Zanamivir
 |
|
|---|---|
| Systematic (IUPAC) name | |
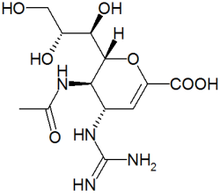
| (2R,3R,4S)- 4-[(diaminomethylidene)amino]- 3-acetamido- 2-[(1R,2R)- 1,2,3-trihydroxypropyl]- 3,4-dihydro- 2H-pyran- 6-carboxylic acid | |
| Identifiers | |
| CAS number | 139110-80-8 |
| ATC code | J05AH01 |
| PubChem | CID 60855 |
| DrugBank | APRD00378 |
| Chemical data | |
| Formula | C12H20N4O7 |
| Mol. mass | 332.31 g/mol |
| Synonyms | 5-acetamido- 4-guanidino- 6-(1,2,3-trihydroxypropyl)- 5,6-dihydro- 4H-pyran- 2-carboxylic acid |
| Pharmacokinetic data | |
| Bioavailability | 2% (oral) |
| Protein binding | <10% |
| Metabolism | Negligible |
| Half-life | 2.5–5.1 hours |
| Excretion | Renal |
| Therapeutic considerations | |
| Pregnancy cat. | B1 (Au), C (US) |
| Legal status | S4 (Au), POM (UK), ℞-only (U.S.) |
| Routes | Inhalation |
| |
|
| Influenza (Flu) |
|---|
 |
| Types |
| Avian (A/H5N1 subtype) · Canine Equine · Swine (A/H1N1 subtype) |
| Vaccines |
| 2009 pandemic (Pandemrix) ACAM-FLU-A · Fluzone · Influvac Live attenuated (FluMist) · Optaflu |
| Treatment |
| Amantadine · Arbidol · Laninamivir Oseltamivir · Peramivir · Rimantadine Vitamin D · Zanamivir |
| Pandemics |
| 2009 · 1968–1969 Hong Kong · 1918 |
| Outbreaks |
| 2008 West Bengal 2007 Bernard Matthews H5N1 2007 Australian equine 2006 H5N1 India · 1976 swine flu |
| See also |
| Flu season · Influenza evolution Influenza research Influenza-like illness |
Zanamivir (INN) (pronounced /zəˈnæmɨvɪər/) is a neuraminidase inhibitor used in the treatment and prophylaxis of Influenzavirus A and Influenzavirus B. Zanamivir was the first neuraminidase inhibitor commercially developed. It is currently marketed by GlaxoSmithKline under the trade name Relenza.
According to the Centers for Disease Control and Prevention (CDC), no flu, seasonal or pandemic, has shown any signs of resistance to zanamivir.[1]
Contents |
History
Zanamivir was discovered in 1989 by scientists led by Mark von Itzstein, at the Victorian College of Pharmacy, Monash University, in collaboration with the CSIRO and scientists at Glaxo, UK. Zanamivir was the first of the neuraminidase inhibitors. The discovery was funded initially by the Australian biotechnology company Biota and was part of Biota's ongoing program to develop antiviral agents through rational drug design. Its strategy relied on the availability of the structure of influenza neuraminidase, by X-ray crystallography. It was also known, as far back as 1974, that 2-deoxy-2,3-didehydro-N-acetylneuraminic acid (DANA), a sialic acid analogue, was an inhibitor of neuraminidase.[2] Sialic acid (N-acetyl neuraminic acid, NANA), the substrate of neuraminidase, is itself a mild inhibitor of the enzyme, but the dehydrated derivative DANA, a transition-state analogue, is a better inhibitor.
Computational chemistry techniques were used to probe the active site of the enzyme, in an attempt to design derivatives of DANA that would bind tightly to the aminoacid residues of the catalytic site, and so would be potent and specific inhibitors of the enzyme. The software GRID from Molecular Discovery was used to determine energetically favourable interactions between various functional groups and residues in the catalytic site canyon. This showed there was a negatively charged zone in the neuraminidase active site that aligned with the C4 hydroxyl group of DANA. This hydroxyl was therefore replaced with a positively charged amino group; the 4-amino DANA was 100 times better an inhibitor than DANA, owing to the formation of a salt bridge with a conserved glutamic acid (119) in the active site. It was also noticed that Glu 119 was at the bottom of a conserved pocket in the active site just big enough to accommodate a more basic functional positively charged group, such as a guanidino group, which was also larger than the amino group.[3] Zanamivir, a transition-state analogue inhibitor of neuraminidase, was the result.[4]
Developments
Recently, the reported oseltamivir-resistance H5N1 virus neuraminidase still retaining susceptibility to zanamivir indicates that the structure of zanamivir has some advantages over oseltamivir in binding to the active pocket of H5N1 neuraminidase.[5][6][7]
As a proven anti-influenza drug target, neuraminidase continues to be attractive for the development of new inhibitors. The crystal structure of H5N1 avian influenza neuraminidase (PDB code: 2HTY) provides the three-dimensional structural information and opportunity for finding new inhibitors in this regard, because the existing inhibitors, such as oseltamivir and zanamivir, were developed based on different structures of neuraminidase, such as subtypes N9, N2, and type B genus of influenza virus.
Pharmocology
Zanamivir is specifically for the treatment of infections caused by Influenzavirus A and Influenzavirus B.
Influenza, commonly known as the flu, is caused by a virus which targets the body's respiratory cells and damages the lining of the respiratory tract, leading to swelling and inflammation of the tract. Influenza spreads rapidly by replicating itself inside the host cell, producing hundreds of copies of the virus in a short period. In approximately an hour the virus can destroy the host cell and propel its replications out into the body to find new host cells. For some people, the flu and its complications can be very serious, even fatal.
Zanamivir works by binding to the active site of the neuraminidase protein, rendering the influenza virus unable to escape its host cell and infect others.[8] It is also an inhibitor of influenza virus replication in vitro and in vivo. In clinical trials it was found that zanamivir was able to reduce the time to symptom resolution by 1.5 days if therapy was started within 48 hours of the onset of symptoms.
Dosing and side effects
The bioavailability of zanamivir is 2%. After inhalation, zanamivir is concentrated in the lungs and oropharynx, where up to 15% of the dose is absorbed and excreted in urine.[9]
Dosing is limited to the inhaled route. This restricts its usage, as treating asthmatics could induce bronchospasm.[10] The U.S. Food and Drug Administration (FDA) has issued a Public Health Advisory warning that it has received some reports of respiratory problems following inhalation of zanamivir by patients with underlying asthma or chronic obstructive pulmonary disease. The zanamivir package insert contains precautionary information regarding risk of bronchospasm in patients with respiratory disease.[11]
Zanamivir has not been known to cause toxic effects, does not spread around through the body's systemic circulation and shows no signs of viral resistance from any flu.
GlaxoSmithKline (GSK) and FDA notified healthcare professionals of a report of the death of a patient with influenza who received Relenza (zanamivir) Inhalation Powder which was solubilized and administered by mechanical ventilation.[12]
Commercial issues
Although zanamivir was the first neuraminidase inhibitor to the market, it had only a few months lead over the second entrant, oseltamivir (Tamiflu), with an oral tablet formulation.
According to the CDC, Tamiflu, zanamivir’s main competitor, is not as effective at treating the Influenza viruses as zanamivir, especially in H1N1 Seasonal Flu. In fact, tests showed that 99.6% of the tested strains of seasonal H1N1 flu and 0.5% of 2009 pandemic flu were resistant to Tamiflu while there have been absolutely zero flu samples seasonal or pandemic that show any resistance to zanamivir.[1] [5][6]
When first marketed in the USA in 1999/2000, zanamivir captured only 25% of the influenza antiviral market, despite a huge promotional campaign. By the end of that season, Tamiflu was outselling zanamivir 3:1. During that season, zanamivir experienced worldwide safety warnings involving the risk of bronchospasm and death. Glaxo then reduced the marketing of zanamivir, and Tamiflu's dominance increased. More than US$20m worth of zanamivir sold by Glaxo in the first US season was returned to the company in the next two seasons because zanamivir's actual sales to patients were far less than expected, highlighting the fact that the results of the first season were even worse than first thought.
Biota commenced legal proceedings in 2004 alleging that Glaxo's reduced marketing of zanamivir was a breach of contract. Biota claimed approximately A$700m from Glaxo. After Biota spent four years trying to progress its case, and incurring A$50m in legal costs, the company abandoned the claim in July 2008, recovering only A$20m including legal costs following settlement at mediation. Biota had refused an earlier tactical offer from Glaxo of A$75m plus legal costs.
In August 2006, Germany announced that it would buy 1.7 million doses of zanamivir, as part of its preparation strategy against bird flu. "Germany's purchase shows that countries are starting to take a balanced view of influenza preparedness," says Simon Tucker, head of research at Melbourne-based Biota, where zanamivir was originally developed.[8]
In April 2009 many cases of swine flu (H1N1 type virus) were reported in USA and Mexico. Zanamivir is one of only two drugs that are prescribed to treat it. A study published in June 2009 emphasized the urgent need for augmentation of oseltamivir (Tamiflu) stockpiles, with additional antiviral drugs including zanamivir, based on an evaluation of the performance of these drugs in the scenario that the 2009 H1N1 swine flu neuraminidase (NA) were to acquire the Tamiflu-resistance (His274Tyr) mutation which is currently widespread in 99.6% of all tested seasonal H1N1 strains.[13]
Biota, being only a small company, was not able to bring zanamivir to market by itself. In 1990, zanamivir patent rights were licensed to Glaxo, now GlaxoSmithKline (GSK). In 1999, the product was approved for marketing in the USA and subsequently has been registered by GSK in a total of 70 countries (GlaxoSmithKline News release, 2006). Zanamivir is delivered via Glaxo's proprietary Diskhaler inhalation device. The license agreement entitled Biota to receive a 7% royalty on Glaxo's sales of zanamivir.
Legal status
The drug is approved for use for the prevention and treatment of influenza in persons over the age of 7 in the United States, Canada, European Union and many other countries. It is not recommended for people with respiratory problems and ailments.
Chemistry

Scheigetz, J.; Zamboni, R.; Bernstein, M. A.;Roy, B.; Org. Prep. Proced. Int. 1995, 27, 637.
References
- ↑ 1.0 1.1 "2008-2009 Influenza Season Week 32 ending August 15, 2009". Flu Activity & Surveillance. Centers for Disease Control and Prevention (CDC). August 21, 2009. http://www.cdc.gov/flu/weekly/weeklyarchives2008-2009/weekly32.htm.
- ↑ Meindl P, Bodo G, Palese P, Schulman J, Tuppy H (April 1974). "Inhibition of neuraminidase activity by derivatives of 2-deoxy-2,3-dehydro-N-acetylneuraminic acid". Virology 58 (2): 457–63. doi:10.1016/0042-6822(74)90080-4. PMID 4362431.
- ↑ Laver, Graeme (March 2007). "Flu drugs - pathway to discovery". Education in Chemistry. http://www.rsc.org/Education/EiC/issues/2007March/FluDrugsPathwayDiscovery.asp. Retrieved 2009-11-11. ISSN 0013-1350
- ↑ von Itzstein M, Wu WY, Kok GB, et al. (June 1993). "Rational design of potent sialidase-based inhibitors of influenza virus replication". Nature 363 (6428): 418–23. doi:10.1038/363418a0. PMID 8502295.
- ↑ 5.0 5.1 Collins PJ, Haire LF, Lin YP, Liu J, Russell RJ, Walker PA, Skehel JJ, Martin SR, Hay AJ, Gamblin SJ. (2008). "Crystal structures of oseltamivir-resistant influenza virus neuraminidase mutants". Nature 453 (7199): 1258. doi:10.1038/nature06956. PMID 18480754.
- ↑ 6.0 6.1 Garcia-Sosa AT, Sild S, Maran U. (2008). "Design of Multi-Binding-Site Inhibitors, Ligand Efficiency, and Consensus Screening of Avian Influenza H5N1 Wild-Type Neuraminidase and of the Oseltamivir-Resistant H274Y Variant". J. Chem. Inf. Model. 48 (10): 2074–2080. doi:10.1021/ci800242z. PMID 18847186.
- ↑ Du QS, Wang SQ, Chou KC (October 2007). "Analogue inhibitors by modifying oseltamivir based on the crystal neuraminidase structure for treating drug-resistant H5N1 virus". Biochemical and Biophysical Research Communications 362 (2): 525–31. doi:10.1016/j.bbrc.2007.08.025. PMID 17707775.
- ↑ 8.0 8.1 Cyranoski D (September 2005). "Threat of pandemic brings flu drug back to life". Nature Medicine 11 (9): 909. doi:10.1038/nm0905-909. PMID 16145557.
- ↑ Moscona A (September 2005). "Neuraminidase inhibitors for influenza". The New England Journal of Medicine 353 (13): 1363–73. doi:10.1056/NEJMra050740. PMID 16192481.
- ↑ Hayden FG (December 2001). "Perspectives on antiviral use during pandemic influenza". Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences 356 (1416): 1877–84. doi:10.1098/rstb.2001.1007. PMID 11779387.
- ↑ "Safe and Appropriate Use of Influenza Drugs". Public Health Advisories (Drugs). U.S. Food and Drug Administration (FDA). April 30, 2009. http://www.fda.gov/Drugs/DrugSafety/PublicHealthAdvisories/ucm052240.htm. Retrieved 2009-11-11.
- ↑ www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm186081.htm
- ↑ Soundararajan V, Tharakaraman K, Raman R, Raguram S, Sasisekharan V, Sasisekharan R (June 2009). "Extrapolating from sequence--the 2009 H1N1 'swine' influenza virus". Nature Biotechnology 27 (6): 510–3. doi:10.1038/nbt0609-510. PMID 19513050.
External links
- The development of Relenza for treatment of influenza
- Drug Information: Zanamivir Inhalation MedlinePlus drug
- [www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm188870.htm Relenza: Consumer Questions and Answers] U.S. Food and Drug Administration (FDA)
- Relenza Biota Holdings
- Relenza web site GlaxoSmithKline
|
||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||