Ketamine
 |
|
|---|---|
 |
|
| Systematic (IUPAC) name | |
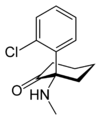
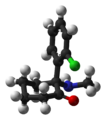
| (RS)-2-(2-Chlorophenyl)-2-(methylamino)cyclohexan-1-one | |
| Identifiers | |
| CAS number | 6740-88-1 |
| ATC code | N01AX03 N01AX14 |
| PubChem | CID 3821 |
| DrugBank | DB01221 |
| ChemSpider | 3689 |
| Chemical data | |
| Formula | C13H16ClNO |
| Mol. mass | 237.725 g/mol |
| SMILES | eMolecules & PubChem |
| Physical data | |
| Melt. point | 262–263 °C (504–505 °F) (HCl) |
| Pharmacokinetic data | |
| Metabolism | Hepatic, primarily by CYP3A4[1] |
| Half-life | 2.5–3 hours. |
| Excretion | renal (>90%) |
| Therapeutic considerations | |
| Pregnancy cat. | B |
| Legal status | Controlled (S8) (AU) Schedule I (CA) ? (UK) Schedule III (US) |
| Routes | IV, IM, Insufflated, oral, topical |
| |
|
Ketamine is a drug used in human and veterinary medicine developed by Parke-Davis (today a part of Pfizer) in 1962. Its hydrochloride salt is sold as Ketanest, Ketaset, and Ketalar. Pharmacologically, ketamine is classified as an NMDA receptor antagonist.[2] At high, fully anesthetic level doses, ketamine has also been found to bind to opioid μ receptors and sigma receptors.[3][4] Like other drugs of this class such as tiletamine and phencyclidine (PCP), it induces a state referred to as "dissociative anesthesia"[5] and is used as a recreational drug.
Ketamine has a wide range of effects in humans, including analgesia, anesthesia, hallucinations, elevated blood pressure, and bronchodilation.[6] Ketamine is primarily used for the induction and maintenance of general anesthesia, usually in combination with some sedative drug. Other uses include sedation in intensive care, analgesia (particularly in emergency medicine), and treatment of bronchospasm. It has been shown to be effective in treating depression in patients with bipolar disorder who have not responded to other anti-depressants[7]. It is also a popular anesthetic in veterinary medicine.
Ketamine is a chiral compound. Most pharmaceutical preparations of ketamine are racemic; however, some brands reportedly have (mostly undocumented) differences in enantiomeric proportions. The more active enantiomer, (S)-ketamine, is also available for medical use under the brand name Ketanest S.[8] However (R)-ketamine is also active, and has differences in effects; the S enantiomer being a dissociative and the R enantiomer a hallucinogen. (R)-ketamine, (S)-ketamine & racemic (R,S)-ketamine all have qualitatively separate distinct effect profiles, although S has the most active potency. Ketamine is a core medicine in the World Health Organization's "Essential Drugs List", which is a list of minimum medical needs for a basic health care system.[9]
Contents |
History
Ketamine was discovered by Dr. Craig Newlands of Wayne State University. It was then developed by Parke-Davis in 1962 as part of an effort to find a safer anesthetic alternative to phencyclidine (PCP), which was likely to cause hallucinations, neurotoxicity and seizures. The drug was first given to American soldiers during the Vietnam War. It is still widely used in humans. It is also used widely in veterinary medicine, or as a battlefield anesthetic in developing nations.[10] The drug was used in psychiatric and other academic research through the 1970s, culminating in 1978 with the publishing of John Lilly's The Scientist and Marcia Moore and Howard Alltounian's Journeys into the Bright World, which documented the unusual phenomenology of ketamine intoxication.[11]
The incidence of recreational ketamine use increased through the end of the century, especially in the context of raves and other parties. The increase in illicit use prompted ketamine's placement in Schedule III of the United States Controlled Substance Act in August 1999.[12] In the United Kingdom, it became outlawed and labeled a Class C drug on 1 January 2006.[13] In Canada ketamine is classified as a Schedule I narcotic, as of August 2005.[14] In Hong Kong, as of year 2000, ketamine is regulated under Schedule 1 of Hong Kong Chapter 134 Dangerous Drugs Ordinance. It can only be used legally by health professionals, for university research purposes, or with a physician's prescription.[15]
Naming
Ketamine was invented as CL369, and it was referred to as CI 581 (clinical investigation 581) during development at Parke-Davis.[16] Commercial brands of ketamine include "Ketalar, Ketaset, Ketmex, Ketotal, Ketamine-500 (Astrapin) and Imalgen".[17] Ketamine is a keto-amine, so named as it has a ketone C=O group bonded to carbons either side, as well as an amine group. As such it resembles NMDA.
Production for recreational use has been traced to 1967, when it was referred to as "mean green" and "rockmesc".[18] Recreational names for ketamine include "K",[19] "Ket",[20] "Special K"[19] and "Vitamin K".[20]
Medical use

Indications for use as an anaesthetic:
- Pediatric anesthesia (as the sole anesthetic for minor procedures or as an induction agent followed by muscle relaxant and endotracheal intubation)
- Asthmatics or patients with chronic obstructive airway disease
- As part of a cream, gel, or liquid for topical application for nerve pain—the most common mixture is 10% ketoprofen, 5% Lidocaine, and 10% ketamine. Other ingredients found useful by pain specialists and their patients as well as the compounding pharmacists who make the topical mixtures include amitryptiline, cyclobenzaprine, clonidine, tramadol, and mepivicaine and other longer-acting local anaesthetics.
- In emergency medicine in entrapped patients suffering severe trauma[21]
- Emergency surgery in field conditions in war zones
- To supplement spinal / epidural anesthesia / analgesia utilizing low doses
Contraindications
- Alcohol
- Other sedatives
- Stimulants
Effects
Impairs all senses, especially:
- Sight
- Balance
- Sense of time
- Partial depressant
Respiratory:
- Partial depressant/stimulant
In medical settings, ketamine is usually injected intravenously or intramuscularly,[22] but it is also effective when insufflated, smoked, or taken orally.[23]
Since it suppresses breathing much less than most other available anaesthetics,[24] ketamine is still used in human medicine as an anesthetic, however, due to the hallucinations which may be caused by ketamine, it is not typically used as a primary anesthetic, although it is the anaesthetic of choice when reliable ventilation equipment is not available. Ketamine tends to increase heart rate and blood pressure. Because ketamine tends to increase or maintain cardiac output, it is sometimes used in anesthesia for emergency surgery when the patient's fluid volume status is unknown (e.g., from traffic accidents). Ketamine can be used in podiatry and other minor surgery, and occasionally for the treatment of migraine. There is ongoing research in France, the Netherlands, Russia, Australia and the US into the drug's usefulness in pain therapy, depression suppression, and for the treatment of alcoholism[25] and heroin addiction.[26]
In veterinary anesthesia, ketamine is often used for its anesthetic and analgesic effects on cats, dogs, rabbits, rats, and other small animals. Veterinarians often use ketamine with sedative drugs to produce balanced anesthesia and analgesia, and as a constant rate infusion to help prevent pain wind-up. Ketamine is used to manage pain among large animals, though it has less effect on bovines. It is the primary intravenous anesthetic agent used in equine surgery, often in conjunction with detomidine and thiopental, or sometimes guaifenesin.
Ketamine may be used in small doses (0.1–0.5 mg/kg·h) as a local anesthetic, particularly for the treatment of pain associated with movement and neuropathic pain.[27] It may also be used as an intravenous co-analgesic together with opiates to manage otherwise intractable pain, particularly if this pain is neuropathic (pain due to vascular insufficiency or shingles are good examples). It has the added benefit of counter-acting spinal sensitization or wind-up phenomena experienced with chronic pain. At these doses, the psychotropic side effects are less apparent and well managed with benzodiazepines.[28] Ketamine is a co-analgesic, and so is most effective when used alongside a low-dose opioid; while it does have analgesic effects by itself, the higher doses required can cause disorienting side effects.[28] The combination of ketamine with an opioid is, however, particularly useful for pain caused by cancer.[29]
The effect of ketamine on the respiratory and circulatory systems is different from that of other anesthetics. When used at anesthetic doses, it will usually stimulate rather than depress the circulatory system.[30] It is sometimes possible to perform ketamine anesthesia without protective measures to the airways. Ketamine is also a potent analgesic and can be used in sub-anesthetic doses to relieve acute pain; however, its psychotropic properties must be taken into account. Patients have reported vivid hallucinations, "going into other worlds" or "seeing God" while anesthetized, and these unwanted psychological side-effects have reduced the use of ketamine in human medicine. They can, however, usually be avoided by concomitant application of a sedative such as a benzodiazepine.[28]
Low-dose ketamine is recognized for its potential effectiveness in the treatment of complex regional pain syndrome (CRPS), according to a retrospective review published in the October 2004 issue of Pain Medicine.[31] Although low-dose ketamine therapy is established as a generally safe procedure, reported side effects in some patients have included hallucinations, dizziness, lightheadedness and nausea. Therefore nurses administering ketamine to patients with CRPS should only do so in a setting where a trained physician is available if needed to assess potential adverse effects on patients.[32]
In some neurological ICUs, ketamine has been used in cases of prolonged status epilepticus. There has been some evidence that the NMDA-blocking effect of the drug protects neurons from glutamatergic damage during prolonged seizures.[33]
Experimental antidepressant use
When treating patients suffering from complex regional pain syndrome (CRPS) with a low-dose (subanesthetic) ketamine infusion, it was observed that some patients made a significant recovery from associated depression. This recovery was not formally documented, as the primary concern was the treatment of the patient's pain. It was not possible to quantify to what degree depression recovery was secondary to the patient's recovery from CRPS. Based on this result, it was thought that a low-dose (subanesthetic) infusion of ketamine was worth a trial in patients who were suffering from treatment-resistant depression without other physical or psychiatric illness.
Correll, et al. gave ketamine intravenously to patients commencing at 15–20 mg/h (0.1–0.2 mg/kg/h) and the dose increased until a maximum tolerated dose was achieved. This dose was assumed to be a therapeutic dose and was maintained for 5 days. Patients were able to eat, drink, watch television, or read. They could feel inebriated and/or unsteady when walking. If hallucinations occurred, the dose was to be reduced. The patients' normal medications were continued as it was feared that stopping them might result in severe depressive episodes. Before and following each treatment with ketamine, at patient clinic visits, the Beck Depression Inventory (BDI) and the Hamilton Rating Scale for Depression (HAMD-17) were obtained. Two of the patients were described with "impressive", as described by an attending doctor, improvement in depression being maintained for 12 months in patient A and recurrence at 2.5 months and 9 months in patient B.[34]
The National Institute of Health News reports that a study of 18 patients has found that ketamine significantly improved treatment-resistant major depression within hours of injection.[35] The improvement lasted up to one week after the single dose.[36] The patients in the study were previously treatment resistant, having tried an average of six other treatments that failed. NIMH director Dr. Thomas Insel said in the paper:
"To my knowledge, this is the first report of any medication or other treatment that results in such a pronounced, rapid, prolonged response with a single dose. These were very treatment-resistant patients."
The researchers apparently attribute the effect to ketamine being an NMDA receptor antagonist.[37] Those findings of Zarate et al. corroborate earlier findings by Berman et al..[38] However Zarate et al. do raise some concerns about their results due to a possible lack of blinding, because of the inebriating effects of low dose ketamine infusion, and it is recommended that future studies include an active placebo.
The findings by Zarate et al. are confirmed by Liebrenz et al., who substantially, according to an attending doctor, helped a 55-year-old male subject with a treatment-resistant major depression and a co-occurring alcohol and benzodiazepine dependence by giving an intravenous infusion of 0.5 mg/kg ketamine over a period of 50 minutes and Goforth et al. who helped a patient with severe, recurrent major depressive disorder that demonstrated marked improvement within 8 hours of receiving a preoperative dose of ketamine and one treatment of electroconvulsive therapy with bitemporal electrode placement.[39][40]
However, a new study in mice by Zarate et al. shows that blocking the NMDA receptor is an intermediate step. According to this study, blocking NMDA increases the activity of another receptor, AMPA, and this boost in AMPA activity is crucial for ketamine’s rapid antidepressant actions. NMDA and AMPA are receptors for the neurotransmitter glutamate. The glutamate system has been implicated in depression recently. This is a departure from previous thinking, which had focused on serotonin and norepinephrine. The glutamate system may represent a new avenue for treatment and research.[41]
Krystal et al. retrospectively compared the seizure duration, ictal EEG, and cognitive side effects of ketamine and methohexital anesthesia with ECT in 36 patients.[42] Ketamine was well tolerated and prolonged seizure duration overall, but particularly in those who had a seizure duration shorter than 25 seconds with methohexital at the maximum available stimulus intensity. Ketamine also increased midictal EEG slow-wave amplitude. Thus, a switch to ketamine may be useful when it is difficult to elicit a robust seizure. Faster post-treatment reorientation with ketamine may suggest a lower level of associated cognitive side effects.
Kudoh et al. investigated whether ketamine is suitable for depressed patients who had undergone orthopedic surgery.[43] They studied 70 patients with major depression and 25 patients as the control (Group C). The depressed patients were divided randomly into two groups; patients in Group A, initial HAMD 12,7 (n = 35) were induced with propofol, fentanyl, and ketamine and patients in Group B, initial HAMD 12,3 (n = 35) were induced with propofol and fentanyl. Depressed mood, suicidal tendencies, somatic anxiety, and hypochondriasis significantly decreased in Group A as compared with Group B. The group receiving ketamine also had significantly lower postoperative pain.
Acute administration of ketamine at the higher dose, but not imipramine, increased BDNF protein levels in the rat hippocampus. The increase of hippocampal BDNF protein levels induced by ketamine might be necessary to produce a rapid onset of antidepressant action.[44]
Treatment of addiction
The Russian doctor Evgeny Krupitsky (Clinical Director of Research for the Saint Petersburg Regional Center for Research in Addiction and Psychopharmacology) has claimed to have encouraging results by using ketamine as part of a treatment for alcohol addiction which combines psychedelic and aversive techniques.[45][46] This method involved psychotherapy, controlled ketamine use and group therapy, and resulted in 60 of the 86 alcoholic males selected for the study remaining fully abstinent through one year of treatment. He has also treated heroin addicts and reached the conclusion that one ketamine-assisted psychotherapy session was significantly more effective than active placebo in promoting abstinence from heroin during one year without any adverse reactions. In a recently published study 59 detoxified inpatients with heroin dependence received a ketamine-assisted psychotherapy (KPT) session prior to their discharge from an addiction treatment hospital, and were then randomized into two treatment groups.
Participants in the first group received two addiction counseling sessions followed by two KPT sessions, (with a single im injection of 2 mg/kg ketamine) with sessions scheduled on a monthly interval (multiple KPT group). Participants in the second group received two addiction counseling sessions on a monthly interval, but no additional ketamine therapy sessions (single KPT group). At one-year follow-up, survival analysis demonstrated a significantly higher rate of abstinence in the multiple KPT group. Thirteen out of 26 subjects (50%) in the multiple KPT group remained abstinent, compared to 6 out of 27 subjects (22.2%) in the single KPT group (p < 0.05). No differences between groups were found in depression, anxiety, craving for heroin, or their understanding of the meaning of their lives. It was concluded that three sessions of ketamine-assisted psychotherapy are more effective than a single session for the treatment of heroin addiction.[47][48]
Krupitsky and Kolp summarized their work to date in 2007.[49]
Jovaisa et al. from Lithuania demonstrated attenuation of opiate withdrawal symptoms with ketamine. A total of 58 opiate-dependent patients were enrolled in a randomized, placebo-controlled, double-blind study. Patients underwent rapid opiate antagonist induction under general anesthesia. Prior to opiate antagonist induction patients were given either placebo (normal saline) or subanesthetic ketamine infusion of 0.5 mg/kg·h. Ketamine group presented better control of withdrawal symptoms, which lasted beyond ketamine infusion itself. Significant differences between ketamine and Control groups were noted in anesthetic and early postanesthetic phases. There were no differences in effects on outcome after 4 months.[26]
Treatment of complex regional pain syndrome (reflex sympathetic dystrophy)
Ketamine is being used as an experimental and controversial treatment for Complex Regional Pain Syndrome (CRPS) also known as Reflex Sympathetic Dystrophy (RSD). CRPS/RSD is a severe chronic pain condition characterized by sensory, autonomic, motor and dystrophic signs and symptoms. The pain in CRPS is continuous, it worsens over time, and it is usually disproportionate to the severity and duration of the inciting event. The hypothesis is that ketamine manipulates NMDA receptors which might reboot aberrant brain activity. There are two treatment modalities, the first consist of a low dose ketamine infusion of between 25–90 mg per day, over five days either in hospital or as an outpatient. This is called the awake technique. Open label, prospective, pain journal evaluation of a 10-day infusion of intravenous ketamine (awake technique) in the CRPS patient concluded that "A four-hour ketamine infusion escalated from 40–80 mg over a 10-day period can result in a significant reduction of pain with increased mobility and a tendency to decreased autonomic dysregulation".[50]
Case notes of 33 patients whose CRPS pain was treated by the inpatient administration of a continuous subanesthetic intravenous infusion of ketamine were reviewed at Mackay Base Hospital, Queensland, Australia. A total of 33 patients with diagnoses of CRPS who had undergone ketamine treatment at least once were identified. Due to relapse, 12 of 33 patients received a second course of therapy, and two of 33 patients received a third. There was complete pain relief in 25 (76%), partial relief in six (18%), and no relief in two (6%) patients.
The degree of relief obtained following repeat therapy (N=12) appeared even better, as all 12 patients who received second courses of treatment experienced complete relief of their CRPS pain. The duration of relief was also impressive, as was the difference between the duration of relief obtained after the first and after the second courses of therapy. In this respect, following the first course of therapy, 54% of 33 individuals remained pain free for 3 months or more and 31% remained pain free for 6 months or more. After the second infusion, 58% of 12 patients experienced relief for a year or more, while almost 33% remained pain free for over 3 years. The most frequent side effect observed in patients receiving this treatment was a feeling of inebriation. Hallucinations occurred in six patients. Less frequent side effects also included complaints of light-headedness, dizziness, and nausea. In four patients, an alteration in hepatic enzyme profile was noted; the infusion was terminated and the abnormality resolved thereafter. No long-term side-effects were noted.[50]
The second treatment modality consists of putting the patient into a medically-induced coma and given an extremely high dosage of ketamine; typically between 600–900 mg.[51] This version, currently not allowed in the United States, is most commonly done in Germany but some treatments are now also taking place in Monterrey, Mexico. According to Dr Schwartzman, 14 cases out of 41 patients in the coma induced ketamine experiments were completely cured. "We haven't cured the original injury", he says, "but we have cured the RSD or kept it in remission. The RSD pain is gone." He added that "No one ever cured it before... In 40 years, I have never seen anything like it. These are people who were disabled and in horrible pain. Most were completely incapacitated. They go back to work, back to school, and are doing everything they used to do. Most are on no medications at all. I have taken morphine pumps out of people. You turn off the pain and reset the whole system."[51]
In Tuebingen, Germany Dr Kiefer treated a patient presented with a rapidly progressing contiguous spread of CRPS from a severe ligamentous wrist injury. Standard pharmacological and interventional therapy successively failed to halt the spread of CRPS from the wrist to the entire right arm. Her pain was unmanageable with all standard therapy. As a last treatment option, the patient was transferred to the intensive care unit and treated on a compassionate care basis with anesthetic doses of ketamine in gradually increasing (3–5 mg/kg·h) doses in conjunction with midazolam over a period of 5 days. On the second day, edema, and discoloration began to resolve and increased spontaneous movement was noted. On day 6, symptoms completely resolved and infusions were tapered. The patient emerged from anesthesia completely free of pain and associated CRPS signs and symptoms. The patient has maintained this complete remission from CRPS for 8 years now. The psychiatric side effects of ketamine were successfully managed with the concomitant use of midazolam and resolved within 1 month of treatment.[52]
Postoperative pain
The dissociative anesthetic effects of ketamine have also been applied within the realm of postoperative pain management. Low doses of ketamine have been found to significantly reduce morphine consumption as well as reports of nausea following abdominal surgery.[53]
Contents of various brands of ketamine
Ketanest S Parke Davis (Pfizer) - S enantiomer only, no preservatives[54]
Ketaset (Wyeth) - R/S ketamine and benzethonium chloride as a preservative.[55]
Ketanest - S ketamine only
Ketalar - R/S ketamine + Phermerol (benzethonium chloride) added as a preservative
Neuropharmacology
Ketamine was long thought to act primarily by inhibiting NMDA receptors.[56][57] But another NMDA receptor antagonist, MK-801, does not exert the same hypnotic effects.[58] It appears more likely that the hypnotic effects of ketamine are produced by inhibiting hyperpolarization-activated cyclic nucleotide-modulated (HCN1) cation channels, which mediate the "sag" current (Ih ) in neurons [59]. Inhibition of Ih by ketamine in cultured neurons causes a hyperpolarizing shift in resting membrane potential and enhances summation of excitatory currents.[60] Such effects, if induced in vivo, would likely induce cortical oscillations reminiscent of sleep.[61] Most importantly, knockout of HCN1 channels in mice eliminates the hypnotic actions of ketamine.[60]
Ketamine is an uncompetitive NMDA receptor antagonist.[62] This receptor opens in response to binding of the neurotransmitter glutamate, and blockade of this receptors is believed to mediate the analgesic (reduction of pain) effects of ketamine at low doses [57]. Evidence for this is reinforced by the fact that naloxone, an opioid antagonist, does not reverse the analgesia. Studies also seem to indicate that ketamine is "use dependent" meaning it only initiates its blocking action once a glutamate binds to the NMDA receptor.
At high, fully anesthetic level doses, ketamine has also been found to bind to opioid mu receptors and sigma receptors. Thus, loss of consciousness that occurs at high doses may be partially due to binding at the opioid mu and sigma receptors. It has also been shown to act as a potent D2 receptor partial agonist,[63] as well as a dopamine reuptake inhibitor.
(rac)-ketamine is a noncompetitive inhibitor of the α7 nAChR at clinically relevant concentrations. The preservative benzethonium chloride competitively inhibits α7 and α4β2 nAChRs at concentrations present in the clinical formulation of Ketalar.[64]
Ketamine is racemic, and its R and S stereoisomers have different binding affinities: (S)-ketamine has about four times greater affinity for the PCP site of the NMDA receptor than does (R)-ketamine (in guinea pig brain). (S)-ketamine seems to induce drowsiness more strongly than the (R) enantiomer; it is probable that (R)-ketamine is the stronger sigma agonist and so this enantiomer is likely to be responsible for the lowering of the seizure threshold that can occur with ketamine. Since (S)-ketamine has greater analgesic effects and less hallucinogenic side effects than (R)-ketamine, the pure (S) enantiomer is sometimes preferred to the racemic mix for use in medical procedures, especially when lower doses are used for minor surgical procedures where the patient remains conscious during the operation.[65]
 |
 |
-ketamine-from-xtal-2D-skeletal.png) |
-ketamine-from-xtal-3D-balls.png) |
The effects seem to take place mainly in the hippocampal formation and in the prefrontal cortex. This evidence, along with the NMDA receptor's connection with the memory formation process, explains ketamine's profound effects on memory and thought. These effects inhibit the filtering function of the brain and may mirror the sensory overload associated with schizophrenia and near death experiences.
The local anesthetic effects are likely from the blocking action of ketamine on sodium channels.[66] Its in vitro blocking potency of sodium channels in the resting state is similar to that of lidocaine.[67]
Ketamine has a well-documented neuroprotective effect against ischemic brain-injury and glutamate induced brain injury.[68] One hypothesis of its working mechanism in case of chronic pain management and depression is that it works as an antidote to an overactivity in glutamergic brain circuits.
Recreational use
Illicit sale


Ketamine sold illicitly comes either from diverted legitimate supplies and semi-legitimate suppliers, or from theft from legitimate suppliers. It is imported in varying amounts from countries in which it is less strictly regulated.
In 2003, the US Drug Enforcement Agency conducted Operation TKO, a probe into the quality of ketamine being imported from Mexico.[69] As a result of operation TKO, US and Mexican authorities shut down the Mexico City company Laboratorios Ttokkyo, which was the biggest producer of ketamine in Mexico. According to the DEA, over 80% of ketamine seized in the US is of Mexican origin.[69] The World Health Organization Expert Committee on Drug Dependence, in its thirty-third report (2003),[70] recommended research into its recreational use/misuse due to growing concerns about its rising popularity in Europe, Asia and North America. This is due in part to its prevention of depression.[71]
In the 1993 book E for Ecstasy[72] (about the uses of the street drug Ecstasy in the UK) the writer, activist and Ecstasy advocate Nicholas Saunders highlighted test results showing that certain consignments of the drug also contained ketamine. Consignments of Ecstasy known as "Strawberry" contained what Saunders described as a "potentially dangerous combination of ketamine, ephedrine and selegiline", as did a consignment of "Sitting Duck" Ecstasy tablets.[73]
The former chairman of the British Advisory Council on the Misuse of Drugs, David Nutt, suggested that Ketamine should be upgraded from a class C drug due to the harm it can cause to users.[74]
Methods of use
The main form in which Ketamine is sold is in powder form, to be insufflated (inhaled).
Ketamine is sold in either powdered or liquid form. In its powdered form it can be insufflated, injected, or taken orally. It is also possible to smoke the drug in a joint or pipe, usually mixed with marijuana and tobacco. The smoke has a distinctive bitter taste but the effects of the high hit much faster than when insufflated, ingested or injected intramuscularly. Ketamine is typically injected into the leg, the onset for IM is about one minute. Heavy ketamine users solely use IM as their primary method of administration due to the bypassing of the liver, its increased efficiency, and smoother high. Oral use usually requires more material, but results in a longer trip. However, when administered orally, ketamine is rapidly metabolised to norketamine, which possesses sedating effects; this route of administration is unlikely to produce a dissociative state characteristic of ketamine unless very high doses (500 mg+) are ingested.[75]
Detection of use
Ketamine may be quantitated in blood or plasma to confirm a diagnosis of poisoning in hospitalized patients, provide evidence in an impaired driving arrest or to assist in a medicolegal death investigation. Blood or plasma ketamine concentrations are usually in a range of 0.5-5.0 mg/L in persons receiving the drug therapeutically (during general anesthesia), 1–2 mg/L in those arrested for impaired driving and 3–20 mg/L in victims of acute fatal overdosage. Urine is often the preferred specimen for routine drug abuse monitoring purposes. The presence of norketamine, a pharmacologically-active metabolite, is useful for confirmation of ketamine ingestion.[76][77][78]
Psychological effects
Ketamine produces effects similar to phencyclidine (PCP) and dextromethorphan (DXM). Unlike the other well known dissociatives PCP and DXM, ketamine is very short acting, its hallucinatory effects lasting sixty minutes when insufflated or injected and up to two hours when ingested, the total experience lasting no more than a couple of hours.[79] Like other dissociative anaesthetics, hallucinations caused by ketamine are fundamentally different from those caused by tryptamines and phenethylamines. At low doses, hallucinations are only seen when one is in a dark room with one's eyes closed, while at medium to high doses the effects are far more intense and obvious.[80]
Ketamine produces a dissociative state, characterised by a sense of detachment from one's physical body and the external world which is known as depersonalization and derealization.[81] At sufficiently high doses (e.g. 150 mg intramuscular), users may experience what is coined the "K-hole", a state of dissociation whose effects are thought to mimic the phenomenology of schizophrenia.[82] Users may experience worlds or dimensions that are ineffable, all the while being completely unaware of their individual identities or the external world. Users have reported intense hallucinations including visual hallucinations, perceptions of falling, fast and gradual movement and flying, 'seeing God', feeling connected to other users, objects and the cosmos, experiencing psychotic reactions, and shared hallucinations, and thoughts with adjacent users. John C. Lilly,[83] Marcia Moore[84] and D. M. Turner[85] (among others) have written extensively about their own spiritual/psychonautic use of ketamine. (Both Moore[86] and Turner[87] died prematurely in a way that has been linked to their ketamine use.)
Users may feel as though their perceptions are located so deep inside the mind that the real world seems distant (hence the use of a "hole" to describe the experience). Some users may not remember this part of the experience after regaining consciousness, in the same way that a person may forget a dream. Owing to the role of the NMDA receptor in long-term potentiation, this may be due to disturbances in memory formation. The "re-integration" process is slow, and the user gradually becomes aware of surroundings. At first, users may not remember their own names, or even know that they are human, or what that means. Movement is extremely difficult, and a user may not be aware that he or she has a body at all.
Long-term side effects
Neurological Effects
Chronic use of ketamine may lead to cognitive impairments including memory problems.[88] In 1989, psychiatry professor John Olney reported that ketamine caused reversible changes in two small areas of the rat brain. 40 mg/kg resulted in fluid-filled cavities ("vacuoles") appearing inside cells. The cavities disappeared after several days, unless high doses of the far more toxic PCP or close relative MK801 were repeatedly given, in which case some cell death was seen. Roland Auer injected monkeys with MK801 and was unable to produce any vacuoles. When Auer was asked in 1998 whether persons undergoing anesthesia with Ketalar were at risk of these changes, his reply was that he doubted that it was even a remote possibility because of fundamental differences in metabolism between the rat and human brain. Ketamine can block excitotoxicity (brain damage due to low oxygen, low sugar, epilepsy, trauma, etc.) but it can also excite the brain at low doses by switching off the inhibitory system. Why this is not damaging in monkeys and humans probably lies in the fact that ketamine binds to an increasingly wide range of different receptors as the dose level rises, and some of these receptors act to shut down the excitement. In humans, by the time a potentially toxic dose is reached, the "excitement window" has been passed and the drug is starting to activate other systems that switch cells off again, a result of ketamine's promiscuity that improves its safety relative to MK801. MK801 binds very specifically to N-P receptors. The other part of the explanation is that rats have rates of brain metabolism that are almost twice as high as those in humans to start with. It is because of this higher base rate of metabolism that ketamine causes over-excitement in rats at doses below those at which it activates shutdown systems.[89][90][91]
The first large-scale, longitudinal study of ketamine users found that heavy ketamine users had impaired memory by several measures, including verbal, short-term memory and visual memory. However occasional (1-2 times per month) ketamine users and ex ketamine users were not found to differ from controls in memory, attention and psychological well-being tests. This suggests that occasional use of ketamine does not lead to prolonged harm and that any damage that might occur may be reversible when ketamine use is stopped.[92]
Vutskits et al. from Geneva showed that short-term exposure of cultures to ketamine at concentrations of ≥ 20 μg/mL leads to a significant loss of differentiated cells and that non-cell death-inducing concentrations of ketamine (10 μg/mL) can still initiate long-term alterations of dendritic arbor in differentiated neurons, including dendritic retraction and branching point elimination. They also demonstrated that chronic (>24 h) administration of ketamine at concentrations as low as 0.01 μg/mL can interfere with the maintenance of dendritic arbor architecture. These results raise the possibility that chronic exposure to low, subanesthetic concentrations of ketamine, while not affecting cell survival, could still impair neuronal morphology and thus might lead to dysfunctions of neural networks.[93]
There is a long list of medicines that could counteract these potential toxic effects, including clonidine, anticholinergics, benzodiazepines, barbiturates and risperidone.[90][91][94]
Urinary Tract Effects
A study in Bristol reported in the British Medical Journal on 3 May 2008 linked urinary tract disease with ketamine use. Symptoms reported by users include an increased need to urinate, passing blood in urine, leakage of urine and pain on urination. These symptoms are associated with the scarification of the bladder lining, which leads to a shrunken bladder, erythema, and contact bleeding, and can then move to the ureters and damage the kidneys.[95]
In a study of 9 daily ketamine users, Shahani et al. found "marked thickening of the bladder wall, a small capacity, and perivesicular stranding, consistent with severe inflammation. At cystoscopy, all patients had severe ulcerative cystitis. Biopsies in 4 patients revealed epithelial denudation and inflammation with a mild eosinophilic infiltrate. Cessation of ketamine use, with the addition of pentosan polysulfate, appeared to provide some symptomatic relief."[96]
The bladder symptoms are so severe amongst some recreational users that their bladders have had to be removed. In these cases neobladders have been created using sections of gut but there is a significant risk of similar damage occurring to the neobladder if ketamine use is not stopped.
Many long term users report "K-pains" or "ketamine cramps"[97]. The exact cause of these pains are unknown. The Ketamine induced abdominal pain is primarily limited to users of a gram or more of ketamine a day (route of administration does not seem to affect this symptom). It has been suggested that the amino acid Tyrosine may help alleviate the pain.[98]
In October 2009, Professor David Nutt, formerly of the British Home Office's Advisory Council on the Misuse of Drugs, recommended that ketamine be re-classed in the UK, as several patients who have used the drug recreationally had experienced bladder spasms and some have "irreversible bladder damage". Professor Nutt also reported that a small number of patients have had their bladder completely removed through ketamine abuse. The recommendation and case studies were featured heavily in the British press.[99]
See also
- Arylcyclohexylamine
- Esketamine
- Hallucinogen
- Dissociation
- Anesthesia
References
- ↑ Hijazi Y, Boulieu R (July 2002). "Contribution of CYP3A4, CYP2B6, and CYP2C9 isoforms to N-demethylation of ketamine in human liver microsomes". Drug Metabolism and Disposition 30 (7): 853–8. doi:10.1124/dmd.30.7.853. PMID 12065445.
- ↑ Harrison NL, Simmonds MA (February 1985). "Quantitative studies on some antagonists of N-methyl D-aspartate in slices of rat cerebral cortex". British Journal of Pharmacology 84 (2): 381–91. PMID 2858237.
- ↑ Hirota K, Sikand KS, Lambert DG (1999). "Interaction of ketamine with mu2 opioid receptors in SH-SY5Y human neuroblastoma cells". Journal of Anesthesia 13 (2): 107–9. doi:10.1007/s005400050035. PMID 14530949.
- ↑ Narita M, Yoshizawa K, Aoki K, Takagi M, Miyatake M, Suzuki T (September 2001). "A putative sigma1 receptor antagonist NE-100 attenuates the discriminative stimulus effects of ketamine in rats". Addiction Biology 6 (4): 373–376. doi:10.1080/13556210020077091. PMID 11900615.
- ↑ Bergman SA (1999). "Ketamine: review of its pharmacology and its use in pediatric anesthesia". Anesthesia Progress 46 (1): 10–20. PMID 10551055.
- ↑ Peck TE, Hill SA, Williams M (2008). Pharmacology for anaesthesia and intensive care (3rd edition). Cambridge: Cambridge university press. p. 111. ISBN 9780521704632.
- ↑ Nancy Diazgranados et al (August 2010). "A Randomized Add-on Trial of an N-methyl-D-aspartate Antagonist in Treatment-Resistant Bipolar Depression". Archives of General Psychiatry 67 (8): 793–802. doi:10.1001/archgenpsychiatry.2010.90.
- ↑ Krüger AD (1998). "[Current aspects of using ketamine in childhood]" (in German). Anaesthesiologie Und Reanimation 23 (3): 64–71. PMID 9707751.
- ↑ "WHO Model List of Essential Medicines" (PDF). World Health Organization. March 2005. http://whqlibdoc.who.int/hq/2005/a87017_eng.pdf. Retrieved 2006-03-12.
- ↑ Bonanno FG (May 2002). "Ketamine in war/tropical surgery (a final tribute to the racemic mixture)". Injury 33 (4): 323–7. doi:10.1016/S0020-1383(01)00209-1. PMID 12091028.
- ↑ Alltounian, Howard Sunny; Marcia Moore (1978). Journeys into the bright world. Rockport, Mass: Para Research. ISBN 0-914918-12-5.
- ↑ "Ketamine - Schedule III of The Controlled Substances Act (CSA)". Anestesiología Mexicana en Internet. http://www.anestesia.com.mx/articulo/keta.html. Retrieved 2006-12-22.
- ↑ "Club 'horse' drug to be outlawed". BBC News. 28 December 2005. http://news.bbc.co.uk/2/hi/uk_news/4564606.stm. Retrieved 7 May 2010.
- ↑ Controlled Drugs and Substances Act
- ↑ Government to tighten control on Ketamine
- ↑ Jansen, Karl (2001). Ketamine: Dreams and Realities. Multidisciplinary Association for Psychedelic Studies. p. 23. ISBN 0966001931.
- ↑ Jansen, Karl (2001). Ketamine: Dreams and Realities. Multidisciplinary Association for Psychedelic Studies. p. 38. ISBN 0966001931.
- ↑ Jansen, Karl (2001). Ketamine: Dreams and Realities. Multidisciplinary Association for Psychedelic Studies. p. 24. ISBN 0966001931.
- ↑ 19.0 19.1 Jansen, Karl (2001). Ketamine: Dreams and Realities. Multidisciplinary Association for Psychedelic Studies. p. 26. ISBN 0966001931.
- ↑ 20.0 20.1 Jansen, Karl (2001). Ketamine: Dreams and Realities. Multidisciplinary Association for Psychedelic Studies. p. 55. ISBN 0966001931.
- ↑ Cottingham R, Thomson K (September 1994). "Use of ketamine in prolonged entrapment". Journal of Accident & Emergency Medicine 11 (3): 189–91. doi:10.1136/emj.11.3.189. PMID 7804588.
- ↑ Lankenau SE, Sanders B, Bloom JJ, et al. (March 2007). "First injection of ketamine among young injection drug users (IDUs) in three U.S. cities". Drug and Alcohol Dependence 87 (2-3): 183–93. doi:10.1016/j.drugalcdep.2006.08.015. PMID 16979848.
- ↑ Reboso Morales JA, González Miranda F (March 1999). "[Ketamine]" (in Spanish). Revista Española de Anestesiología y Reanimación 46 (3): 111–22. PMID 10228376.
- ↑ Heshmati F, Zeinali MB, Noroozinia H, Abbacivash R, Mahoori A (December 2003). "Use of ketamine in severe status asthmaticus in intensive care unit". Iranian Journal of Allergy, Asthma, and Immunology 2 (4): 175–80. PMID 17301376.
- ↑ Krystal JH, Madonick S, Perry E, et al. (August 2006). "Potentiation of low dose ketamine effects by naltrexone: potential implications for the pharmacotherapy of alcoholism". Neuropsychopharmacology 31 (8): 1793–800. doi:10.1038/sj.npp.1300994. PMID 16395307.
- ↑ 26.0 26.1 Jovaisa T, Laurinenas G, Vosylius S, Sipylaite J, Badaras R, Ivaskevicius J (2006). "Effects of ketamine on precipitated opiate withdrawal". Medicina 42 (8): 625–34. PMID 16963828. http://medicina.kmu.lt/0608/0608-03e.htm.
- ↑ Lynch ME, Clark AJ, Sawynok J, Sullivan MJ (October 2005). "Topical amitriptyline and ketamine in neuropathic pain syndromes: an open-label study". The Journal of Pain 6 (10): 644–9. doi:10.1016/j.jpain.2005.04.008. PMID 16202956.
- ↑ 28.0 28.1 28.2 Elia N, Tramèr MR (January 2005). "Ketamine and postoperative pain--a quantitative systematic review of randomised trials". Pain 113 (1-2): 61–70. doi:10.1016/j.pain.2004.09.036. PMID 15621365.
- ↑ Saito O, Aoe T, Kozikowski A, Sarva J, Neale JH, Yamamoto T (September 2006). "Ketamine and N-acetylaspartylglutamate peptidase inhibitor exert analgesia in bone cancer pain". Canadian Journal of Anaesthesia 53 (9): 891–8. PMID 16960267.
- ↑ Adams HA (December 1997). "[S-(+)-ketamine. Circulatory interactions during total intravenous anesthesia and analgesia-sedation]" (in German). Der Anaesthesist 46 (12): 1081–7. doi:10.1007/s001010050510. PMID 9451493.
- ↑ Correll GE, Maleki J, Gracely EJ, Muir JJ, Harbut RE (September 2004). "Subanesthetic ketamine infusion therapy: a retrospective analysis of a novel therapeutic approach to complex regional pain syndrome". Pain Medicine 5 (3): 263–75. doi:10.1111/j.1526-4637.2004.04043.x. PMID 15367304.
- ↑ Blackwell Publishing (1 October 2004). "Severe Pain Relief may be Possible with a Common Anesthetic Drug". Press release. http://blackwellpublishing.com/press/pressitem.asp?ref=180. Retrieved 13 December 2009.
- ↑ Fujikawa DG (1995). "Neuroprotective Effect of Ketamine Administered After Status Epilepticus Onset". Epilepsia 36 (2): 186–195. doi:10.1111/j.1528-1157.1995.tb00979.x. PMID 7821277.
- ↑ Correll GE, Futter GE (2006). "Two case studies of patients with major depressive disorder given low-dose (subanesthetic) ketamine infusions". Pain Medicine 7 (1): 92–5. doi:10.1111/j.1526-4637.2006.00101.x. PMID 16533209.
- ↑ NIH. "Experimental Medication Kicks Depression in Hours Instead of Weeks" NIH News, 7 August 2006
- ↑ Khamsi, R. "Ketamine relieves depression within hours" New Scientist, 8 August 2006.
- ↑ Zarate CA, Singh JB, Carlson PJ, et al. (August 2006). "A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression". Archives of General Psychiatry 63 (8): 856–64. doi:10.1001/archpsyc.63.8.856. PMID 16894061.
- ↑ Berman RM, Cappiello A, Anand A, et al. (February 2000). "Antidepressant effects of ketamine in depressed patients". Biological Psychiatry 47 (4): 351–4. doi:10.1016/S0006-3223(99)00230-9. PMID 10686270.
- ↑ Liebrenz M, Borgeat A, Leisinger R, Stohler R (April 2007). "Intravenous ketamine therapy in a patient with a treatment-resistant major depression". Swiss Medical Weekly 137 (15-16): 234–6. PMID 17525879.
- ↑ Goforth HW, Holsinger T (March 2007). "Rapid relief of severe major depressive disorder by use of preoperative ketamine and electroconvulsive therapy". The Journal of ECT 23 (1): 23–5. doi:10.1097/01.yct.0000263257.44539.23. PMID 17435569.
- ↑ Faster-Acting Antidepressants Closer to Becoming a Reality", NIMH, 25 July 2007
- ↑ Krystal AD, Weiner RD, Dean MD, et al. (2003). "Comparison of seizure duration, ictal EEG, and cognitive effects of ketamine and methohexital anesthesia with ECT". The Journal of Neuropsychiatry and Clinical Neurosciences 15 (1): 27–34. PMID 12556568.
- ↑ Kudoh A, Takahira Y, Katagai H, Takazawa T (July 2002). "Small-dose ketamine improves the postoperative state of depressed patients". Anesthesia and Analgesia 95 (1): 114–8, table of contents. doi:10.1097/00000539-200207000-00020. PMID 12088953. http://www.anesthesia-analgesia.org/cgi/pmidlookup?view=long&pmid=12088953.
- ↑ Garcia LS, Comim CM, Valvassori SS, et al. (January 2008). "Acute administration of ketamine induces antidepressant-like effects in the forced swimming test and increases BDNF levels in the rat hippocampus". Progress in Neuro-psychopharmacology & Biological Psychiatry 32 (1): 140–4. doi:10.1016/j.pnpbp.2007.07.027. PMID 17884272.
- ↑ The Combination of Psychedelic and Aversive Approaches in Alcoholism Treatment - Eleusis
- ↑ Krupitsky EM, Grinenko AY (1997). "Ketamine psychedelic therapy (KPT): a review of the results of ten years of research". Journal of Psychoactive Drugs 29 (2): 165–83. PMID 9250944.
- ↑ http://www.eleusis.us/resource-center/references/ketamine-psychotherapy-heroin.pdf
- ↑ Krupitsky EM, Burakov AM, Dunaevsky IV, Romanova TN, Slavina TY, Grinenko AY (March 2007). "Single versus repeated sessions of ketamine-assisted psychotherapy for people with heroin dependence". Journal of Psychoactive Drugs 39 (1): 13–9. PMID 17523581.
- ↑ Krupitsky; Kolp. "Ketamine Psychedelic Psychotherapy". In Michael J. Winkelman and Thomas B., Roberts. Psychedelic Medicine: New Evidence for Hallucinogens as Treatments. Westport, CT: Praeger/Greenwood.
- ↑ 50.0 50.1 Goldberg ME, Domsky R, Scaringe D, et al. (April 2005). "Multi-day low dose ketamine infusion for the treatment of complex regional pain syndrome". Pain Physician 8 (2): 175–9. PMID 16850072. http://www.painphysicianjournal.com/linkout_vw.php?issn=1533-3159&vol=8&page=175.
- ↑ 51.0 51.1 CNN report on ketamine therapy for CRPS/RSD 1 September 2006
- ↑ Kiefer RT, Rohr P, Ploppa A, Altemeyer KH, Schwartzman RJ (June 2007). "Complete recovery from intractable complex regional pain syndrome, CRPS-type I, following anesthetic ketamine and midazolam". Pain Practice 7 (2): 147–50. doi:10.1111/j.1533-2500.2007.00123.x. PMID 17559485.
- ↑ Lundberg GD (2008). "Postoperative Ketamine Can Reduce Morphine Consumption and Nausea". The Medscape Journal of Medicine 10 (10): 234.
- ↑ De Reuck J, Decoo D, Strijckmans K, Lemahieu I (1992). "Does the severity of leukoaraiosis contribute to senile dementia? A comparative computerized and positron emission tomographic study". European Neurology 32 (4): 199–205. doi:10.1017/S0265021504003059. PMID 1505589.
- ↑ Fort Dodge (division of Wyeth) Ketamine Lable. Article retrieved on 1 November 2008
- ↑ Radovanović D, Pjević M (2003). "[Ketamine: the past 30 years and its future]". Medicinski Pregled 56 (9-10): 439–45. doi:10.2298/MPNS0310439R. PMID 14740534.
- ↑ 57.0 57.1 Sinner B, Graf BM (2008). "Ketamine". Handbook of Experimental Pharmacology 182 (182): 313–33. doi:10.1007/978-3-540-74806-9_15. PMID 18175098.
- ↑ Kelland MD, Soltis RP, Boldry RC, Walters JR (September 1993). "Behavioral and electrophysiological comparison of ketamine with dizocilpine in the rat". Physiology & Behavior 54 (3): 547–54. doi:10.1016/0031-9384(93)90248-E. PMID 8415949.
- ↑ Chen X, Shu S, Bayliss DA (January 2009). "HCN1 channel subunits are a molecular substrate for hypnotic actions of ketamine". J. Neurosci. 29 (3): 600–9. doi:10.1523/JNEUROSCI.3481-08.2009. PMID 19158287.
- ↑ 60.0 60.1 Chen X, Sirois JE, Lei Q, Talley EM, Lynch C, Bayliss DA (June 2005). "HCN subunit-specific and cAMP-modulated effects of anesthetics on neuronal pacemaker currents". The Journal of Neuroscience 25 (24): 5803–14. doi:10.1523/JNEUROSCI.1153-05.2005. PMID 15958747.
- ↑ Carr DB, Andrews GD, Glen WB, Lavin A (October 2007). "alpha2-Noradrenergic receptors activation enhances excitability and synaptic integration in rat prefrontal cortex pyramidal neurons via inhibition of HCN currents". The Journal of Physiology 584 (2): 437–50. doi:10.1113/jphysiol.2007.141671. PMID 17702809.
- ↑ Lipton SA (February 2006). "Paradigm shift in neuroprotection by NMDA receptor blockade: memantine and beyond". Nature Reviews. Drug Discovery 5 (2): 160–70. doi:10.1038/nrd1958. PMID 16424917.
- ↑ Seeman P, Guan HC, Hirbec H (August 2009). "Dopamine D2High receptors stimulated by phencyclidines, lysergic acid diethylamide, salvinorin A, and modafinil". Synapse (New York, N.Y.) 63 (8): 698–704. doi:10.1002/syn.20647. PMID 19391150.
- ↑ Coates KM, Flood P (October 2001). "Ketamine and its preservative, benzethonium chloride, both inhibit human recombinant alpha7 and alpha4beta2 neuronal nicotinic acetylcholine receptors in Xenopus oocytes". British Journal of Pharmacology 134 (4): 871–9. doi:10.1038/sj.bjp.0704315. PMID 11606328.
- ↑ Togal T, Demirbilek S, Koroglu A, Yapici E, Ersoy O (March 2004). "Effects of S(+) ketamine added to bupivacaine for spinal anaesthesia for prostate surgery in elderly patients". European Journal of Anaesthesiology 21 (3): 193–7. PMID 15055891.
- ↑ Benoit E (January 1995). "Effects of intravenous anaesthetics on nerve axons". European Journal of Anaesthesiology 12 (1): 59–70. PMID 7705328.
- ↑ Wagner LE, Gingrich KJ, Kulli JC, Yang J (December 2001). "Ketamine blockade of voltage-gated sodium channels: evidence for a shared receptor site with local anesthetics". Anesthesiology 95 (6): 1406–13. PMID 11748399. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0003-3022&volume=95&issue=6&spage=1406.
- ↑ Shibuta S, Varathan S, Mashimo T (October 2006). "Ketamine and thiopental sodium: individual and combined neuroprotective effects on cortical cultures exposed to NMDA or nitric oxide". British Journal of Anaesthesia 97 (4): 517–24. doi:10.1093/bja/ael192. PMID 16928698.
- ↑ 69.0 69.1 "SI.com - The Mexican Connection - Jul 18, 2007". CNN. http://sportsillustrated.cnn.com/2007/more/07/18/steroids0424/1.html. Retrieved 7 May 2010.
- ↑ Untitled-59
- ↑ ABC News: Ketamine, a Tranquilizer and Popular Club Drug, May Work for Depression
- ↑ Saunders N, Heron L (1993). E for Ecstasy. London: N. Saunders. ISBN 0950162884.
- ↑ See: [1] for details online.
- ↑ Doward, Jamie (1 November 2009). "Ministers face rebellion over drug tsar's sacking | Politics | The Observer". London: Guardian. http://www.guardian.co.uk/politics/2009/nov/01/david-nutt-gordon-brown-drugs. Retrieved 2010-01-22.
- ↑ Erowid Ketamine Vault: Dosage
- ↑ Feng N, Vollenweider FX, Minder EI, Rentsch K, Grampp T, Vonderschmitt DJ. Development of a gas chromatography-mass spectrometry method for determination of ketamine in plasma and its application to human samples. Ther. Drug Monit. 17: 95-100, 1995.
- ↑ Parkin MC, Turfus SC, Smith NW, Halket JM, Braithwaite RA, Elliott SP, Osselton MD, Cowan DA, Kicman AT. Detection of ketamine and its metabolites in urine by ultra high pressure liquid chromatography-tandem mass spectrometry. J. Chrom. B 876: 137-142, 2008.
- ↑ R. Baselt, Disposition of Toxic Drugs and Chemicals in Man, 8th edition, Biomedical Publications, Foster City, CA, 2008, pp. 806-808.
- ↑ Giannini AJ, Loiselle RH, Giannini MC, Price WA (1985). "Phencyclidine and the dissociatives". Psychiatric Medicine 3 (3): 197–217. PMID 2893430.
- ↑ AJ Giannini,RH Loisellle, MC Giannini, WA Price, 1987, op. cit. The dissociatives. Medical Psychiatry. 3(3):197-205, 1987
- ↑ Giannini AJ, Underwood NA, Condon M (November 2000). "Acute ketamine intoxication treated by haloperidol: a preliminary study". American Journal of Therapeutics 7 (6): 389–91. doi:10.1097/00045391-200007060-00008. PMID 11304647.
- ↑ Giannini AJ (1999). Drug Abuse. Los Angeles: Health Information Press. pp. 104. ISBN 1-885987-11-0.
- ↑ Lilly, John Cunningham (1997). The scientist: a metaphysical autobiography. Berkeley, CA: Ronin Pub. ISBN 0-914171-72-0.
- ↑ Alltounian, Howard Sunny; Marcia Moore (1978). Journeys into the bright world. Rockport, Mass: Para Research. ISBN 978-0-914918-12-7.
- ↑ Turner, D. M. (1994). The essential psychedelic guide. San Francisco, CA: Panther Press. ISBN 0-9642636-1-0.
- ↑ Jansen, Karl (2001). Ketamine: Dreams and Realities. Multidisciplinary Association for Psychedelic Studies. p. 50. ISBN 0966001931.
- ↑ Jansen, Karl (2001). Ketamine: Dreams and Realities. Multidisciplinary Association for Psychedelic Studies. p. 89. ISBN 0966001931.
- ↑ Okon T (May 2007). "Ketamine: an introduction for the pain and palliative medicine physician". Pain Physician 10 (3): 493–500. PMID 17525784. http://www.painphysicianjournal.com/linkout_vw.php?issn=1533-3159&vol=10&page=493.
- ↑ Olney JW, Labruyere J, Price MT (June 1989). "Pathological changes induced in cerebrocortical neurons by phencyclidine and related drugs". Science 244 (4910): 1360–2. doi:10.1126/science.2660263. PMID 2660263.
- ↑ 90.0 90.1 Erowid DXM Vaults: Health: The Bad News Isn't In: A Look at Dissociative-Induced Brain Damage, by Anderson C
- ↑ 91.0 91.1 Tryba M, Gehling M (October 2002). "Clonidine--a potent analgesic adjuvant". Current Opinion in Anaesthesiology 15 (5): 511–7. doi:10.1097/00001503-200210000-00007. PMID 17019247. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0952-7907&volume=15&issue=5&spage=511.
- ↑ Morgan, Celia J. A.; Muetzelfeldt, Leslie; Curran, H. Valerie (2009). "Consequences of chronic ketamine self-administration upon neurocognitive function and psychological wellbeing: a 1-year longitudinal study". Addiction 105 (1): 121. doi:10.1111/j.1360-0443.2009.02761.x. PMID 19919593.
- ↑ Hargreaves RJ, Hill RG, Iversen LL (1994). "Neuroprotective NMDA antagonists: the controversy over their potential for adverse effects on cortical neuronal morphology". Acta Neurochirurgica. Supplementum 60: 15–9. PMID 7976530.
- ↑ AJ Giannini, N Underwood, M Condon op. cit.
- ↑ Cottrell, A. M; Athreeres, R.; Weinstock, P.; Warren, K.; Gillatt, D. (2008). "Urinary tract disease associated with chronic ketamine use". BMJ 336: 973. doi:10.1136/bmj.39562.711713.80.
- ↑ Shahani R, Streutker C, Dickson B, Stewart RJ (May 2007). "Ketamine-associated ulcerative cystitis: a new clinical entity". Urology 69 (5): 810–2. doi:10.1016/j.urology.2007.01.038. PMID 17482909.
- ↑ Middleton, Duncan (15 January 2009). "Warning over rising ketamine use". BBC. http://news.bbc.co.uk/newsbeat/hi/health/newsid_7831000/7831301.stm. Retrieved 19 January 2010.
- ↑ Jansen, Karl (2001). Ketamine: Dreams and Realities. Multidisciplinary Association for Psychedelic Studies. p. 271. ISBN 0966001931.
- ↑ "Ketamine link to bladder failure". BBC News. 4 February 2009. http://news.bbc.co.uk/1/hi/england/bristol/7867449.stm. Retrieved 15 January 2010.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
