Imatinib
 |
|
|---|---|
| Systematic (IUPAC) name | |
| 4-[(4-methylpiperazin-1-yl)methyl]-N-[4-methyl-3-[(4-pyridin-3-ylpyrimidin-2-yl)amino]phenyl]benzamide | |
| Identifiers | |
| CAS number | 152459-95-5 220127-57-1 (mesilate) |
| ATC code | L01XE01 |
| PubChem | CID 5291 |
| DrugBank | APRD01028 |
| ChemSpider | 5101 |
| Chemical data | |
| Formula | C29H31N7O |
| Mol. mass | 493.603 g/mol 589.7 g/mol (mesilate) |
| SMILES | eMolecules & PubChem |
| Pharmacokinetic data | |
| Bioavailability | 98% |
| Protein binding | 95% |
| Metabolism | Hepatic (mainly CYP3A4-mediated) |
| Half-life | 18 hours (imatinib) 40 hours (active metabolite) |
| Excretion | Fecal (68%) and renal (13%) |
| Therapeutic considerations | |
| Licence data | EMA:Link, US FDA:link |
| Pregnancy cat. | D(AU) D(US) |
| Legal status | POM (UK) ℞-only (US) |
| Routes | Oral |
| |
|
Imatinib is a drug used to treat certain types of cancer. It is currently marketed by Novartis as Gleevec (USA) or Glivec (Europe/Australia/Latin America) as its mesylate salt, imatinib mesilate (INN). It is used in treating chronic myelogenous leukemia (CML), gastrointestinal stromal tumors (GISTs) and other cancers.
It is the first member of a new class of agents that act by specifically inhibiting a certain enzyme that is characteristic of a particular cancer cell, rather than non-specifically inhibiting and killing all rapidly dividing cells.
In CML, the tyrosine kinase enzyme ABL is stuck in the "on" position. Imatinib binds to the site of tyrosine kinase activity, and prevents its activity.
Contents |
History
Imatinib was developed in the late 1990s by biochemist Nicholas Lydon, a former researcher for Novartis, and oncologist Brian Druker of Oregon Health and Science University (OHSU). Other major contributions to imatinib development were made by Carlo Gambacorti-Passerini, a physician scientist at University of Milano Bicocca(http://www.unimib.it), Italy, John Goldman at Royal Hammersmith Hospital in London, UK, and Charles Sawyers of Memorial Sloan-Kettering Cancer Center,[1] who led the clinical trials confirming its efficacy in CML.
Imatinib was developed by rational drug design. After the Philadelphia chromosome mutation and defective bcr-abl protein were discovered, the investigators screened chemical libraries to find a drug that would inhibit that protein. With high-throughput screening, they identified 2-phenylaminopyrimidine. This lead compound was then tested and modified by the introduction of methyl and benzamide groups to give it enhanced binding properties, resulting in imatinib.[2]
Gleevec received FDA approval in May 2001. On the same month it made the cover of TIME magazine as the "magic bullet" to cure cancer.
Druker, Lydon and Sawyers received the Lasker-DeBakey Clinical Medical Research Award in 2009 for "converting a fatal cancer into a manageable chronic condition".[1]
Uses
Imatinib is used in chronic myelogenous leukemia (CML), gastrointestinal stromal tumors (GISTs) and a number of other malignancies. One study demonstrated that Imatinib mesylate was effective in patients with systemic mastocytosis, including those who had the D816V mutation in c-Kit.[3] Experience has shown, however, that imatinib is much less effective in patients with this mutation, and patients with the mutation comprise nearly 90% of cases of mastocytosis. Early clinical trials also show its potential for treatment of hypereosinophilic syndrome and dermatofibrosarcoma protuberans.
Imatinib may also have a role in the treatment of pulmonary hypertension. It has been shown to reduce both the smooth muscle hypertrophy and hyperplasia of the pulmonary vasculature in a variety of disease processes, including portopulmonary hypertension. [4]
In laboratory settings, imatinib is being used as an experimental agent to suppress platelet-derived growth factor (PDGF) by inhibiting its receptor (PDGF-Rβ). One of its effects is delaying atherosclerosis in mice without[5] or with diabetes.[6]
Recent mouse animal studies at Emory University in Atlanta have suggested that imatinib and related drugs may be useful in treating smallpox, should an outbreak ever occur.[7]
Tolerability and adverse effects

In the United States, the Food and Drug Administration has approved imatinib as first-line treatment for CML.[8] Imatinib has passed through Phase III trials for CML, and has been shown to be more effective than the previous standard treatment of α-interferon and cytarabine. Although the long-term side effects of imatinib have not yet been ascertained, research suggests that it is generally very well tolerated. Broadly, side effects such as edema, nausea, rash and musculoskeletal pain are common but mild.
Severe congestive cardiac failure is an uncommon but recognized side effect of imatinib and mice treated with large doses of imatinib show toxic damage to their myocardium.[9]
Pharmacology
Pharmacokinetics
Imatinib is rapidly absorbed when given by mouth, and is highly bioavailable: 98% of an oral dose reaches the bloodstream. Metabolism of imatinib occurs in the liver and is mediated by several isozymes of the cytochrome P450 system, including CYP3A4 and, to a lesser extent, CYP1A2, CYP2D6, CYP2C9, and CYP2C19. The main metabolite, N-demethylated piperazine derivative, is also active. The major route of elimination is in the bile and feces; only a small portion of the drug is excreted in the urine. Most of imatinib is eliminated as metabolites, only 25% is eliminated unchanged. The half-lives of imatinib and its main metabolite are 18 and 40 hours, respectively.It blocks the activity of Abelson cytoplasmic tyrosine kinase (ABL), c-Kit and the platelet-derived growth factor receptor (PDGFR). As an inhibitor of PDGFR, imatinib mesylate appears to have utility in the treatment of a variety of dermatological diseases. Imatinib has been reported to be an effective treatment for FIP1L1-PDGFRalpha+ mast cell disease, hypereosinophilic syndrome, and dermatofibrosarcoma protuberans.[10]
Mechanism of action
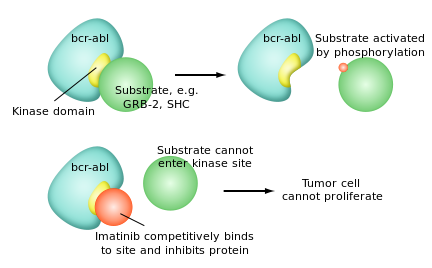
Imatinib is a 2-phenylaminopyrimidine derivative that functions as a specific inhibitor of a number of tyrosine kinase enzymes. It occupies the TK active site, leading to a decrease in activity.
There are a large number of TK enzymes in the body, including the insulin receptor. Imatinib is specific for the TK domain in abl (the Abelson proto-oncogene), c-kit and PDGF-R (platelet-derived growth factor receptor).
In chronic myelogenous leukemia, the Philadelphia chromosome leads to a fusion protein of abl with bcr (breakpoint cluster region), termed bcr-abl. As this is now a constitutively active tyrosine kinase, imatinib is used to decrease bcr-abl activity.
The active sites of tyrosine kinases each have a binding site for ATP. The enzymatic activity catalyzed by a tyrosine kinase is the transfer of the terminal phosphate from ATP to tyrosine residues on its substrates, a process known as protein tyrosine phosphorylation. Imatinib works by binding close to the ATP binding site of bcr-abl, locking it in a closed or self-inhibited conformation, and therefore inhibiting the enzyme activity of the protein semi-competitively.[11] This fact explains why many BCR-ABL mutations can cause resistance to imatinib by shifting its equilibrium toward the open or active conformation.[12]
Imatinib is quite selective for bcr-abl – it does also inhibit other targets mentioned above (c-kit and PDGF-R), but no other known tyrosine kinases. Imatinib also inhibits the abl protein of non-cancer cells but cells normally have additional redundant tyrosine kinases which allow them to continue to function even if abl tyrosine kinase is inhibited. Some tumor cells, however, have a dependence on bcr-abl.[8] Inhibition of the bcr-abl tyrosine kinase also stimulates its entry in to the nucleus, where it is unable to perform any of its normal anti-apoptopic functions.[13]
Costs

The cost of Gleevec for CML is $32,000[14][15] to $98,000[16] a year, and for GIST is $64,800 a year.[17] As a result, many patients have stopped taking it even though their disease will recur. Gleevec is often cited as an example of pharmaceutical industry innovation that justifies the high cost of drugs. Marcia Angell and Arnold S. Relman argue that Gleevec is actually an example of the contribution of taxpayer-supported research and of industry inaction. Druker tested several drugs, imatinib was the most potent, and unusually, had almost no effect on normal cells. Novartis had "little corporate enthusiasm," they write, but Druker persisted.[18] Druker has complained that he is disappointed with the high price of Gleevec.
Prices for a 100 mg pill of Gleevec internationally range from $20 to $30[19], although generic imatinib is cheaper.[20]
In 2007, imatinib became a test case through which Novartis challenged India's patent laws. A win for Novartis would make it harder for Indian companies to produce generic versions of drugs still manufactured under patent elsewhere in the world. Médecins Sans Frontières argues that a change in law would make it impossible for Indian companies to produce cheap generic antiretrovirals (anti-HIV medication), thus making it impossible for Third World countries to buy these essential medicines.[21] On 6 August 2007 the Madras High Court, dismissed the writ petition filed by Novartis, challenging the constitutionality of Section 3(d) of Indian Patent Act and deferred to the World Trade Organization (WTO) forum to resolve the TRIPS compliance question.
See also
- History of cancer chemotherapy
References
- ↑ 1.0 1.1 A Conversation With Brian J. Druker, M.D., Researcher Behind the Drug Gleevec by Claudia Dreifus, The New York Times, November 2, 2009
- ↑ Druker BJ, Lydon NB. Lessons learned from the development of an Abl tyrosine kinase inhibitor for chronic myelogenous leukemia. J Clin Invest 2000;105:3-7. PMID 10619854
- ↑ Droogendijk HJ, Kluin-Nelemans HJ, van Doormaal JJ, Oranje AP, van de Loosdrecht AA, van Daele PL. Imatinib mesylate in the treatment of systemic mastocytosis: a phase II trial. Cancer. 2006 Jul 15;107(2):345-51. PMID 16779792
- ↑ Tapper EB, Knowles D, Heffron T, Lawrence EC, Csete M. Portopulmonary hypertension: imatinib as a novel treatment and the emory experience with this condition. Transplant Proc. 2009 Jun;41(5):1969-71.
- ↑ Philippe Boucher, Michael Gotthardt, Wei-Ping Li, Richard G.W. Anderson, Joachim Herz (2003). LRP: Role in Vascular Wall Integrity and Protection from Atherosclerosis. Science 300, 329-332. PMID 12690199
- ↑ Lassila M, Allen TJ, Cao Z, Thallas V, Jandeleit-Dahm KA, Candido R, Cooper ME. Imatinib attenuates diabetes-associated atherosclerosis. Arterioscler Thromb Vasc Biol 2004;24:935-42. PMID 14988091
- ↑ Reeves P, Bommarius B, Lebeis S, McNulty S, Christensen J, Swimm A, Chahroudi A, Chavan R, Feinberg M, Veach D, Bornmann W, Sherman M, Kalman D (2005). Disabling poxvirus pathogenesis by inhibition of Abl-family tyrosine kinases. Nat Med 11 (7): 731-9. PMID 15980865
- ↑ 8.0 8.1 Deininger M, Druker BJ. Specific Targeted Therapy of Chronic Myelogenous Leukemia with Imatinib. Pharmacol Rev 2003;55:401-423. PMID 12869662.
- ↑ Risto Kerkelä, Luanda Grazette, Rinat Yacobi, et al.. "Cardiotoxicity of the cancer therapeutic agent imatinib mesylate". Nature Med 12: 908–16.
- ↑ Scheinfeld NS. A comprehensive review of imatinib mesylate (Gleevac) for dermatological disease. J Drug Dermatol. 5:18-23;2006. PMID 16485879
- ↑ Takimoto CH, Calvo E. "Principles of Oncologic Pharmacotherapy" in Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ (Eds) Cancer Management: A Multidisciplinary Approach. 11 ed. 2008.
- ↑ C Gambacorti-Passerini, R Gunby, R Piazza, A Galietta, R Rostagno, L Scapozza. Molecular mechanisms of resistance to imatinib in Ph-positive leukemias. Lancet Oncology, 2003:4:75-85. PMID 12573349
- ↑ Vigneri P, Wang JY. Induction of apoptosis in chronic myelogenous leukemia cells through nuclear entrapment of BCR-ABL tyrosine kinase. Nat Med 2001:7:228-234. PMID 11175855
- ↑ BCR-ABL Tyrosine Kinase Inhibitors for Chronic Myelogenous Leukemia, Charles A. Schiffer, N Engl J Med 2007; 357:258-265July 19, 2007
- ↑ As Pills Treat Cancer, Insurance Lags Behind, By ANDREW POLLACK, New York Times, April 14, 2009
- ↑ Living With a Formerly fatal Blood Cancer, By JANE E. BRODY, New York Times, January 18, 2010
- ↑ Nonadherence to Imatinib during an Economic Downturn, Letters, Robin K. Kelley and Alan P. Venook, N Engl J Med 2010; 363:596-598, August 5, 2010
- ↑ [1] How the drug industry distorts medicine and politics: America’s Other Drug Problem, By Arnold S. Relman and Marcia Angell, New Republic, December 16, 2002
- ↑ Patented Medicine Review Board (Canada). Report on New Patented Drugs - Gleevec.
- ↑ pharmacychecker.com
- ↑ Médecins Sans Frontières. "As Novartis Challenges India's Patent Law, MSF Warns Access to Medicines Is Under Threat", 2006-09-26. Accessed 2006-02-10.
External links
|
|||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||