyday activities is essential to an individual’s health and well-being.
Occupational therapists (OTs) focus on three life areas, which include self-care, productivity, and leisure. [12] Self-care tasks include basic needs such as bathing, hygiene, feeding, and dressing. Productivity includes activities such as paid work, volunteering, caregiving, or parenting. Leisure includes fun and enjoyable activities activities typically done during spare time. Performing daily activities can be difficult for an individual with a spinal cord injury. However, through the rehabilitation process individuals with SCI can live independently in the community with or without full-time attendant care, depending on the level of their injury. [13]
Occupational therapist's work collaboratively with their clients to identify challenges in the performance of daily tasks and activities related to self-care, productivity and leisure. [14] Informal and formal assessments help OTs gain information that helps them to understand their clients' challenges.
How Occupational Therapy Can Help Address Occupational Performance Issues
When an individual receives occupational therapy, they are referred to as a client. The role of occupational therapy in SCI rehabilitation is to assist clients in regaining abilities and roles that are important and meaningful. [15] After identifying areas that the client feels challenged with, the OT and client work together to prioritize and set goals. Together, they create plans that address the performance issues in order to encourage participation in everyday activities. An important feature of occupational therapy is the use of ‘therapeutic activities’ to achieve this goal. Finally, reassessment is done to measure the outcome of the effectiveness of the therapy plans.
Pallastrini et al [15]emphasize the importance of early occupational therapy, started immediately after the client is stable. During these early stages, OTs evaluate what the client is able to do and what the client is having difficulty with. Occupational therapists then work one-on-one with the client on skills required for daily living. The client is shown new ways of doing things and may be given assistive devices or equipment. Occupational therapists also help their clients develop coping skills, and implement exercises and routines that strengthen muscles. [15]
Occupational therapists use the information gained from formal and informal assessments to guide their intervention plans. When considering the role of OT in SCI, it is helpful to think about what interventions are commonplace during different phases of recovery, namely acute, acute rehabilitation and community phases. During the rehabilitation process, assessments are re-administered to evaluate progress and the effectiveness of therapy interventions. When considering assessments and interventions, consideration must also be given to age, gender, and a multitude of client-specific factors.
Phase 1: Acute Recovery
During acute recovery, the focus is on support and prevention. The OT helps the client gain a sense of control over a situation in which the client likely feels little independence. [13] The OT may make splints to prevent deformities in the hands. Additionally, daily arm and hand exercises are performed to maintain normal function. Fitting and selecting the most appropriate temporary wheelchair to enable mobility is important in this stage. Finally, teaching the client and care providers appropriate positioning in bed and in the wheelchair is critical for the prevention of pressure sores. [13] Education regarding pressure sore prevention continues into the rehabilitation phase. See self-care skills.
Phase 2: Acute Rehabilitation
During acute rehabilitation, OT interventions focus on support, education for the client and family/caregivers, meaningful activities, choosing equipment and restoring the client’s self esteem and confidence. [13] It is particularly important to consider the client’s discharge environment (i.e. home, community and social setting) in order to prepare for community living. With the client, the OT creates an individual program to meet the client's needs. The following are key areas of intervention common to numerous rehabilitation settings [16] :
Assessment and treatment of the upper limbs.
Early in the rehabilitation phase, the OT evaluates the client’s strength and sensation in the upper extremity (UE); lower extremity (LE) evaluation falls under the responsibility of the physical therapist. The OT makes use of therapeutic activities to both strengthen muscles and improve hand function. Custom-made splints are commonly used to help position the hands in a functional position and assist in preventing deformity. [16] Individuals who retain wrist function are taught to use tenodesis grasp (extending the wrist to bring the thumb and index finger together and flexing the wrist to separate the thumb and index finger) for picking up and releasing light objects. [13] Using meaningful activities to build strength, endurance, and coordination helps to differentiate the work of occupational therapists from physical therapists.
Self care retraining.
Obtaining competency in self-care tasks contributes significantly to an individual's sense of self confidence and independence. The focus is on feeding, grooming, bathing, dressing and bowel/bladder management. [13] Assistive devices and specialized equipment are prescribed by the OT to help the client achieve greater competency and independence in their activities of daily living. Depending on the level and severity of the injury, independence in feeding, grooming, UE dressing and bathing may be achieved with the assistance of adaptive equipment for dressing and bathing the LE. [17] Examples of commonly prescribed equipment include: dressing and bathing aids for the LE, a padded transfer tub bench, shower-commode chair, or hand-held shower. Adaptive devices may also be required to assist with bowel and bladder management. A key role for the OT is to educate both the client and the client's caregiver(s) in the proper care and use of the adaptive aids/equipment. Practice sessions under the supervision and guidance of the OT are provided until the client feels competent using the adaptive aids and techniques.
Pressure sores are secondary complications of SCI. Educating clients about the risks that lead to pressure sores and strategies for prevention is important to health and well-being.[16] For example, an important part of the prevention strategy includes teaching clients about the importance of maintaining a good position in bed and in any seating aids (e.g. wheelchair). In addition, the OT teaches the client about the importance of shifting their weight regularly in both lying and seated positions. Clients who lack strength in their upper extremity can achieve a weight shift by tilting their chair in space. Tilting the wheelchair takes pressure off the buttocks area, which is one area at high-risk for pressure sore development. In addition to education, the therapist assesses the client for the best pressure relieving surfaces (i.e. cushion and mattress) to aid in pressure sore prevention.
Transfer skills.
Transfers are a key area of education and skill development. [16] Examples of different transfers include: moving from bed to wheelchair, from wheelchair to toilet or tub, and from wheelchair to driver’s seat. Strength in the upper extremities makes it possible to transfer independently from one surface to another either with the aid of a sliding transfer board or by utilizing grab bars. Frequent practice under the guidance of the OT assists clients with the necessary skill development.
Bed mobility.
Occupational therapists teach their clients bed mobility skills required for many daily tasks, such as getting dressed, moving out of bed, and correct positioning in bed for skin protection and comfort. [16]
Mobility skills.
Not being able to move around without help is the largest restriction to participating in activities of daily living. The wheelchair that a person uses can significantly affect their quality of participation. A key area for the OT is to assist clients with the selection of the most suitable mobility aid in accordance with their needs, finances, abilities, preferences and available technology. [18] A proper fitting wheelchair is critical for good posture and comfort. Creating an ideal match between the client's needs and the equipment available is challenging. The client's level of funding and the high cost of equipment adds further complexity. [18]
The level and severity of a clients SCI determines the most suitable mobility aid. For example, some clients require a power wheelchair both indoors and outdoors while others can manage on both terrains using a manual wheelchair. If a client requires assistance with uneven outdoor surfaces, the OT may prescribe both a power and manual wheelchair to allow for flexibility according to their needs. This involves fitting clients for both wheelchairs and selecting the best pressure relieving surfaces/cushions and backrests. In addition, power and manual wheelchair training assists clients in developing skills both indoors and outdoors.
Home assessment and modifications.
Discussing the client's housing situation is an important part of rehabilitation planning. Where possible, the OT will make a home visit to assess the need for changes and adaptations to the home. Examples of common adaptations include: adding ramps or lifts to get into the home, widening doorways, adapting the bathroom and kitchen for wheelchair accessibility, placing electrical switches at wheelchair level, and choosing wheelchair-friendly flooring. Involving the client and family in determining solutions and making decisions is very important. Assessing the need for specialized equipment (i.e. hospital bed or pressure relieving mattress) also takes place during rehabilitation. The client will be encouraged to try different pieces of equipment in relation to self-care, communication, and other activities of daily living. With guidance from the OT, the client will decide on the most appropriate items of equipment to suit their needs.
Domestic retraining.
During rehabilitation, opportunities are provided for clients to practice a variety of domestic skills. For example, clients can practice cooking in a wheelchair-accessible kitchen. They can trial different pieces of equipment that can enhance independence in this area. A variety of adaptive aids for the kitchen address limitations in grip strength. [15] Occupational therapists teach adaptive strategies for carrying out domestic chores (i.e. childcare, cleaning, laundry) that are adjusted to suit the client's needs and abilities. It may be necessary to hire a community home care support worker to assist with domestic chores. The amount of additional outside support depends on the level and severity of the client's SCI and can vary from 24 hours per day to just a few hours per day. [13]
Assistance with return to driving/transportation.
Clients who are able to transfer independently from their wheelchair to the driver’s seat using a sliding transfer board, are candidates for returning to driving. Complete independence with driving also requires the ability to load and unload one’s wheelchair from the vehicle. [13] Clients capable of driving are referred by the OT to the 'Return to driving program' within the Driver Assessment and Rehabilitation Unit at the hospital. The goal of the program is to provide education and retraining to help clients return to driving. Assistance with selecting an appropriate modified vehicle that will meet the client’s needs and budget are part of the program. For clients who do not wish to return to driving, alternate transportation options are also addressed (i.e. accessible parking, taxi subsidy vouchers, modified vehicle for passenger transit and public transportation).
Community living skills.
Clients may be involved in a support group, which addresses skills that prepare clients for returning home and to the community. As previously mentioned, driving and wheelchair mobility skills are important for accessing the community. Community outings are commonly organized to help transition the client into the community. [16] (See community reintegration for more details.)
Leisure and recreation skills.
Part of rehabilitation involves investigating options for returning to previous leisure/recreation interests as well as developing new pursuits. In addition, the OT can assist the client in finding ways to cope with physical and social issues that may get in the way of leisure participation. [17]
Work/study skills.
Addressing the client's career and educational goals is very important. If appropriate, a work site/school visit may be arranged to assess for accessibility. Otherwise, a referral to a community based work/school assessment service may be indicated. [17]
Sexual Health.
Exploring concerns related to sexual health and function should form an integral part of each client's treatment plan. The OT can assist their client by providing information and identifying alternate resources and adaptive devices as needed. [17]
Phase 3: Community reintegration
Following rehabilitation, the client begins the process of community reintegration. Community participation is an important aspect in maintaining quality of life. [19] During community reintegration, the focus of occupational therapy is on restoring client roles at home and in the community, and promoting social participation and life satisfaction. [19] Ongoing education of the client, family and caregivers continues throughout this stage. Referrals can be made to an outpatient clinic or community therapist to continue with treatment and progress made during rehabilitation. Outpatient programs teach clients how to use new movement and they offer training for activities of daily living as clients continue to gain strength during the first year after injury. In addition, the OT and client work on goals and skills that encourage the client towards community integration (i.e. driving, vocational evaluation and training, participation in leisure interests). Additionally, the therapist identifies transitional services such as support groups and transitional living centres if required.
Occupational therapists are also involved with advocacy on behalf of their clients. Advocacy can take many forms and apply in areas that impact the client's ability to fully participate within their community. This includes helping to address barriers to employment, and leisure at a policy level. Examples of large barriers involving physical structures are playground designs, city planning, and accessible buildings. An OT can address decision makers, argue in favour of their client's needs and bring important information and perspectives to others who may be causing a barrier for the client. Occupational therapists can promote awareness, and lobby on behalf of their clients. Finally, OTs address issues such as social stigma by advocating on their client's behalf. Stigma can be addressed: (a) by challenging others to think differently, (b) by making others aware of marginalization, and (c) by helping others understand the loss of privileges that can occur at both the societal and policy level. [20]
See also
- Brown-Sequard Syndrome
- Syringomyelia
- Paraplegia
- Quadriplegia/Tetraplegia
External links
- Miami Project to Cure Paralysis Noted for experimental cooling protocol used on Kevin Everett
- United Spinal Association A membership organization dedicated to improving the quality of life of individuals with spinal cord injuries and related disorders.
- Syringomyelia Foundation A Non-Profit Charity whose goal is to improve the quality of life of those who suffer from Syringomyelia (also known as Morvan's Disease) and other spinal cord injuries and conditions by providing various types of assistance as needed on a case-by-case basis through case management
- Rehabilitation Research and Training Center (RRTC) on Spinal Cord Injury: Promoting Health and Preventing Complications through Exercise
- SCI Images - Images of Spinal Cord Injury
- sci.rutgers.edu - Spinal Cord Injury Levels and Classification
- The Spinal Cord Injury Project, W.M. Keck Center for Collaborative Neuroscience at Rutgers University
- EMSCI Network European Multicenter Study about Spinal Cord Injury
- Brigham and Women's Hospital Translational Pain Research Clinical trials for pain following SCI
- Pediatric and Adolescent Spinal Cord Injury
- Rehabilitation Engineering Research Center on Wheeled Mobility
- International Institute for Research in Paraplegia Research funding foundation, based in Zurich
- Spinal Cord Injuries Emergency Medicine for Spinal Cord Injuries
- Trefethen, Tre. User's Manual for the Paralyzed Penis: Love after spinal cord injury American Sexuality Magazine. Accessed 3-22-07.
- About Spinal Cord Injury Spinal Cord Injury FAQ for those with SCI, and their families, by Canadian Paraplegic Association - Ontario.
- ICF based Case studies in Spinal Cord Injury Rehabilitation
- CareCure Community Social and informational site for individuals with spinal cord injuries.
- Spinal Cord Injury Health Information Information and support for people affected with spinal cord injuries.
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
References
- ↑ Spinal Cord Medicine: Principles and Practice (2002) Lin VWH, Cardenas DD, Cutter NC, Frost FS, Hammond MC. Demos Medical Publishing
- ↑ Spinal Cord Medicine (2001) Kirshblum S, Campagnolo D, Delisa J. Lippincott Williams & Wilkins
- ↑ http://www.fscip.org/facts.htm
- ↑ Qiu J (July 2009). "China Spinal Cord Injury Network: changes from within". Lancet Neurol 8 (7): 606–7. doi:10.1016/S1474-4422(09)70162-0. PMID 19539234.
- ↑ Klebin, Phil Sexual Function of Men with Spinal Cord Injury May 2007
- ↑ "UpToDate Inc.". http://www.uptodate.com/online/content/topic.do?topicKey=medneuro/10703&selectedTitle=3~150&source=search_result.
- ↑ "BestBets: Steroids in acute spinal cord injury". http://www.bestbets.org/bets/bet.php?id=105.
- ↑ Abraham S (March 2008). "Autologous Stem Cell Injections for Spinal Cord Injury - A multicentric Study with 6 month follow up of 108 patients". 7th Annual Meeting of Japanese Society of Regenerative Medicine, Nagoya, Japan.
- ↑ R Ravikumar, S Narayanan and S Abraham (Nov 2007). "Autologous stem cells for spinal cord injury". Regenerative Medicine 2 (6): 53-61.
- ↑ Abraham S (June 2007). "Autologous Bone Marrow Mononuclear Cells for spinal cord injury- A case report". Cytotherapy 9 (1).
- ↑ Dobkin, BH.; Curt, A.; Guest, J. “Cellular transplants in China: observational study from the largest human experiment in chronic spinal cord injury.” Neurorehabilitation and Neural Repair, v. 20 issue 1, 2006, p. 5-13.
- ↑ Krupa T, Fossey E, Anthony WA, Brown C. Doing daily life: how occupational therapy can inform psychiatric rehabilitation practice. Psychiatr Rehabil J.2009; 32(3), 155-161.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 13.7 Radomski MV, Trombly Latham CA. Occupational therapy for physical dysfunction: 6th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2008.
- ↑ Canadian Association of Occupational Therapists. Enabling occupation: an occupational therapy perspective (Rev. ed.). Ottawa, (ON): CAOT Publications ACE; 2002.
- ↑ 15.0 15.1 15.2 15.3 Pillastrini P, Mugnai R, Bonfiglioli R, Curti S, Mattioli S, Maioli MG, et al. Evaluation of an occupational therapy program for patients with spinal cord injury. Spinal Cord 2008;46:78-81.
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 Ozelie R, Sipple S, Foy T, Cantoni K, Kellogg K, Lookingbill J, et al. Classification of SCI rehabilitation treatments #8: SCI Rehab Project Series: The Occupational Therapy Taxonomy. J Spinal Cord Med 2009;32:283–297.
- ↑ 17.0 17.1 17.2 17.3 Atchison BJ, Dirette, D.K. Conditions in Occupational Therapy. Effect on Occupational Performance. 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2007.
- ↑ 18.0 18.1 Di Marco A, Russell M, Masters M. Standards for wheelchair prescription. Aust Occup Ther J 2003;50:30-39.
- ↑ 19.0 19.1 Cohen ME, Schemm RL. Client-centered occupational therapy for individuals with Spinal Cord Injury. Occup Ther in Health Care 2007;21(3):1-15.
- ↑ Townsend EA, Polatajko H. Enabling occupation II: Advancing an occupational therapy vision for health, well-being, & justice through occupation. Ottawa, Ontario: CAOT Publications; 2007.