Mycobacterium
| Mycobacterium | |
|---|---|
 |
|
| TEM micrograph of M. tuberculosis. | |
| Scientific classification | |
| Kingdom: | Bacteria |
| Phylum: | Actinobacteria |
| Order: | Actinomycetales |
| Suborder: | Corynebacterineae |
| Family: | Mycobacteriaceae |
| Genus: | Mycobacterium Lehmann & Neumann 1896 |
| Species | |
|
See below. |
|
Mycobacterium is a genus of Actinobacteria, given its own family, the Mycobacteriaceae. The genus includes pathogens known to cause serious diseases in mammals, including tuberculosis and leprosy.[1] The Latin prefix "myco—" means both fungus and wax; its use here could be related to the "waxy" compounds that compose parts of the cell wall (see Discussion for details)'.
|
Microbiologic characteristics

Mycobacteria are aerobic and nonmotile bacteria (except for the species Mycobacterium marinum, which has been shown to be motile within macrophages) that are characteristically acid-alcohol fast.[1] Mycobacteria do not contain endospores or capsules and are usually considered Gram-positive. A recent paper in PNAS showed sporulation in Mycobacterium marinum and perhaps in M. bovis [2]. However, this has been strongly argued by other scientists [3]. While mycobacteria do not seem to fit the Gram-positive category from an empirical standpoint (i.e. they generally do not retain the crystal violet stain well), they are classified as an acid-fast Gram-positive bacterium due to their lack of an outer cell membrane. All Mycobacterium species share a characteristic cell wall, thicker than in many other bacteria, which is hydrophobic, waxy, and rich in mycolic acids/mycolates. The cell wall consists of the hydrophobic mycolate layer and a peptidoglycan layer held together by a polysaccharide, arabinogalactan. The cell wall makes a substantial contribution to the hardiness of this genus. The biosynthetic pathways of cell wall components are potential targets for new drugs for tuberculosis.[4]
Many Mycobacterium species adapt readily to growth on very simple substrates, using ammonia or amino acids as nitrogen sources and glycerol as a carbon source in the presence of mineral salts. Optimum growth temperatures vary widely according to the species and range from 25 °C to over 50 °C.
Some species can be very difficult to culture (i.e. they are fastidious), sometimes taking over two years to develop in culture. Further, some species also have extremely long reproductive cycles — M. leprae, may take more than 20 days to proceed through one division cycle (for comparison, some E. coli strains take only 20 minutes), making laboratory culture a slow process.[1] In addition, the availability of genetic manipulation techniques still lags far behind that of other bacterial species.[5]
A natural division occurs between slowly– and rapidly–growing species. Mycobacteria that form colonies clearly visible to the naked eye within seven days on subculture are termed rapid growers, while those requiring longer periods are termed slow growers. Mycobacteria cells are straight or slightly curved rods between 0.2-0.6 µm wide by 1.0-10 µm long.
Pigmentation
Some mycobacteria produce carotenoid pigments without light. Others require photoactivation for pigment production.
- Photochromogens (Group I)
- Produce nonpigmented colonies when grown in the dark and pigmented colonies only after exposure to light and reincubation.
- Ex: M. kansasii, M. marinum, M. simiae.
- Scotochromogens (Group II)
- Produce deep yellow to orange colonies when grown in the presence of either the light or dark.
- Ex: M. scrofulaceum, M. gordonae, M. xenopi, M. szulgai.
- Non-chromogens (Groups III & IV)
- Nonpigmented in the light and dark or have only a pale yellow, buff or tan pigment that does not intensify after light exposure.
- Ex: M. tuberculosis, M. avium-intra-cellulare, M. bovis, M. ulcerans
- Ex: M. fortuitum, M. chelonae
Staining characteristics
Mycobacteria are classical acid-fast organisms.[6] Stains used in evaluation of tissue specimens or microbiological specimens include Fite's stain, Ziehl-Neelsen stain, and Kinyoun stain.
Mycobacteria appear phenotypically most closely related to members of Nocardia, Rhodococcus and Corynebacterium.
Ecological characteristics
Mycobacteria are widespread organisms, typically living in water (including tap water treated with chlorine) and food sources. Some, however, including the tuberculosis and the leprosy organisms, appear to be obligate parasites and are not found as free-living members of the genus.
Pathogenicity
Mycobacteria can colonize their hosts without the hosts showing any adverse signs. For example, billions of people around the world have asymptomatic infections of M. tuberculosis.
Mycobacterial infections are notoriously difficult to treat. The organisms are hardy due to their cell wall, which is neither truly Gram negative nor positive. Additionally, they are naturally resistant to a number of antibiotics that disrupt cell-wall biosynthesis, such as penicillin. Due to their unique cell wall, they can survive long exposure to acids, alkalis, detergents, oxidative bursts, lysis by complement, and many antibiotics. Most mycobacteria are susceptible to the antibiotics clarithromycin and rifamycin, but antibiotic-resistant strains have emerged.
As with other bacterial pathogens, surface and secreted proteins of M. tuberculosis contribute significantly to the virulence of this organism. There is an increasing list of extracytoplasmic proteins proven to have a function in the virulence of M. tuberculosis.[7]
Medical classification
Mycobacteria can be classified into several major groups for purpose of diagnosis and treatment: M. tuberculosis complex, which can cause tuberculosis: M. tuberculosis, M. bovis, M. africanum, and M. microti; M. leprae, which causes Hansen's disease or leprosy; Nontuberculous mycobacteria (NTM) are all the other mycobacteria, which can cause pulmonary disease resembling tuberculosis, lymphadenitis, skin disease, or disseminated disease.
Phenotypic testing
Various phenotypic tests can be used to identify and distinguish different Mycobacteria species and strains.
Phenotypic testing of Mycobacteria
Mycosides
Mycosides are phenolic alcohols (such as phenolphthiocerol) that were shown to be components of mycobacterium glycolipids that are termed glycosides of phenolphthiocerol dimycocerosate (Smith DW et al., Nature 1960, 186, 887) There are 18 and 20 carbon atoms in mycosides A, and B, respectively.[8]
Species
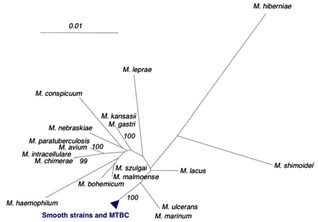
In older systems, mycobacteria are grouped based upon their appearance and rate of growth. However, these are symplesiomorphies, and more recent classification is based upon cladistics.
Slowly growing
Mycobacterium tuberculosis complex
- Mycobacterium tuberculosis complex (MTBC) members are causative agents of human and animal tuberculosis. Species in this complex include:
- M. tuberculosis, the major cause of human tuberculosis
- M. bovis
- M. bovis BCG
- M. africanum
- M. canetti
- M. caprae
- M. microti
- M. pinnipedii
Mycobacterium avium complex
- Mycobacterium avium complex (MAC), is a group of species that, in a disseminated infection but not lung infection, used to be a significant cause of death in AIDS patients. Species in this complex include:
- M. avium
- M. avium paratuberculosis, which has been implicated in Crohn's disease in humans and Johne's disease in cattle and sheep
- M. avium silvaticum
- M. avium "hominissuis"
- M. colombiense
Mycobacterium gordonae clade
- M. asiaticum
- M. gordonae
Mycobacterium kansasii clade
- M. gastri
- M. kansasii
Mycobacterium nonchromogenicum/terrae clade
- M. hiberniae
- M. nonchromogenicum
- M. terrae
- M. triviale
Mycolactone-producing mycobacteria
- M. ulcerans, which causes the "Buruli", or "Bairnsdale, ulcer"
- M. pseudoshottsii
- M. shottsii
Mycobacterium simiae clade
- M. triplex
- M. genavense
- M. florentinum
- M. lentiflavum
- M. palustre
- M. kubicae
- M. parascrofulaceum
- M. heidelbergense
- M. interjectum
- M. simiae
Ungrouped
- M. branderi
- M. cookii
- M. celatum
- M. bohemicum
- M. haemophilum
- M. malmoense
- M. szulgai
- M. leprae, which causes leprosy
- M. lepraemurium
- M. lepromatosis, another (less significant) cause of leprosy, described in 2008
- M. africanum
- M. botniense
- M. chimaera
- M. conspicuum
- M. doricum
- M. farcinogenes
- M. heckeshornense
- M. intracellulare
- M. lacus
- M. marinum
- M. monacense
- M. montefiorense
- M. murale
- M. nebraskense
- M. saskatchewanense
- M. scrofulaceum
- M. shimoidei
- M. tusciae
- M. xenopi
Intermediate growth rate
- M. intermedium
Rapidly growing
Mycobacterium chelonae clade
- M. abscessus
- M. chelonae
- M. bolletii
Mycobacterium fortuitum clade
- M. fortuitum
- M. fortuitum subsp. acetamidolyticum
- M. boenickei
- M. peregrinum
- M. porcinum
- M. senegalense
- M. septicum
- M. neworleansense
- M. houstonense
- M. mucogenicum
- M. mageritense
- M. brisbanense
- M. cosmeticum
Mycobacterium parafortuitum clade
- M. parafortuitum
- M. austroafricanum
- M. diernhoferi
- M. hodleri
- M. neoaurum
- M. frederiksbergense
Mycobacterium vaccae clade
- M. aurum
- M. vaccae
CF
- M. chitae
- M. fallax
Ungrouped
- M. confluentis
- M. flavescens
- M. madagascariense
- M. phlei
- M. smegmatis
- M. goodii
- M. wolinskyi
- M. thermoresistibile
- M. gadium
- M. komossense
- M. obuense
- M. sphagni
- M. agri
- M. aichiense
- M. alvei
- M. arupense
- M. brumae
- M. canariasense
- M. chubuense
- M. conceptionense
- M. duvalii
- M. elephantis
- M. gilvum
- M. hassiacum
- M. holsaticum
- M. immunogenum
- M. massiliense
- M. moriokaense
- M. psychrotolerans
- M. pyrenivorans
- M. vanbaalenii
- M. pulveris
Ungrouped
- M. arosiense
- M. aubagnense
- M. caprae
- M. chlorophenolicum
- M. fluoroanthenivorans
- M. kumamotonense
- M. novocastrense
- M. parmense
- M. phocaicum
- M. poriferae
- M. rhodesiae
- M. seoulense
- M. tokaiense
References
- ↑ 1.0 1.1 1.2 Ryan KJ, Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. ISBN 0-8385-8529-9.
- ↑ Ghosh, Jaydip, Pontus Larsson, Bhupender Singh, B M Fredrik Pettersson, Nurul M Islam, Sailendra Nath Sarkar, Santanu Dasgupta, y Leif A Kirsebom. 2009. Sporulation in mycobacteria. Proceedings of the National Academy of Sciences of the United States of America 106, no. 26 (Junio 30): 10781-10786. http://www.ncbi.nlm.nih.gov/pubmed/19541637
- ↑ Traag BA, Driks A, Stragier P, Bitter W, Broussard G, Hatfull G, Chu F, Adams KN, Ramakrishnan L, Losick R.2010. Do mycobacteria produce endospores? Proc Natl Acad Sci U S A. 2010 Jan 12;107(2):878-81.
- ↑ Bhamidi S (2009). "Mycobacterial Cell Wall Arabinogalactan". Bacterial Polysaccharides: Current Innovations and Future Trends. Caister Academic Press. ISBN 978-1-904455-45-5.
- ↑ Parish T, Brown A (editors) (2009). Mycobacterium: Genomics and Molecular Biology. Caister Academic Press. ISBN 978-1-904455-40-0.
- ↑ McMurray DN (1996). "Mycobacteria and Nocardia". In Baron S et al. (eds.). Baron's Medical Microbiology (4th ed.). Univ of Texas Medical Branch. ISBN 0-9631172-1-1. http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=mmed.section.1772.
- ↑ McCann et al. (2009). "Secreted and Exported Proteins Important to Mycobacterium tuberculosis Pathogenesis". Bacterial Secreted Proteins: Secretory Mechanisms and Role in Pathogenesis. Caister Academic Press. ISBN 978-1-904455-42-4.
- ↑ fatty alcohols and aldehydes
Further reading
- Diagnosis and Treatment of Disease Caused by Nontuberculous Mycobacteria (PDF). American Thoracic Society. Am J Respiratory and Critical Care Medicine. Aug 1997 156(2) Part 2 Supplement
- RIDOM: Ribosomal Differentiation of Medical Microorganisms
- J.P. Euzéby: List of Prokaryotic Names with Standing in Nomenclature - Genus Mycobacterium
External links
- Tuberculist: Genome annotation database
- MTB Sysborg: Genome annotation database from the Institute of Genomics and Integrative Biology
- TB Structural Genomics Consortium: Structures of Mycobacterium tuberculosis proteins
- MycDB: Mycobacterium database
- TBDB: Tuberculosis database
- Mycobacterium genomes and related information at PATRIC, a Bioinformatics Resource Center funded by NIAID
- Frequently Asked Questions about NTM Lung Disease
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||