Radiology

Radiology is the branch or specialty of medicine that utilizes imaging technologies like x-rays, CT scans, and MRIs to diagnose and treat diseases.
Radiologists are physicians that utilize an array of imaging technologies (such as ultrasound, computed tomography (CT), nuclear medicine, positron emission tomography (PET) and magnetic resonance imaging (MRI)) to diagnose or treat diseases. Interventional radiology is the performance of (usually minimally invasive) medical procedures with the guidance of imaging technologies. The acquisition of medical imaging is usually carried out by the radiographer or radiologic technologist.
Contents |
Acquisition of radiological images
The following imaging modalities are used in the field of diagnostic radiology:
Projection (plain) radiography
Radiographs (or roentgenographs, named after the discoverer of x-rays, Wilhelm Conrad Röntgen) are produced by the transmission of x-rays through a patient to a capture device then converted into an image for diagnosis. The original and still common imaging produces silver impregnated films. In Film-Screen radiography an x-ray tube generates a beam of x-rays which is aimed at the patient. The x-rays which pass through the patient are filtered to reduce scatter and noise and then strike an undeveloped film, held tight to a screen of light emitting phosphors in a light-tight cassette. The film is then developed chemically and an image appears on the film. Now replacing Film-Screen radiography is Digital Radiography, DR, in which x-rays strike a plate of sensors which then converts the signals generated into digital information and an image on computer screen. Plain radiography was the only imaging modality available during the first 50 years of radiology. It is still the first study ordered in evaluation of the lungs, heart and skeleton because of its wide availability, speed and relative low cost.
Fluoroscopy
Fluoroscopy and angiography are special applications of X-ray imaging, in which a fluorescent screen and image intensifier tube is connected to a closed-circuit television system.[1]:26 This allows real-time imaging of structures in motion or augmented with a radiocontrast agent. Radiocontrast agents are administered, often swallowed or injected into the body of the patient, to delineate anatomy and functioning of the blood vessels, the genitourinary system or the gastrointestinal tract. Two radiocontrasts are presently in use. Barium (as BaSO4) may be given orally or rectally for evaluation of the GI tract. Iodine, in multiple proprietary forms, may be given by oral, rectal, intraarterial or intravenous routes. These radiocontrast agents strongly absorb or scatter X-ray radiation, and in conjunction with the real-time imaging allows demonstration of dynamic processes, such as peristalsis in the digestive tract or blood flow in arteries and veins. Iodine contrast may also be concentrated in abnormal areas more or less than in normal tissues and make abnormalities (tumors, cysts, inflammation) more conspicuous. Additionally, in specific circumstances air can be used as a contrast agent for the gastrointestinal system and carbon dioxide can be used as a contrast agent in the venous system; in these cases, the contrast agent attenuates the X-ray radiation less than the surrounding tissues.
Interventional radiology
Interventional radiology (abbreviated IR or sometimes VIR for vascular and interventional radiology, also known as Image-Guided Surgery) is a subspecialty of radiology in which minimally invasive procedures are performed using image guidance. Some of these procedures are done for purely diagnostic purposes (e.g., angiogram), while others are done for treatment purposes (e.g., angioplasty).
The basic concept behind interventional radiology is to diagnose or treat pathology with the most minimally invasive technique possible. Interventional radiologists diagnose and treat several disorders including peripheral vascular disease, renal artery stenosis, inferior vena cava filter placement, gastrostomy tube placements, biliary stents and hepatic interventions. Images are used for guidance and the primary instruments used during the procedure are needles and tiny tubes called catheters. The images provide road maps that allow the interventional radiologist to guide these instruments through the body to the areas containing disease. By minimizing the physical trauma to the patient, peripheral interventions can reduce infection rates and recovery time as well as shorten hospital stays. To be a trained interventionalist in the United States, an individual typically requires fifteen years of post-high school training, of which seven years is spent in residency.[2]
CT scanning

CT imaging uses X-rays in conjunction with computing algorithms to image the body.[3] In CT, an X-ray generating tube opposite an X-ray detector (or detectors) in a ring shaped apparatus rotate around a patient producing a computer generated cross-sectional image (tomogram). CT is acquired in the axial plane, while coronal and sagittal images can be rendered by computer reconstruction. Radiocontrast agents are often used with CT for enhanced delineation of anatomy. Although radiographs provide higher spatial resolution, CT can detect more subtle variations in attenuation of X-rays. CT exposes the patient to more ionizing radiation than a radiograph. Spiral Multi-detector CT utilizes 8, 16, 64 or more detectors during continuous motion of the patient through the radiation beam to obtain much finer detail images in a shorter exam time. With rapid administration of IV contrast during the CT scan these fine detail images can be reconstructed into 3D images of carotid, cerebral and coronary arteries, CTA, CT angiography. CT scanning has become the test of choice in diagnosing some urgent and emergent conditions such as cerebral hemorrhage, pulmonary embolism (clots in the arteries of the lungs), aortic dissection (tearing of the aortic wall), appendicitis, diverticulitis, and obstructing kidney stones. Continuing improvements in CT technology including faster scanning times and improved resolution have dramatically increased the accuracy and usefulness of CT scanning and consequently increased utilization in medical diagnosis.
The first commercially viable CT scanner was invented by Sir Godfrey Hounsfield at EMI Central Research Labs, Great Britain in 1972. EMI owned the distribution rights to The Beatles music and it was their profits which funded the research.[4] Sir Hounsfield and Alan McLeod McCormick shared the Nobel Prize for Medicine in 1979 for the invention of CT scanning. The first CT scanner in North America was installed at the Mayo Clinic in Rochester, MN in 1972.
Ultrasound
Medical ultrasonography uses ultrasound (high-frequency sound waves) to visualize soft tissue structures in the body in real time. No ionizing radiation is involved, but the quality of the images obtained using ultrasound is highly dependent on the skill of the person (ultrasonographer) performing the exam. Ultrasound is also limited by its inability to image through air (lungs, bowel loops) or bone. The use of ultrasound in medical imaging has developed mostly within the last 30 years. The first ultrasound images were static and two dimensional (2D), but with modern-day ultrasonography 3D reconstructions can be observed in real-time; effectively becoming 4D.
Because ultrasound does not utilize ionizing radiation, unlike radiography, CT scans, and nuclear medicine imaging techniques, it is generally considered safer. For this reason, this modality plays a vital role in obstetrical imaging. Fetal anatomic development can be thoroughly evaluated allowing early diagnosis of many fetal anomalies. Growth can be assessed over time, important in patients with chronic disease or gestation-induced disease, and in multiple gestations (twins, triplets etc.). Color-Flow Doppler Ultrasound measures the severity of peripheral vascular disease and is used by Cardiology for dynamic evaluation of the heart, heart valves and major vessels. Stenosis of the carotid arteries can presage cerebral infarcts (strokes). DVT in the legs can be found via ultrasound before it dislodges and travels to the lungs (pulmonary embolism), which can be fatal if left untreated. Ultrasound is useful for image-guided interventions like biopsies and drainages such as thoracentesis). Small portable ultrasound devices now replace peritoneal lavage in the triage of trauma victims by directly assessing for the presence of hemorrhage in the peritoneum and the integrity of the major viscera including the liver, spleen and kidneys. Extensive hemoperitoneum (bleeding inside the body cavity) or injury to the major organs may require emergent surgical exploration and repair.
MRI (Magnetic Resonance Imaging)
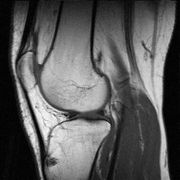
MRI uses strong magnetic fields to align atomic nuclei (usually hydrogen protons) within body tissues, then uses a radio signal to disturb the axis of rotation of these nuclei and observes the radio frequency signal generated as the nuclei return to their baseline states plus all surrounding areas. The radio signals are collected by small antennae, called coils, placed near the area of interest. An advantage of MRI is its ability to produce images in axial, coronal, sagittal and multiple oblique planes with equal ease. MRI scans give the best soft tissue contrast of all the imaging modalities. With advances in scanning speed and spatial resolution, and improvements in computer 3D algorithms and hardware, MRI has become a tool in musculoskeletal radiology and neuroradiology.
One disadvantage is that the patient has to hold still for long periods of time in a noisy, cramped space while the imaging is performed. Claustrophobia severe enough to terminate the MRI exam is reported in up to 5% of patients. Recent improvements in magnet design including stronger magnetic fields (3 teslas), shortening exam times, wider, shorter magnet bores and more open magnet designs, have brought some relief for claustrophobic patients. However, in magnets of equal field strength there is often a trade-off between image quality and open design. MRI has great benefit in imaging the brain, spine, and musculoskeletal system. The modality is currently contraindicated for patients with pacemakers, cochlear implants, some indwelling medication pumps, certain types of cerebral aneurysm clips, metal fragments in the eyes and some metallic hardware due to the powerful magnetic fields and strong fluctuating radio signals the body is exposed to. Areas of potential advancement include functional imaging, cardiovascular MRI, as well as MR image guided therapy.
Nuclear Medicine
Nuclear medicine imaging involves the administration into the patient of radiopharmaceuticals consisting of substances with affinity for certain body tissues labeled with radioactive tracer. The most commonly used tracers are Technetium-99m, Iodine-123, Iodine-131, Gallium-67 and Thallium-201. The heart, lungs, thyroid, liver, gallbladder, and bones are commonly evaluated for particular conditions using these techniques. While anatomical detail is limited in these studies, nuclear medicine is useful in displaying physiological function. The excretory function of the kidneys, iodine concentrating ability of the thyroid, blood flow to heart muscle, etc. can be measured. The principal imaging device is the gamma camera which detects the radiation emitted by the tracer in the body and displays it as an image. With computer processing, the information can be displayed as axial, coronal and sagittal images (SPECT images, single-photon emission computed tomography). In the most modern devices Nuclear Medicine images can be fused with a CT scan taken quasi-simultaneously so that the physiological information can be overlaid or co-registered with the anatomical structures to improve diagnostic accuracy.
Positron emission tomography (PET), scanning also falls under "nuclear medicine." In PET scanning, a radioactive, biologically active substance, most often Fludeoxyglucose (18F), is injected into a patient and the radiation emitted by the patient is detected to produce multi-planar images of the body. Metabolically more active tissues, such as cancer, concentrate the active substance more than normal tissues. PET images can be combined (or "fused") with an anatomic imaging study (currently generally CT images), to more accurately localize PET findings and thereby improve diagnostic accuracy.
Teleradiology
Teleradiology is the transmission of radiographic images from one location to another for interpretation by a radiologist. It is most often used to allow rapid interpretation of emergency room, ICU and other emergent examinations after hours of usual operation, at night and on weekends. In these cases the images are often sent across time zones (i.e. to Spain, Australia, India) with the receiving radiologist working his normal daylight hours. Teleradiology can also be utilized to obtain consultation with an expert or sub-specialist about a complicated or puzzling case.
Teleradiology requires a sending station, high speed Internet connection and high quality receiving station. At the transmission station, plain radiographs are passed through a digitizing machine before transmission, while CT scans, MRIs, Ultrasounds and Nuclear Medicine scans can be sent directly as they are already a stream of digital data. The computer at the receiving end will need to have a high-quality display screen that has been tested and cleared for clinical purposes. The interpreting radiologist then faxes or e-mails the radiology report to the requesting physician.
The major advantage of teleradiology is the ability to utilize different time zones to provide real-time emergency radiology services around-the-clock. The disadvantages include higher costs , limited contact between the ordering physician and the radiologist, and the inability to cover for procedures requiring an onsite radiologist. Laws and regulations concerning the use of teleradiology vary among the states, with some states requiring a license to practice medicine in the state sending the radiologic exam. Some states require the teleradiology report to be preliminary with the official report issued by a hospital staff radiologist.
Radiologist training
United States
Radiology is a competitive field in medicine and successful applicants are often near the top of their medical school class, with high board scores. The field is rapidly expanding due to advances in computer technology, which is closely linked to modern imaging. Diagnostic radiologists must complete at least 13 years of post-high school education, including 4 years of prerequisite undergraduate training, 4 years of medical school, and 5 years of post-graduate training. The first postgraduate year is usually a transitional year of various rotations, but is sometimes a preliminary internship in medicine or surgery. A four-year diagnostic radiology residency follows. The Radiology resident must pass a medical physics board exam covering the science and technology of ultrasound, CTs, x-rays, nuclear medicine and MRI. Core knowledge of the radiologist includes radiobiology, which is the study of the effects of ionizing radiation on living tissue. Near the completion of residency, the radiologist in training is eligible to take the written and oral board examinations administered by the American Board of Radiology (ABR). Starting in 2010, the ABR's board examination structure will be changed to include two computer-based exams, one given after the third year of residency training, and the second given 18 months after the first.
Following completion of residency training, radiologists either begin their practice or enter into sub-speciality training programs known as fellowships. Examples of sub-speciality training in radiology include abdominal imaging, thoracic imaging, CT/Ultrasound, MRI, musculoskeletal imaging, interventional radiology, neuroradiology, interventional neuroradiology, paediatric radiology, mammography and women's imaging. Fellowship training programs in radiology are usually 1 or 2 years in length. [5]
Radiographic exams are usually performed by radiologic technologists, (also known as diagnostic radiographers) who in the United States have a 2-year Associates Degree and the UK a 3 year Honours Degree.
Veterinary radiologists are veterinarians that specialize in the use of X-rays, ultrasound, MRI and nuclear medicine for diagnostic imaging or treatment of disease in animals. They are certified in either diagnostic radiology or radiation oncology by the American College of Veterinary Radiology.
Germany
After obtaining medical licensure, German radiologists complete a 5-year residency, culminating with a board examination (known as Facharztausbildung).
Italy
Until 2008, a Radiology training program had a duration of four years. At present, a radiology training program lasts five years. Further training is required for specialization in radiotherapy or nuclear medicine.
See also
- X-ray image intensifier (C-Arm), equipment that uses x-rays to produce an image feed displayed on a TV screen
- Digital Mammography and PACS
- Interventional radiology, in which minimally invasive procedures are performed using image guidance
- Medical radiography, the use of ionizing electromagnetic radiation, such as X-rays, in medicine
- Positron emission tomography, which produces a three-dimensional image
- Radiobiology, the interdisciplinary science that studies the biological effects of ionizing and non-ionizing radiation of the whole electromagnetic spectrum
- Radiation protection, the science of protecting people and the environment from the harmful effects of ionizing radiation
- Radiography, the use of X-rays to view unseen or hard-to-image objects
- Radiosensitivity, the susceptibility of organic tissues to the harmful effect of ionizing radiation
- Teleradiology, the transmission by electronic means of radiological patient images from one location to another for interpretation or consultation
- Radiology technician
References
- ↑ Novelline, Robert. Squire's Fundamentals of Radiology. Harvard University Press. 5th edition. 1997. ISBN 0674833392.
- ↑ Society of Interventional Radiology -- Global Statement Defining Interventional radiology. http://www.sirweb.org/news/newsPDF/IR_Global_Statement.pdf
- ↑ Herman, G. T., Fundamentals of computerized tomography: Image reconstruction from projection, 2nd edition, Springer, 2009
- ↑ Filler, Aaron (2010). "The History, Development and Impact of Computed Imaging in Neurological Diagnosis and Neurosurgery: CT, MRI, and DTI". Internet Journal of Neurosurgery 7 (1).
- ↑ http://www.healthsystem.virginia.edu/internet/radiology/educ-opps/fellowships.cfm
External links
- Radiology at the Open Directory Project
- MedPix medical imaging database
- MedWorm Radiology directory
- MyPACS medical imaging database
- Radiolopolis an international Radiology community for education, research and clinical practice
- radRounds Radiology Network - Professional and Social Network for Radiology
- DSCT.com international dual source CT experts community for education, research and clinical practice
|
|||||||||||||||||||||||||||||||
|
||||||||||||||||||||||
Bold text