Cleft lip and palate
| Cleft lip and palate | |
|---|---|
| Classification and external resources | |
 Child born with cleft palate, age 5 months |
|
| ICD-10 | Q35.-Q37. |
| ICD-9 | 749 |
| DiseasesDB | 29604 29414 |
| eMedicine | ped/2679 |
Cleft lip (cheiloschisis) and cleft palate (palatoschisis), which can also occur together as cleft lip and palate, are variations of a type of clefting congenital deformity caused by abnormal facial development during gestation. A cleft is a fissure or opening—a gap. It is the non-fusion of the body's natural structures that form before birth. Approximately 1 in 700 children born have a cleft lip and/or a cleft palate. It has sometimes colloquially been equated with the phrase harelip, but this is used incorrectly, as that term refers to the pulling of the lip towards the nose.
Clefts can also affect other parts of the face, such as the eyes, ears, nose, cheeks, and forehead. In 1976, Paul Tessier described fifteen lines of cleft. Most of these craniofacial clefts are even more rare and are frequently described as Tessier clefts using the numerical locator devised by Tessier.[1]
A cleft lip or palate can be successfully treated with surgery, especially so if conducted soon after birth or in early childhood.
Cleft lip and palate
If the cleft does not affect the palate structure of the mouth it is referred to as cleft lip. Cleft lip is formed in the top of the lip as either a small gap or an indentation in the lip (partial or incomplete cleft) or it continues into the nose (complete cleft). Lip cleft can occur as a one sided (unilateral) or two sided (bilateral). It is due to the failure of fusion of the maxillary and medial nasal processes (formation of the primary palate).
 Unilateral incomplete |
 Unilateral complete |
 Bilateral complete |
A mild form of a cleft lip is a microform cleft. A microform cleft can appear as small as a little dent in the red part of the lip or look like a scar from the lip up to the nostril. In some cases muscle tissue in the lip underneath the scar is affected and might require reconstructive surgery. It is advised to have newborn infants with a microform cleft checked with a craniofacial team as soon as possible to determine the severity of the cleft.
 3 month old boy before going into surgery to have his unilateral incomplete cleft lip repaired. |
 The same boy, 1 month after the surgery. |
 Again the same boy, 18 months old. Note how the scar gets less visible with age. |
 6 month old girl before going into surgery to have her unilateral complete cleft lip repaired. |
 The same girl, 1 month after the surgery. |
 Again the same girl, age 5 years old. Note how the scar gets less visible with age. |
Cleft palate
Cleft palate is a condition in which the two plates of the skull that form the hard palate (roof of the mouth) are not completely joined. The soft palate is in these cases cleft as well. In most cases, cleft lip is also present. Cleft palate occurs in about one in 700 live births worldwide.[2]
Palate cleft can occur as complete (soft and hard palate, possibly including a gap in the jaw) or incomplete (a 'hole' in the roof of the mouth, usually as a cleft soft palate). When cleft palate occurs, the uvula is usually split. It occurs due to the failure of fusion of the lateral palatine processes, the nasal septum, and/or the median palatine processes (formation of the secondary palate).
The hole in the roof of the mouth caused by a cleft connects the mouth directly to the nasal cavity.
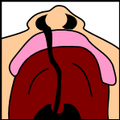
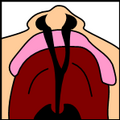
Note: the next images show the roof of the mouth. The top shows the nose, the lips are colored pink. For clarity the images depict a toothless infant.
 Incomplete cleft palate |
 Unilateral complete lip and palate |
 Bilateral complete lip and palate |
A direct result of an open connection between the oral cavity and nasal cavity is velopharyngeal inadequacy (VPI). Because of the gap, air leaks into the nasal cavity resulting in a hypernasal voice resonance and nasal emissions.[3] Secondary effects of VPI include speech articulation errors (e.g., distortions, substitutions, and omissions) and compensatory misarticulations (e.g., glottal stops and posterior nasal fricatives).[4]. Possible treatment options include speech therapy, prosthetics, augmentation of the posterior pharyngeal wall, lengthening of the palate, and surgical procedures.[3]
Submucous cleft palate (SMCP) can also occur, which is an occult cleft of the soft palate with a classic clinical triad of bifid uvula, a furrow along the midline of the soft palate, and a notch in the posterior margin of the hard palate.[5]
Sub-clinical manifestations
The spectrum of severity in visible CL/P is broad, ranging from notches of the vermilion and/or grooves in the philtrum to complete unilateral and bilateral clefts of the lip and palate [6]. At the mild end of the spectrum, studies have described minimal or microform expressions of the CL/P phenotype, typically involving subtle defects of the lip, alveolar arch, and/or inferior nasal region to varying degrees [7]. Histological evidence indicates that these defects extend to the muscle fibers of the superior orbicularis oris (OO) muscle [8]. Martin et al. [9] found histological evidence of defects in the OO muscle in two 18-week fetuses with no obvious visible clefting, suggesting that the CL/P phenotype might also include occult subepithelial clefts, i.e., OO defects in the absence of any overt signs of CL/P. Subsequently, Martin et al. [10] used ultrasonography to visualize subepithelial OO defects in a small sample of non-cleft relatives of individuals with CL/P and healthy controls. Critically, they observed a significant increase in the frequency of OO defects in the non-cleft relatives.
Prevalence among ethnic groups
Prevalence rates reported for live births for Cleft lip with or without Cleft Palate (CL +/- P) and Cleft Palate alone (CPO) varies within different ethnic groups.
The highest prevalence rates for (CL +/- P) are reported for Native Americans and Asians. Africans have the lowest prevalence rates.[11]
- Native Americans: 3.74/1000
- Japanese: 0.82/1000 to 3.36/1000
- Chinese: 1.45/1000 to 4.04/1000
- Caucasians: 1.43/1000 to 1.86/1000
- Latin Americans: 1.04/1000
- Africans: 0.18/1000 to 1.67/1000
Rate of occurrence of CPO is similar for Caucasians, Africans, North American natives, Japanese and Chinese. The trait is dominant.
Prevalence of "cleft uvula" has varied from .02% to 18.8% with the highest numbers found among Chippewa and Navajo and the lowest generally in Africans.
Causes of cleft
The development of the face is coordinated by complex morphogenetic events and rapid proliferative expansion, and is thus highly susceptible to environmental and genetic factors, rationalising the high incidence of facial malformations. During the first six to eight weeks of pregnancy, the shape of the embryo's head is formed. Five primitive tissue lobes grow:
- a) one from the top of the head down towards the future upper lip; (Frontonasal Prominence)
- b-c) two from the cheeks, which meet the first lobe to form the upper lip; (Maxillar Prominence)
- d-e) and just below, two additional lobes grow from each side, which form the chin and lower lip; (Mandibular Prominence)
If these tissues fail to meet, a gap appears where the tissues should have joined (fused). This may happen in any single joining site, or simultaneously in several or all of them. The resulting birth defect reflects the locations and severity of individual fusion failures (e.g., from a small lip or palate fissure up to a completely malformed face).
The upper lip is formed earlier than the palate, from the first three lobes named a to c above. Formation of the palate is the last step in joining the five embryonic facial lobes, and involves the back portions of the lobes b and c. These back portions are called palatal shelves, which grow towards each other until they fuse in the middle.[12] This process is very vulnerable to multiple toxic substances, environmental pollutants, and nutritional imbalance. The biologic mechanisms of mutual recognition of the two cabinets, and the way they are glued together, are quite complex and obscure despite intensive scientific research.[13]
Genetic factors contributing to cleft lip and cleft palate formation have been identified for some syndromic cases, but knowledge about genetic factors that contribute to the more common isolated cases of cleft lip/palate is still patchy.
If a person is born with a cleft, the chances of that person having a child with a cleft, given no other obvious factor, rises to 1 in 14. Many clefts run in families, even though in some cases there does not seem to be an identifiable syndrome present, possibly because of the current incomplete genetic understanding of midfacial development.
Syndromic cases: The Van der Woude Syndrome is caused by a specific variation in the gene IRF6 that increases the occurrence of these deformities threefold.[14][15] Another syndrome, Siderius X-linked mental retardation, is caused by mutations in the PHF8 gene (OMIM 300263); in addition to cleft lip and/or palate, symptoms include facial dysmorphism and mild mental retardation.[16] In some cases, cleft palate is caused by syndromes which also cause other problems. Stickler's Syndrome can cause cleft lip and palate, joint pain, and myopia. Loeys-Dietz syndrome can cause cleft palate or bifid uvula, hypertelorism, and aortic aneurysm. Hardikar syndrome can cause cleft lip and palate, Hydronephrosis, Intestinal obstruction and other symptoms. [17] Cleft lip/palate may be present in many different chromosome disorders including Patau Syndrome (trisomy 13).
Non-syndromic cases: Many genes associated with syndromic cases of cleft lip/palate (see above) have been identified to contribute to the incidence of isolated cases of cleft lip/palate. This includes in particular sequence variants in the genes IRF6, PVRL1 and MSX1.[18] The understanding of the genetic complexities involved in the morphogenesis of the midface, including molecular and cellular processes, has been greatly aided by research on animal models, including of the genes BMP4, SHH, SHOX2, FGF10 and MSX1.[18]
Environmental influences may also cause, or interact with genetics to produce, orofacial clefting. An example for how environmental factors might be linked to genetics comes from research on mutations in the gene PHF8 that cause cleft lip/palate (see above). It was found that PHF8 encodes for a histone lysine demethylase,[19] and is involved in epigenetic regulation. The catalytic activity of PHF8 depends on molecular oxygen,[19] a fact considered important with respect to reports on increased incidence of cleft lip/palate in mice that have been exposed to hypoxia early during pregnancy.[20] In humans, fetal cleft lip and other congenital abnormalities have also been linked to maternal hypoxia, as caused by e.g. maternal smoking,[21] maternal alcohol abuse or some forms of maternal hypertension treatment.[22] Other environmental factors that have been studied include: seasonal causes (such as pesticide exposure); maternal diet and vitamin intake; retinoids - which are members of the vitamin A family; anticonvulsant drugs; alcohol; cigarette use; nitrate compounds; organic solvents; parental exposure to lead; and illegal drugs (cocaine, crack cocaine, heroin, etc).
Current research continues to investigate the extent to which Folic acid can reduce the incidence of clefting.
Diagnosis
Traditionally, the diagnosis is made at the time of birth by physical examination. Recent advances in prenatal diagnosis have allowed obstetricians to diagnose facial clefts in utero.[23]
Treatment
Cleft lip and palate is very treatable; however, the kind of treatment depends on the type and severity of the cleft.
Most children with a form of clefting are monitored by a cleft palate team or craniofacial team through young adulthood. Care can be lifelong. Treatment procedures can vary between craniofacial teams. For example, some teams wait on jaw correction until the child is aged 10 to 12 (argument: growth is less influential as deciduous teeth are replaced by permanent teeth, thus saving the child from repeated corrective surgeries), while other teams correct the jaw earlier (argument: less speech therapy is needed than at a later age when speech therapy becomes harder). Within teams, treatment can differ between individual cases depending on the type and severity of the cleft.
Cleft lip treatment
Within the first 2–3 months after birth, surgery is performed to close the cleft lip. While surgery to repair a cleft lip can be performed soon after birth, the often preferred age is at approximately 10 weeks of age, following the "rule of 10s" coined by surgeons Wilhelmmesen and Musgrave in 1969 (the child is at least 10 weeks of age; weighs at least 10 pounds, and has at least 10g hemoglobin). If the cleft is bilateral and extensive, two surgeries may be required to close the cleft, one side first, and the second side a few weeks later. The most common procedure to repair a cleft lip is the Millard procedure pioneered by Ralph Millard. Millard performed the first procedure at a Mobile Army Surgical Hospital (MASH) unit in Korea.[24]
Often an incomplete cleft lip requires the same surgery as complete cleft. This is done for two reasons. Firstly the group of muscles required to purse the lips run through the upper lip. In order to restore the complete group a full incision must be made. Secondly, to create a less obvious scar the surgeon tries to line up the scar with the natural lines in the upper lip (such as the edges of the philtrum) and tuck away stitches as far up the nose as possible. Incomplete cleft gives the surgeon more tissue to work with, creating a more supple and natural-looking upper lip.
 The blue lines indicate incisions. |
 Movement of the flaps; flap A is moved between B and C. C is rotated slightly while B is pushed down. |
 Pre-operation |
 Post-operation, the lip is swollen from surgery and will get a more natural look within a couple of weeks. See photos in the section above. |
Pre-surgical devices for cleft lip treatment
In some cases of a severe bi-lateral complete cleft, the premaxillary segment will be protruded far outside the mouth.
Nasoalveolar molding followed by surgery can improve long-term nasal symmetry among patients with complete unilateral cleft lip-cleft palate patients compared to surgery alone, according to a retrospective cohort study.[25] Significant improvements in nasal symmetry were observed in the measurements of the projected length of the nasal ala, position of the superoinferior alar groove, position of the mediolateral nasal dome, and nasal bridge deviation. "The nasal ala projection length demonstrated an average ratio of 93.0 percent in the surgery-alone group and 96.5 percent in the nasoalveolar molding group" this study concluded.
Cleft palate treatment
Often a cleft palate is temporarily closed, the cleft isn't closed, but it is covered by a palatal obturator (a prosthetic device made to fit the roof of the mouth covering the gap).
Cleft palate can also be corrected by surgery, usually performed between 6 and 12 months. Approximately 20-25% only require one palatal surgery to achieve a competent velopharyngeal valve capable of producing normal, non-hypernasal speech. However, combinations of surgical methods and repeated surgeries are often necessary as the child grows. One of the new innovations of cleft lip and cleft palate repair is the Latham appliance. The Latham is surgically inserted by use of pins during the child's 4th or 5th month. After it is in place, the doctor, or parents, turn a screw daily to bring the cleft together to assist with future lip and/or palate repair.
If the cleft extends into the maxillary alveolar ridge, the gap is usually corrected by filling the gap with bone tissue. The bone tissue can be acquired from the patients own chin, rib or hip.
Speech and hearing treatments
A tympanostomy tube is often inserted into the eardrum to aerate the middle ear. This is often beneficial for the hearing ability of the child.
Speech problems are usually treated by a speech-language pathologist. In some cases pharyngeal flap surgery or augmentation pharyngoplasty is performed to reduce the escape of nasal airflow in speech sounds requiring oral air pressure, to improve the pronunciation of those sounds, and reduce nasality in those parts of speech that are not normally nasalized. The speech-language pathologist may also be called on to correct incorrect speaking habits that the child developed before the cleft was corrected surgically.
Sample treatment schedule
Note that each individual patient's schedule is treated on a case-by-case basis and can vary per hospital. The table below shows a common sample treatment schedule. The colored squares indicate the average timeframe in which the indicated procedure occurs. In some cases this is usually one procedure (for example lip repair) in other cases this is an ongoing therapy (for example speech therapy).
|
age |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Palatal obturator | ||||||||||||||||||||||
| Repair cleft lip | ||||||||||||||||||||||
| Repair soft palate | ||||||||||||||||||||||
| Repair hard palate | ||||||||||||||||||||||
| Tympanostomy tube | ||||||||||||||||||||||
| Speech therapy/Pharyngoplasty | ||||||||||||||||||||||
| Bone grafting jaw | ||||||||||||||||||||||
| Orthodontics | ||||||||||||||||||||||
| Further cosmetic corrections (Including jawbone surgery) |
Craniofacial team
A craniofacial team is routinely used to treat this condition. The majority of hospitals still use craniofacial teams; yet others are making a shift towards dedicated cleft lip and palate programs. While craniofacial teams are widely knowledgeable about all aspects of craniofacial conditions, dedicated cleft lip and palate teams are able to dedicate many of their efforts to being on the cutting edge of new advances in cleft lip and palate care.
Many of the top pediatric hospitals are developing their own CLP clinics in order to provide patients with comprehensive multi-disciplinary care from birth through adolescence. Allowing an entire team to care for a child throughout their cleft lip and palate treatment (which is ongoing) allows for the best outcomes in every aspect of a child's care. While the individual approach can yield significant results, current trends indicate that team based care leads to better outcomes for CLP patients. .[26]
The members of the craniofacial team at a minimum include a plastic or facial plastic surgeon, or an Oral and maxillofacial surgeon trained in craniofacial surgery, otolaryngologist, geneticist, orthodontist, and social worker.
A complete listing of craniofacial teams in the United States is available through the Cleft Palate Foundation
Complications

Cleft may cause problems with feeding, ear disease, speech and socialization.
Due to lack of suction, an infant with a cleft may have trouble feeding. An infant with a cleft palate will have greater success feeding in a more upright position. Gravity will help prevent milk from coming through the baby's nose if he/she has cleft palate. Gravity feeding can be accomplished by using specialized equipment, such as the Haberman Feeder, or by using a combination of nipples and bottle inserts like the one shown, is commonly used with other infants. A large hole, crosscut, or slit in the nipple, a protruding nipple and rhythmically squeezing the bottle insert can result in controllable flow to the infant without the stigma caused by specialized equipment.
Individuals with cleft also face many middle ear infections which can eventually lead to total hearing loss. The Eustachian tubes and external ear canals may be angled or tortuous, leading to food or other contamination of a part of the body that is normally self cleaning.
Speech is both receptive and expressive. We hear and understand spoken language (receptive) We learn to manipulate our mouth, tongue, oral cavity, to express ourselves (expressive).
Hearing is related to learning to speak. Babies with palatal clefts may have compromised hearing and therefore, if the baby cannot hear, it cannot try to mimic the sounds of speech. Thus, even before expressive language acquisition, the baby with the cleft palate is at risk for receptive language acquisition. Because the lips and palate are both used in pronunciation, individuals with cleft usually need the aid of a speech therapist.
Bonding with the infant, socializing with family and community may be interrupted by the unexpected appearance, unusual speech and the surgical interventions necessary. Support for the parents as well as for the child can be pivotal.
Psychosocial issues
Having a cleft palate/lip does not inevitably lead to a psychosocial problem. Most children who have their clefts repaired early enough are able to have a happy youth and a healthy social life. However, it is important to remember that adolescents with cleft palate/lip are at an elevated risk for developing psychosocial problems especially those relating to self concept, peer relationships, and appearance. It is important for parents to be aware of the psychosocial challenges their adolescents may face and to know where to find professional help if problems arise.
A cleft palate/lip may impact an individual’s self-esteem, social skills, and behavior. There is a large amount of research dedicated to the psychosocial development of individuals with cleft palate. Self-concept may be adversely affected by the presence of a cleft lip and or cleft palate. Research has shown that during the early preschool years (ages 3–5), children with cleft lip and or cleft palate tend to have a self-concept that is similar to their peers without a cleft. However, as they grow older and their social interactions with other children increase, children with clefts tend to report more dissatisfaction with peer relationships and higher levels of social anxiety. Experts conclude that this is probably due to the associated stigma of visible deformities and speech abnormalities, if present. Children who are judged as attractive tend to be perceived as more intelligent, exhibit more positive social behaviors, and are treated more positively than children with cleft lip and or cleft palate.[27] Children with clefts tend to report feelings of anger, sadness, fear, and alienation from their peers. Yet these children were similar to their peers in regard to "how well they liked themselves."
The relationship between parental attitudes and a child’s self-concept is crucial during the preschool years. It has been reported that elevated stress levels in mothers correlated with reduced social skills in their children.[28] Strong parent support networks may help to prevent the development of negative self-concept in children with cleft palate . In the later preschool and early elementary years, the development of social skills is no longer only impacted by parental attitudes but is beginning to be shaped by their peers. A cleft lip and or cleft palate may affect the behavior of preschoolers. Experts suggest that parents discuss with their children ways to handle negative social situations related to their cleft lip and or cleft palate. A child who is entering school should learn the proper (and age-appropriate) terms related to the cleft. The ability to confidently explain the condition to others may limit feelings of awkwardness and embarrassment and reduce negative social experiences.[29]
As children reach adolescence, the period of time between age 13 and 19, the dynamics of the parent-child relationship change as peer groups are now the focus of attention. An adolescent with cleft lip and or cleft palate will deal with the typical challenges faced by most of their peers including issues related to self esteem, dating, and social acceptance.[30][31][32] Adolescents, however, view appearance as the most important characteristic above intelligence and humor.[33] This being the case, adolescents are susceptible to additional problems because they cannot hide their facial differences from their peers. Adolescent boys typically deal with issues relating to withdrawal, attention, thought, and internalizing problems and may possibly develop anxiousness-depression and aggressive behaviors.[32] Adolescent girls are more likely to develop problems relating to self concept and appearance. Individuals with cleft lip and or cleft palate often deal with threats to their quality of life for multiple reasons including: unsuccessful social relationships, deviance in social appearance, and multiple surgeries.
Controversy
In some countries, cleft lip or palate deformities are considered reasons (either generally tolerated or officially sanctioned) to perform abortion beyond the legal fetal age limit, even though the fetus is not in jeopardy of life or limb. Some human rights activists contend this practice of "cosmetic murder" amounts to eugenics. British clergywoman Joanna Jepson, who suffered from a congenital jaw deformity herself (not a cleft lip or palate as is sometimes reported), has started legal action to stop the practice in the United Kingdom[34][35] (although in the United Kingdom, such an abortion would not be permitted under the 1967 Abortion Act, because a cleft lip and palate is not considered a serious handicap).
The Japanese anime Ghost Stories arose some controversy when people complained of an episode featuring a Kuchisake-onna (a ghost who is said to have a Glasgow smile through her face) because her scar resembled cleft lip.[36]
Famous people born with a cleft
| Name | Comments | |
|---|---|---|
| John Henry "Doc" Holliday | American dentist, gambler and gunfighter of the American Old West, who is usually remembered for his friendship with Wyatt Earp and the Gunfight at the O.K. Corral | [37] |
| Tutankhamen | Egyptian pharaoh who may have had a slightly cleft palate according to diagnostic imaging | [38] |
| Thorgils Skarthi | Thorgils 'the hair-lipped' - a 10th century viking warrior and founder of Scarborough, England. | [39] |
| Tad Lincoln | Fourth and youngest son of President Abraham Lincoln | [40] |
| Carmit Bachar | American dancer and singer | [41][42] |
| Jürgen Habermas | German philosopher and sociologist | [43] |
| Ljubo Milicevic | Australian professional footballer | [44] |
| Stacy Keach | American actor and narrator | [45] |
| Cheech Marin | American actor and comedian | [46] |
| Chin-Chin | American magician and stage illusionist | [47] |
| Owen Schmitt | American football fullback | [48] |
Cleft lip and palate in animals
Cleft lips and palates are occasionally seen in cattle and dogs, and rarely in sheep, cats, horses, pandas and ferrets. Most commonly, the defect involves the lip, rhinarium, and premaxilla. Clefts of the hard and soft palate are sometimes seen with a cleft lip. The cause is usually hereditary. Brachycephalic dogs such as Boxers and Boston Terriers are most commonly affected.[49] An inherited disorder with incomplete penetrance has also been suggested in Shih tzus, Swiss Sheepdogs, Bulldogs, and Pointers.[50] In horses, it is a rare condition usually involving the caudal soft palate.[51] In Charolais cattle, clefts are seen in combination with arthrogryposis, which is inherited as an autosomal recessive trait. It is also inherited as an autosomal recessive trait in Texel sheep. Other contributing factors may include maternal nutritional deficiencies, exposure in utero to viral infections, trauma, drugs, or chemicals, or ingestion of toxins by the mother, such as certain lupines by cattle during the second or third month of gestation.[52] The use of corticosteroids during pregnancy in dogs and the ingestion of Veratrum californicum by pregnant sheep have also been associated with cleft formation.[53]
Difficulty with nursing is the most common problem associated with clefts, but aspiration pneumonia, regurgitation, and malnutrition are often seen with cleft palate and is a common cause of death. Providing nutrition through a feeding tube is often necessary, but corrective surgery in dogs can be done by the age of twelve weeks.[49] For cleft palate, there is a high rate of surgical failure resulting in repeated surgeries.[54] Surgical techniques for cleft palate in dogs include prosthesis, mucosal flaps, and microvascular free flaps.[55] Affected animals should not be bred due to the hereditary nature of this condition.
|
Cleft lip in a Boxer |
Cleft lip in a Boxer with premaxillary involvement |
Same dog as picture on left, one year later |
See also
Associated genes
- GAD1,[56] one of the glutamate decarboxylases
Movies showing on this topic
- Smile Pinki
Treatment and aids
- Oral and maxillofacial surgery
- Haberman Feeder
- Palatal obturator
- Vomer flap surgery
Syndromes
- Hearing loss with craniofacial syndromes
- Popliteal pterygium syndrome
- Van der Woude syndrome
General support discussion boards
- Face Forward - The UK's Number One Discussion Boards , For Both Patients And Parents
- cleftAdvocate's Family-to-Family Connection Listserv
Organizations
- List of Cleft lip & palate organizations
References
- ↑ Tessier, Paul (June 4, 1976). J Maxillofac Surg. pp. 69–92.
- ↑ "Statistics by country for cleft palate". WrongDiagnosis.com. http://www.wrongdiagnosis.com/c/cleft_palate/stats-country.htm. Retrieved 2007-04-24.
- ↑ 3.0 3.1 Sloan GM (2000). "Posterior pharyngeal flap and sphincter pharyngoplasty: the state of the art". Cleft Palate Craniofac. J. 37 (2): 112–22. doi:10.1597/1545-1569(2000)037<0112:PPFASP>2.3.CO;2. PMID 10749049.
- ↑ Hill, J.S. (2001). Velopharyngeal insufficiency: An update on diagnostic and surgical techniques. Current Opinion in Otolaryngology and Head and Neck Surgery, 9, 365-368.
- ↑ Kaplan EN (1975). "The Occult and Submucous Cleft Palate". Cleft Palate Journal 12: 356–68. PMID 1058746.
- ↑ [Gorlin et al., 2001; Eppley et al., 2005]
- ↑ [Cosman and Crikelair; 1966; Carstens, 2000; Mulliken, 2005]
- ↑ [Lehman and Artz, 1976; Heckler et al., 1979]
- ↑ [1993]
- ↑ Martin RA, Hunter V, Neufeld-Kaiser W, et al. (January 2000). "Ultrasonographic detection of orbicularis oris defects in first degree relatives of isolated cleft lip patients". Am. J. Med. Genet. 90 (2): 155–61. doi:10.1002/(SICI)1096-8628(20000117)90:2<155::AID-AJMG13>3.0.CO;2-V. PMID 10607956.
- ↑ See "Who is affected by cleft lip and cleft palate". http://www.webmd.com/hw-popup/who-is-affected-by-cleft-lip-and-cleft-palate. Retrieved 2008-06-20.
- ↑ Dudas et al. (2007): Palatal fusion – Where do the midline cells go? A review on cleft palate, a major human birth defect. Acta Histochemica, Volume 109, Issue 1, 1 March 2007, Pages 1-14
- ↑ Dudas M, Li WY, Kim J, Yang A, Kaartinen V (2007). "Palatal fusion - where do the midline cells go? A review on cleft palate, a major human birth defect". Acta Histochem. 109 (1): 1–14. doi:10.1016/j.acthis.2006.05.009. PMID 16962647.
- ↑ Zucchero, T.M. et al. 2004 Interferon Regulatory Factor 6 (IRF6) Gene Variants and the Risk of Isolated Cleft Lip or Palate New England Journal of Medicine 351:769-780 [1]
- ↑ "Cleft palate genetic clue found". BBC News. 2004-08-30. http://news.bbc.co.uk/1/hi/health/3577784.stm. Retrieved 2007-07-01.
- ↑ Siderius LE, Hamel BC, van Bokhoven H, et al. (2000). "X-linked mental retardation associated with cleft lip/palate maps to Xp11.3-q21.3.". Am. J. Med. Genet. 85 (3): 216–220. doi:10.1002/(SICI)1096-8628(19990730)85:3<216::AID-AJMG6>3.0.CO;2-X. PMID 10398231.
- ↑ Hardikar syndrome symptoms
- ↑ 18.0 18.1 Cox, T. C. (2004). "Taking it to the max: The genetic and developmental mechanisms coordinating midfacial morphogenesis and dysmorphology". Clin. Genet. 65 (3): 163–176. doi:10.1111/j.0009-9163.2004.00225.x. PMID 14756664.
- ↑ 19.0 19.1 Loenarz, C.; Ge W., Coleman M. L., Rose N. R., Cooper C. D. O., Klose R. J., Ratcliffe P. J., Schofield, C. J. (2009). "PHF8, a gene associated with cleft lip/palate and mental retardation, encodes for an N{varepsilon}-dimethyl lysine demethylase". Hum. Mol. Genet.. doi:10.1093/hmg/ddp480. PMID 19843542.
- ↑ Millicovsky, G.; Johnston, M.C. (1981). "Hyperoxia and hypoxia in pregnancy: simple experimental manipulation alters the incidence of cleft lip and palate in CL/Fr mice". Proc. Natl. Acad. Sci. U. S. A. 78 (9): 5722–5723. doi:10.1073/pnas.78.9.5722. PMID 6946511.
- ↑ Shi, M.; Wehby, G.L. and Murray, J.C. (2008). "Review on genetic variants and maternal smoking in the etiology of oral clefts and other birth defects". Birth Defects Res., Part C 84 (1): 16–29. doi:10.1002/bdrc.20117. PMID 18383123.
- ↑ Hurst, J. A.; Houlston, R.S., Roberts, A., Gould, S.J. and Tingey, W.G. (1995). "Transverse limb deficiency, facial clefting and hypoxic renal damage: an association with treatment of maternal hypertension?". Clin. Dysmorphol. 4 (4): 359–363. PMID 8574428.
- ↑ PMID 18848093
- ↑ "Biography and Personal Archive". http://calder.med.miami.edu/Ralph_Millard/biography.html. Retrieved 2007-07-01. at miami.edu
- ↑ PMID 19319066
- ↑ Joanne Green. "The Importance of a Multi-Disciplinary Approach". http://www.widesmiles.org/cleftlinks/WS-359.html. Retrieved 2007-10-15.
- ↑ Tobiasen, J.M. (1984) Psychosocial correlated of congenital facial clefts: a conceptualization and model. Cleft Palate Journal, 21, 131-139.
- ↑ Pope AW, Ward J (1997). "Self-perceived facial appearance and psychosocial adjustment in preadolescents with craniofacial anomalies". Cleft Palate Craniofac. J. 34 (5): 396–401. doi:10.1597/1545-1569(1997)034<0396:SPFAAP>2.3.CO;2. PMID 9345606.
- ↑ "Cleft Palate Foundation". http://cleftline.org. Retrieved 2007-07-01.
- ↑ Snyder HT, Bilboul MJ, Pope AW (2005). "Psychosocial adjustment in adolescents with craniofacial anomalies: a comparison of parent and self-reports". Cleft Palate Craniofac. J. 42 (5): 548–55. doi:10.1597/04-078R.1. PMID 16149838.
- ↑ Endriga MC, Kapp-Simon KA (1999). "Psychological issues in craniofacial care: state of the art". Cleft Palate Craniofac. J. 36 (1): 3–11. doi:10.1597/1545-1569(1999)036<0001:PIICCS>2.3.CO;2. PMID 10067755.
- ↑ 32.0 32.1 Pope, A.W. & Snyder, H.T. (2004). Psychosocial adjustment in children and adolescents with a craniofacial anomaly: Age and sex patterns. The Cleft Palate-Craniofacial Journal, 42, 4.
- ↑ Prokohorov, A.V., Perry, C.L., Kelder, S.H., & Klepp, K.I. (1993). Lifestyle values of adolescents: Results from the Minnesota Heart Health Youth Program. Adolescence, 28.
- ↑ "CNN.com - Priest challenges late abortion - Dec. 1, 2003". 2003-12-01. http://www.cnn.com/2003/WORLD/europe/12/01/uk.curate.abortion/index.html. Retrieved 2007-07-01.
- ↑ "CPS examines late abortion case". BBC News. 2004-09-22. http://news.bbc.co.uk/1/hi/england/hereford/worcs/3680162.stm. Retrieved 2007-07-01.
- ↑ [2]
- ↑ "Doc Holliday: A Family Portrait", Karen Holliday Tanner, University of Omaha Press, 1998, ISBN 0-8061-3036-9.
- ↑ "King Tut Not Murdered Violently, CT Scans Show". http://news.nationalgeographic.com/news/2005/03/0308_050308_kingtutmurder_2.html. Retrieved 2007-07-01.
- ↑ Bloodfeud: Murder and Revenge in Anglo-Saxon England, Richard Fletcher
- ↑ "HistoryBuff.com -- Tad Lincoln: The Not-so-Famous Son of A Most-Famous President". http://www.historybuff.com/library/reftad.html. Retrieved 2007-07-01.
- ↑ "Carmit Bachar, smile ambassador". http://www.buddytv.com/articles/pussycat-dolls-present-the-search-for-the-next-doll/pussycat-dolls-carmit-bachar-i-12393.aspx. Retrieved 2007-10-13.
- ↑ Beverley Lyons, October 16, 2006. Carmite Doing Her Bit For Charity. The Daily Record
- ↑ "Jurgen Habermas". http://www.nyu.edu/classes/stephens/Habermas%20page.htm. Retrieved 2008-12-18.
- ↑ "Chat To Ljubo...LIVE". 28 May 2009. http://au.fourfourtwo.com/news/104299,chat-to-ljubolive.aspx. Retrieved 23 December 2009.
- ↑ "Stacy Keach". http://www.cleftline.org/story_of_the_month/oct02. Retrieved 2007-07-01.
- ↑ "Cheech Marin". http://www.disabled-world.com/artman/publish/famous-cleft.shtml//oct02. Retrieved 2007-07-01.
- ↑ "Chin-Chin". http://www.chin-chin.com. Retrieved 2007-07-01.
- ↑ Whiteside, Kelly (4 Nov 2006). "Schmitt is face of West Va. toughness". http://www.usatoday.com/sports/college/football/bigeast/2006-11-01-wvu-schmitt_x.htm. Retrieved 2010-04-30.
- ↑ 49.0 49.1 Ettinger, Stephen J.;Feldman, Edward C. (1995). Textbook of Veterinary Internal Medicine (4th ed.). W.B. Saunders Company. ISBN 0-7216-6795-3.
- ↑ Garcia, J.F. Rodriguez (2006). "Surgery of the Soft and Hard Palate". Proceedings of the North American Veterinary Conference. http://www.ivis.org/proceedings/navc/2006/SAE/516.asp?LA=1. Retrieved 2007-04-28.
- ↑ Semevolos, Stacy A.; Ducharme, Norm (1998). "Surgical Repair of Congenital Cleft Palate in Horses: Eight Cases (1979–1997)" (PDF). Proceedings of the American Association of Equine Practitioners. http://www.ivis.org/proceedings/AAEP/1998/Semevolo.pdf. Retrieved 2007-04-28.
- ↑ "Mouth". The Merck Veterinary Manual. 2006. http://www.merckvetmanual.com/mvm/index.jsp?cfile=htm/bc/20202.htm. Retrieved 2007-04-28.
- ↑ Beasley, V. (1999). "Teratogenic Agents". Veterinary Toxicology. http://www.ivis.org/advances/Beasley/cpt8a/chapter_frm.asp?LA=1&table=1. Retrieved 2007-04-28.
- ↑ Lee J, Kim Y, Kim M, Lee J, Choi J, Yeom D, Park J, Hong S (2006). "Application of a temporary palatal prosthesis in a puppy suffering from cleft palate". J. Vet. Sci. 7 (1): 93–5. PMID 16434860.
- ↑ Griffiths L, Sullivan M (2001). "Bilateral overlapping mucosal single-pedicle flaps for correction of soft palate defects". Journal of the American Animal Hospital Association 37 (2): 183–6. PMID 11300527.
- ↑ Kanno, K.; Suzuki, Y.; Yamada, A.; Aoki, Y.; Kure, S.; Matsubara, Y. : Association between nonsyndromic cleft lip with or without cleft palate and the glutamic acid decarboxylase 67 gene in the Japanese population. Am. J. Med. Genet. 127A: 11-16, 2004. PMID 15103710
External links
- Cleft lip and palate - Institute of Reconstructive Plastic Surgery @ NYU Langone Medical Center
- Cleft lip and palate - Children's Hospital Boston
- Cleft lip and palate and before/after patient photos - University of Missouri Children's Hospital
|
|||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||