Norovirus
| Norovirus | |
|---|---|
 |
|
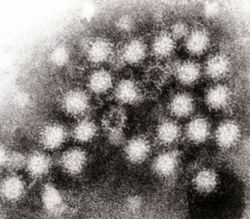
| Transmission electron micrograph of noroviruses. The bar = 50 nm | |
| Virus classification | |
| Group: | Group IV ((+)ssRNA) |
| Family: | Caliciviridae |
| Genus: | Norovirus |
Norovirus (formerly Norwalk agent) is an RNA virus (taxonomic family Caliciviridae) that causes approximately 90% of epidemic non-bacterial outbreaks of gastroenteritis around the world,[1] and may be responsible for 50% of all foodborne outbreaks of gastroenteritis in the US.[2][3] Norovirus affects people of all ages. The viruses are transmitted by faecally contaminated food or water, by person-to-person contact,[4] and via aerosolization of the virus and subsequent contamination of surfaces.[5]
After infection, immunity to norovirus is usually incomplete and temporary.[6] There is an inherited predisposition to infection, and individuals with blood type O are more often infected,[1][7] while blood types B and AB can confer partial protection against symptomatic infection.[8][9]
Outbreaks of norovirus infection often occur in closed or semi-closed communities, such as long-term care facilities, overnight camps, hospitals, prisons, dormitories, and cruise ships where the infection spreads very rapidly either by person-to-person transmission or through contaminated food.[10] Many norovirus outbreaks have been traced to food that was handled by one infected person.[11]
Norovirus is rapidly inactivated by sufficient heating and by chlorine-based disinfectants, but the virus is less susceptible to alcohols and detergents as it does not have a lipid envelope.[12]
Contents |
History
The norovirus was originally named the Norwalk agent after Norwalk, Ohio, USA, where an outbreak of acute gastroenteritis occurred among children at Bronson Elementary School in November 1968. The name was shortened to norovirus after being identified in a number of outbreaks on cruise ships and receiving attention throughout the USA. In 1972, electron microscopy on stored human stool samples identified a virus, which was given the name Norwalk virus. Numerous outbreaks with similar symptoms have been reported since. The cloning and sequencing of the Norwalk virus genome showed that these viruses have a genomic organization consistent with viruses belonging to the family Caliciviridae.[13] The name norovirus (Norovirus for the genus) was approved by the International Committee on Taxonomy of Viruses in 2002.[14]
Common names of the illness caused by noroviruses are winter vomiting disease, viral gastroenteritis, and acute non-bacterial gastroenteritis,[4] also colloquially known as "stomach flu"—a broad name that refers to gastric inflammation caused by a range of viruses and bacteria.
The virus has previously been called Norwalk virus, Norwalk-like virus, SRSVs (Small Round Structured Viruses), and Snow Mountain virus.[15]
Pathology
When a person becomes infected with norovirus, the virus begins to multiply within the small intestine. After approximately 1 to 2 days, norovirus symptoms can appear. The principal symptom is acute gastroenteritis that develops between 24 and 48 hours after exposure, and lasts for 24–60 hours.[3] The disease is usually self-limiting, and characterized by nausea, vomiting, diarrhea, and abdominal pain; and in some cases, loss of taste. General lethargy, weakness, muscle aches, headache, and low-grade fever may occur.
Severe illness is rare: although people are frequently treated at the emergency ward, they are rarely admitted to the hospital. The number of deaths from norovirus in the US is estimated to be around 300 each year, with most of these occurring in the very young, elderly and persons with weakened immune systems. Symptoms may become life-threatening in these groups if dehydration is ignored or not treated.[4]
The most common genotype identified in hospitalized children was GII.4 and increased amount of virus (7.2 x 107) were shed by those children. Even though GII.4 Norovirus was the most common identified, other genotypes were identified in less proportion, including the novel GII.18-NICA.
Diagnosis
Specific diagnosis of norovirus is routinely made by polymerase chain reaction (PCR) assays or real-time PCR assays, which give results within a few hours. These assays are very sensitive and can detect concentrations as low as 10 virus particles.[16]
Tests such as ELISA that use antibodies against a mixture of norovirus strains are available commercially but lack specificity and sensitivity.[17]
Epidemiology, prevention and infection control
Noroviruses are transmitted directly from person to person and indirectly via contaminated water and food. They are highly contagious, with as few as ten virus particles being able to cause infection. Transmission occurs through ingesting contaminated food and water and by person-to-person spread. Transmission is predominantly fecal-oral but may be airborne due to aerosolisation of vomit. Norovirus can be aerosolized when those stricken with the illness vomit; infection can follow eating food near an episode of vomiting, even if cleaned up[18]. The viruses continue to be shed after symptoms have subsided and shedding can still be detected many weeks after infection.[19]
Norovirus is extremely infectious. In one outbreak at an international scout jamboree in the Netherlands, each person with gastroenteritis infected an average of 14 people before increased hygiene measures were put in place. Even after these new measures were enacted an average ill person still infected 2.1 other people.[20] A CDC study of eleven outbreaks in New York State lists the suspected mode of transmission as person-to-person in seven outbreaks, foodborne in two, waterborne in one, and one unknown. The source of waterborne outbreaks may include water from municipal supplies, wells, recreational lakes, swimming pools and ice machines.[21]
Shellfish and salad ingredients are the foods most often implicated in norovirus outbreaks. Ingestion of shellfish that have not been sufficiently heated poses a high risk for norovirus infection. Foods other than shellfish may be contaminated by infected food handlers.[22]
Hand washing is an effective method to reduce the spread of norovirus pathogens. Sanitizing of surfaces where the norovirus may be present is recommended. Alcohol rubs are not very effective at dealing with Norovirus.
In health-care environments, the prevention of nosocomial infections involves routine and terminal cleaning. Nonflammable alcohol vapor in CO2 systems are used in health care environments where medical electronics would be adversely affected by aerosolized chlorine or other caustic compounds.[23]
Ligocyte announced in 2007 that it was working on a vaccine and had started phase 1 trials.[24]
Epidemiological data from developing countries about the importance of norovirus in pediatric diarrhea is limited. Recently, in Nicaragua, it has been observed that norovirus is responsible for 11% of the diarrhea cases occurring in children <5 years of age at community level and 15% of the moderate to severe cases requiring intravenous re-hydration.[25]
Detection of norovirus in foods
Routine protocols to detect norovirus (norovirus RNA) in clams and oysters by RT-PCR (reverse transcription polymerase chain reaction) are being employed by governmental laboratories such as the FDA in the USA. However, routine methods to detect the virus on other food items are not readily available due to the variable nature of different food items affecting concentration and extraction of the virus and presence of factors that make PCR (polymerase chain reaction) analysis techniques ineffective.[26]
Microbiology
Classification
Noroviruses (NoV) are a genetically diverse group of single stranded RNA, nonenveloped viruses belonging to the Caliciviridae family.[27] According to the International Committee on Taxonomy of Virus, the genus Norovirus has one species, which is called "Norwalk virus" and assigned the abbreviation "NV". Serotypes, strains and isolates include:[28]
- Norwalk virus [M87661] (Hu/NLV/NV/1968/US)
- Hawaii virus [U07611] (Hu/NLV/HV/1971/US)
- Snow Mountain virus [L23831] (Hu/NLV/SMV/1976/US)
- Mexico virus [U22498] (Hu/NLV/MX/1989/MX)
- Desert Shield virus [U04469] (Hu/NLV/DSV395/1990/SR)
- Southampton virus [L07418] (Hu/NLV/SHV/1991/UK)
- Lordsdale virus [X86557] (Hu/NLV/LD/1993/UK)
Noroviruses commonly isolated in cases of acute gastroenteritis belong to two genogroups: genogroup I (GI) includes Norwalk virus, Desert Shield virus and Southampton virus and II (GII), which includes Bristol virus, Lordsdale virus, Toronto virus, Mexico virus, Hawaii virus and Snow Mountain virus.[27]
Noroviruses can genetically be classified into 5 different genogroups (GI, GII, GIII, GIV, and GV), which can be further divided into different genetic clusters or genotypes. For example genogroup II, the most prevalent human genogroup, presently contains 19 genotypes. Genogroups I, II and IV infect humans, whereas genogroup III infects bovine species and genogroup V has recently been isolated in mice.[29]
Most noroviruses that infect humans belong to genogroup GI and GII.[30] Noroviruses from Genogroup II, genotype 4 (abbreviated as GII.4) account for the majority of adult outbreaks of gastroenteritis and often sweep across the globe. Recent examples include US95/96-US strain, associated with global outbreaks in the mid- to late-90s, Farmington Hills virus associated with outbreaks in Europe and the United States in 2002 and in 2004 Hunter virus was associated with outbreaks in Europe, Japan and Australasia. In 2006 there was another large increase in NoV infection around the globe.[31] Two new GII.4 variants caused around 80% of those Norovirus associated outbreaks and they have been termed 2006a and 2006b. Recent reports have shown a link between blood group and susceptibility to infection by norovirus.[32][33][34]
A study performed by scientists at Washington University School of Medicine in St. Louis, published in the journal PLoS Pathogens (July 18, 2008), suggests that the protein MDA-5 may be the primary immune sensor that detects the presence of noroviruses in the body.[35] Interestingly, some people have common variations of the MDA-5 gene that could make them more susceptible to norovirus infection.[36]
Another study at Washington University School of Medicine in June 2010 suggested that a specific genetic version of Norovirus (which would not be distinguishable from other types of the virus using standard viral antibody tests) interacts with a specific mutation in the Atg16L1 gene to help trigger symptomatic Crohn's Disease in mice that have been subjected to a chemical that causes intestinal injury similar to the process in humans (there are other similar ways for such diseases to happen like this, and this study in itself does not prove that Norovirus causes Crohn's in humans).
Virus structure
Noroviruses contain a positive-sense RNA genome of approximately 7.5 knt, encoding a major structural protein (VP1) of about 58~60 kDa and a minor capsid protein (VP2).[37] The virus particles demonstrate an amorphous surface structure when visualized using electron microscopy and are between 27-38 nm in size.[38]
References
- ↑ 1.0 1.1 Lindesmith L, Moe C, Marionneau S, et al. (2003). "Human susceptibility and resistance to Norwalk virus infection". Nat. Med. 9 (5): 548–53. doi:10.1038/nm860. PMID 12692541.
- ↑ Widdowson MA, Sulka A, Bulens SN, et al. (2005). "Norovirus and foodborne disease, United States, 1991-2000". Emerging Infect. Dis. 11 (1): 95–102. PMID 15705329. http://www.cdc.gov/ncidod/EID/vol11no01/04-0426.htm.
- ↑ 3.0 3.1 "Norovirus: Technical Fact Sheet". National Center for Infectious Diseases, CDC. http://www.cdc.gov/ncidod/dvrd/revb/gastro/norovirus-factsheet.htm.
- ↑ 4.0 4.1 4.2 Goodgame R (2006). "Norovirus gastroenteritis". Curr Gastroenterol Rep 8 (5): 401–8. doi:10.1007/s11894-006-0026-4. PMID 16968608.
- ↑ Said MA, Perl TM, Sears CL (November 2008). "Healthcare epidemiology: gastrointestinal flu: norovirus in health care and long-term care facilities". Clinical Infectious Diseases : an Official Publication of the Infectious Diseases Society of America 47 (9): 1202–8. doi:10.1086/592299. PMID 18808354. http://www.journals.uchicago.edu/doi/abs/10.1086/592299?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dncbi.nlm.nih.gov.
- ↑ Lindesmith L, Moe C, Lependu J, Frelinger JA, Treanor J, Baric RS (2005). "Cellular and humoral immunity following Snow Mountain virus challenge". J. Virol. 79 (5): 2900–9. doi:10.1128/JVI.79.5.2900-2909.2005. PMID 15709009. PMC 548455. http://jvi.asm.org/cgi/pmidlookup?view=long&pmid=15709009.
- ↑ Hutson, AM; Atmar RL, Graham DY, Estes MK. (July 2003). "Norwalk virus infection and disease is associated with ABO histo-blood group type". Journal of Infectious Diseases 188 (1): 176–7. doi:10.1086/375829. PMID 12825190. http://www.ncbi.nlm.nih.gov/pubmed/12001052?dopt=Abstract.
- ↑ "Norwalk Virus Infection and Disease Is Associated with ABO Histo-Blood Group Type". The Journal of Infectious Diseases. 2002. http://www.journals.uchicago.edu/cgi-bin/resolve?doi=10.1086/339883&erFrom=-6346711085704863031Guest/. Retrieved 2007-02-05.
- ↑ "Binding of Norwalk Virus-Like Particles to ABH Histo-Blood Group Antigens Is Blocked by Antisera from Infected Human Volunteers or Experimentally Vaccinated Mice". Journal of Virology. 2002. http://jvi.asm.org/cgi/content/full/76/23/12335/. Retrieved 2007-02-05.
- ↑ Noda M, Fukuda S, Nishio O (2007). "Statistical analysis of attack rate in norovirus foodborne outbreaks". Int J Food Microbiol 122 (1-2): 216. doi:10.1016/j.ijfoodmicro.2007.11.073. PMID 18177970. http://linkinghub.elsevier.com/retrieve/pii/S0168-1605(07)00662-9.
- ↑ Koopmans M, Duizer E (2004). "Foodborne viruses: an emerging problem". Int. J. Food Microbiol. 90 (1): 23–41. doi:10.1016/S0168-1605(03)00169-7. PMID 14672828. http://linkinghub.elsevier.com/retrieve/pii/S0168160503001697.
- ↑ Jimenez L, Chiang M (2006). "Virucidal activity of a quaternary ammonium compound disinfectant against feline calicivirus: a surrogate for norovirus". Am J Infect Control 34 (5): 269–73. doi:10.1016/j.ajic.2005.11.009. PMID 16765204. http://linkinghub.elsevier.com/retrieve/pii/S0196-6553(06)00078-2.
- ↑ Kapikian AZ (1996). "Overview of viral gastroenteritis". Arch. Virol. Suppl. 12: 7–19. PMID 9015097.
- ↑ ICTVdB Management (2006). 00.012.0.03. Norovirus. In: ICTVdB — The Universal Virus Database, version 4. Büchen-Osmond, C. (Ed), Columbia University, New York, USA
- ↑ Appleton H (1987). "Small round viruses: classification and role in food-borne infections". Ciba Found. Symp. 128: 108–25. PMID 3036438.
- ↑ Marshall JA, Bruggink LD (2006). "Laboratory diagnosis of norovirus". Clin. Lab. 52 (11-12): 571–81. PMID 17175887.
- ↑ Wilhelmi de Cal I, Revilla A, del Alamo JM, Román E, Moreno S, Sánchez-Fauquier A (2007). "Evaluation of two commercial enzyme immunoassays for the detection of norovirus in faecal samples from hospitalised children with sporadic acute gastroenteritis". Clin. Microbiol. Infect. 13 (3): 341–3. doi:10.1111/j.1469-0691.2006.01594.x. PMID 17391396. http://www.blackwell-synergy.com/openurl?genre=article&sid=nlm:pubmed&issn=1198-743X&date=2007&volume=13&issue=3&spage=341.
- ↑ "I've lost my appetite...": New Scientist article on spread of viral food poisoning across a restaurant by eating near where someone has vomited
- ↑ Atmar RL, Opekun AR, Gilger MA, et al. (October 2008). "Norwalk virus shedding after experimental human infection". Emerging Infect. Dis. 14 (10): 1553–7. doi:10.3201/eid1410.080117. PMID 18826818.
- ↑ Heijne JCM, Teunis P, Morroy G, et al. (2009). "Enhanced hygiene measures and norovirus transmission during an outbreak". Emerg. Infect. Dis. 15 (1): 24–30. doi:10.3201/1501.080299. PMID 19116045. PMC 2660689. http://www.cdc.gov/EID/content/15/1/pdfs/24.pdf.
- ↑ Hedberg CW, Osterholm MT (1993). "Outbreaks of food-borne and waterborne viral gastroenteritis". Clin. Microbiol. Rev. 6 (3): 199–210. PMID 8395330. PMC 358282. http://cmr.asm.org/cgi/pmidlookup?view=long&pmid=8395330.
- ↑ Parashar UD, Monroe SS (2001). ""Norwalk-like viruses" as a cause of foodborne disease outbreaks". Rev. Med. Virol. 11 (4): 243–52. doi:10.1002/rmv.321. PMID 11479930.
- ↑ Chadwick PR, Beards G, Brown D, Caul EO, Cheesbrough J, Clarke I, Curry A, O'Brien S, Quigley K, Sellwood J, Westmoreland D (2000). "Management of hospital outbreaks of gastro-enteritis due to small roundstructured viruses". J. Hosp. Infect. 45 (1): 1–10. doi:10.1053/jhin.2000.0662. PMID 10833336. http://linkinghub.elsevier.com/retrieve/pii/jhin.2000.0662.
- ↑ http://www.ligocyte.com/downloads/Noro.pdf norovirus candidate vaccine from Ligocyte
- ↑ Bucardo F, Nordgren J, Carlsson B, Paniagua M, Lindgren PE, Espinoza F, Svensson L., "Pediatric norovirus diarrhea in Nicaragua", J. Clin. Microbiology, 46: 8 (August 2008), pp. 2573–80.
- ↑ Shieh Y, Monroe SS, Fankhauser RL, Langlois GW, Burkhardt W, Baric RS (2000). "Detection of norwalk-like virus in shellfish implicated in illness". J. Infect. Dis. 181 Suppl 2: S360–6. doi:10.1086/315578. PMID 10804149. http://www.journals.uchicago.edu/cgi-bin/resolve?JID990682.
- ↑ 27.0 27.1 Department of Health and Ageing Norovirus laboratory case definition
- ↑ Schuffenecker I, Ando T, Thouvenot D, Lina B, Aymard M (2001). "Genetic classification of "Sapporo-like viruses"". Arch. Virol. 146 (11): 2115–32. doi:10.1007/s007050170024. PMID 11765915. http://link.springer.de/link/service/journals/00705/bibs/1146011/11462115.htm. Retrieved 2009-03-01.
- ↑ Ramirez S, Giammanco GM, De Grazia S, Colomba C, Martella V, Arista S (2008). "Genotyping of GII.4 and GIIb norovirus RT-PCR amplicons by RFLP analysis". J. Virol. Methods 147 (2): 250–6. doi:10.1016/j.jviromet.2007.09.005. PMID 17953996. http://linkinghub.elsevier.com/retrieve/pii/S0166-0934(07)00362-X.
- ↑ Vinjé J, Green J, Lewis DC, Gallimore CI, Brown DW, Koopmans MP (2000). "Genetic polymorphism across regions of the three open reading frames of "Norwalk-like viruses"". Arch. Virol. 145 (2): 223–41. doi:10.1007/s007050050020. PMID 10752550. http://link.springer.de/link/service/journals/00705/bibs/0145002/01450223.htm.
- ↑ Tu ET, Bull RA, Greening GE, Hewitt J, Lyon MJ, Marshall JA, McIver CJ, Rawlinson WD, White PA (2008). "Epidemics of gastroenteritis during 2006 were associated with the spread of norovirus GII.4 variants 2006a and 2006b" (– Scholar search). Clin. Infect. Dis. 46 (3): 413–20. doi:10.1086/525259. PMID 18177226. http://bjr.birjournals.org/cgi/pmidlookup?view=long&pmid=18177226.
- ↑ Huang P, Farkas T, Marionneau S, Zhong W, Ruvoën-Clouet N, Morrow AL, Altaye M, Pickering LK, Newburg DS, LePendu J, Jiang X (2003). "Noroviruses bind to human ABO, Lewis, and secretor histo-blood group antigens: identification of 4 distinct strain-specific patterns". J. Infect. Dis. 188 (1): 19–31. doi:10.1086/375742. PMID 12825167. http://www.journals.uchicago.edu/cgi-bin/resolve?JID30248.
- ↑ Huang P, Farkas T, Zhong W, Tan M, Thornton S, Morrow AL, Jiang X (2005). "Norovirus and histo-blood group antigens: demonstration of a wide spectrum of strain specificities and classification of two major binding groups among multiple binding patterns". J. Virol. 79 (11): 6714–22. doi:10.1128/JVI.79.11.6714-6722.2005. PMID 15890909. PMC 1112114. http://jvi.asm.org/cgi/pmidlookup?view=long&pmid=15890909.
- ↑ Rockx BH, Vennema H, Hoebe CJ, Duizer E, Koopmans MP (2005). "Association of histo-blood group antigens and susceptibility to norovirus infections". J. Infect. Dis. 191 (5): 749–54. doi:10.1086/427779. PMID 15688291. http://www.journals.uchicago.edu/cgi-bin/resolve?JID33169.
- ↑ McCartney SA, Thackray LB, Gitlin L, Gilfillan S, Virgin Iv HW, Colonna M (July 18, 2008). "MDA-5 recognition of a murine norovirus.". PLoS Pathog 4 (7): e1000108. doi:10.1371/journal.ppat.1000108. PMID 18636103.
- ↑ Researchers Discover Primary Sensor That Detects Stomach Viruses Newswise, Retrieved on July 20, 2008.
- ↑ Clarke IN, Lambden PR (2000). "Organization and expression of calicivirus genes". J. Infect. Dis. 181 Suppl 2: S309–16. doi:10.1086/315575. PMID 10804143. http://www.journals.uchicago.edu/cgi-bin/resolve?JID990679.
- ↑ Prasad BV, Crawford S, Lawton JA, Pesavento J, Hardy M, Estes MK (2001). "Structural studies on gastroenteritis viruses". Novartis Found. Symp. 238: 26–37; discussion 37–46. doi:10.1002/0470846534.ch3. PMID 11444031.
External links
- NHS Choices Health A-Z Norovirus infections
- CDC Viral Gastroenteritis FAQs: Center for Disease Control and Prevention of Food Illness Fact Sheet
- "Norovirus in Healthcare Facilities Fact Sheet", CDC, released December 21, 2006
- tips from CDC for cruise vacationers
- Winter Vomiting Disease – UK government factsheet
- Viralzone: Norovirus
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||